Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.12 no.4 Piracicaba Out./Dez. 2013
ORIGINAL ARTICLE
Use of etoricoxib and dexamethasone for postoperative pain prevention and control in mucogingival surgery - A randomized parallel double-blind clinical trial
Ligia Nadal ZardoI; Fábio André dos SantosI; Gibson Luiz PilattiI
I Department of Periodontology, Dental School, State University of Ponta Grossa, Ponta Grossa, PR, Brazil
ABSTRACT
AIM: To compare the use of etoricoxib and dexamethasone for postoperative pain prevention and control after mucogingival surgery. METHODS: Fifty-eight patients with indication for mucogingival surgery took part in this randomized parallel double-blind clinical trial. They were divided into three groups (G): G1 – placebo 1 h before surgery; G2 – 8 mg dexamethasone 1 h before surgery; G3 – 90 mg etoricoxib 1 h before surgery. Pain intensity was assessed in donor and recipient sites separately using the 101-point numerical rating scale NRS – 101, every hour for the first 8 h after surgery and three times a day on the following 3 days. RESULTS: there was a statistically significant difference in the postoperative pain intensity in the donor site between G1 and G3 after 1 h, 2 h, 3 h, 7 h, 8 h and on the second day – in the evening after 32 h; between G1 and G2 after 2 h and 3 h, and between G2 and G3 only after the first hour. Pain intensity in the recipient site was statistically significant between G1 and G3 after 1 and 2 h (p<0.05). In addition, there was a lower ingestion of rescue medication in G2 and in G3 than in G1 (p=0.002). CONCLUSIONS: the use of a pre-emptive single dose of etoricoxib or dexamethasone may be considered an effective protocol for postoperative pain prevention and control after mucogingival surgery.
Keywords: analgesia; pain, postoperative; surgery, oral.
Introduction
Periodontal surgical procedures, such as soft tissue grafts (mucogingival surgeries) or those involving bone resection may have a significant expectation of pain and edema for patients after surgery1,2.
Soft tissue grafts are autogenous grafts from masticatory mucosa completely detached from their original site and placed in a prepared recipient bed3. The so called "free gingival graft" has been widely used to increase the width of the keratinised tissue and to treat gingival recessions4,5. The predictability of root coverage procedures was dramatically increased by the use of subepithelial connective tissue graft techniques6.
Pain following periodontal surgery results from a cascade of events during the inflammatory response triggered by a surgical tissue trauma. To prevent or minimize these effects preemptive analgesia has been used, which consists in the use of a drug regimen prior to nociceptive stimuli in order to prevent hyperalgesia and subsequent pain amplification7,8.
The search for drug protocols that provide adequate analgesia and comfort for the patient in the postoperative period has been highlighted in the literature9-14.
A few trials15,16 suggested that preoperative administration of different anti-inflammatory drugs reduced postoperative pain intensity and the need for supplementary analgesics. Several pre- and postoperative medication protocols have been used to minimize postoperative pain after third molars extraction9,17-20, endodontic surgery21 and periodontal surgical treatment2,10,12,14,22.
Etoricoxib is considered a non-steroidal anti-inflammatory drug (NSAID) that selectively inhibits COX-2, predominantly produced during inflammation, thereby inhibiting prostaglandin production and release. It is rapidly absorbed and reaches optimum plasma levels 1 h after administration. It has an elimination half-life of approximately 25 h23.
The inhibition of COX-2 by NSAID does not prevent the formation of leukotrienes, which also promote sensitization of nociceptors and result in pain and edema. Corticosteroids are steroidal anti-inflammatory drugs (SAID) which suppress inflammation by several mechanisms. They interact with specific intracellular receptor proteins in the target tissues and alter the expression of genes to corticosteroids. Specific steroid receptors in the cell cytoplasm bind to ligands for steroid hormone-receptor complexes that occsionally translocate to the cell nucleus. In the nucleus, these complexes bind to specific DNA sequences and alter their expression. The complexes may induce transcription of messenger RNA, leading to the synthesis of new proteins. Among these proteins, annexin is known to inhibit phospholipase A2 and thus block the production of mediators and arachidonic acid metabolites such as the COX-2 enzyme, leukotrienes and prostaglandins, cytokines, interleukins, adhesion molecules and enzymes such as collagenase24,25.
Dexamethasone is a SAID that inhibits phospholipase A2, affects the prostaglandins and leukotrienes synthesis, reducing polymorphonuclear leukocytes chemotaxis. Furthermore, SAIDs are able to down-regulate many proinflammatory cytokines such as Interleukin 1â, -6, -8, -12 and -18, and alpha tumor necrosis factor, involved in inflammation and immune response. It has a half-life (t 1/2) of approximately 3 h and an apparent distribution volume (Vd) of 1.0 L/kg24.
There are no published studies comparing the use of dexamethasone and etoricoxib before mucogingival surgery. The hypothesis to be tested is whether there is any difference in the intensity of postoperative pain in patients undergoing mucogingival surgery after different protocols of preemptive analgesia with anti-inflammatory drugs administered in a single preoperative dose.
Material and methods
Sixty patients referred for periodontal therapy in the Dental School of Ponta Grossa State University took part in this study, from March 2010 to November 2011. This was a randomized double-blind parallel trial, which included patients of both genders, aged 19 to 67 (mean=36.56 ± SD=9.57) who had at least one area with mucogingival surgery indication of epithelized soft tissue graft or subepithelial connective tissue, such as a narrow width of keratinized tissue, labial frenum with an insertion close to the gingival margin associated with a shallow depth of the vestibule, and class I and II gingival recessions in an aesthetic area.
Patients with untreated periodontal disease, poor oral hygiene, history of systemic diseases, pregnant and lactating women, allergy to any of the involved medications, patients making long term use of analgesics and/or anti-inflammatory drugs or at risk of infective endocarditis were excluded from the study. The nature of the study was previously explained to each patient, who signed an informed consent form approved by the University's Institutional Ethical Committee on Human Research (protocol 16/2011). The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2000.
Each patient received a different preoperative medication, one hour before surgery: Group 1 received a placebo capsule (n=20); Group 2 received two 4-mg tablets of dexamethasone (n=20) and Group 3 received one 90-mg tablet of etoricoxib (n=20). Both the surgeon and the patient had no knowledge of the drug that was used in the trial.
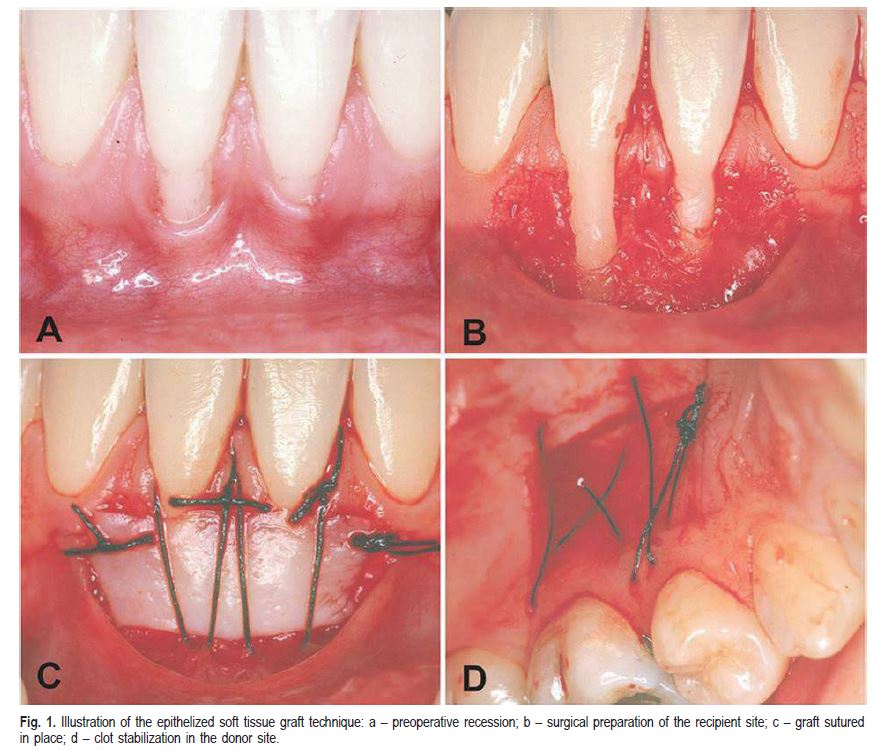
The mucogingival surgeries were performed by an experienced periodontist (LNZ) following all preoperative care to avoid cross-infection. Patients scheduled to receive an epithelized soft tissue graft received local buccal (1.8 mL) and palatal (0.3-0.4 mL) terminal infiltration anesthesia of 2% lidocaine with 1:100,000 epinephrine (DFL, Rio de Janeiro, RJ, Brazil). The recipient site was dissected by an incision with a 15C blade, parallel to the mucogingival junction, removing the epithelium and part of the underlying connective tissue, and exposing the periosteum around the affected teeth. A soft tissue graft consisting of epithelium and connective tissue was gently removed from the palate, adapted and sutured to the recipient site with a 5.0 nylon suture and a non-traumatic needle (Figure 1).
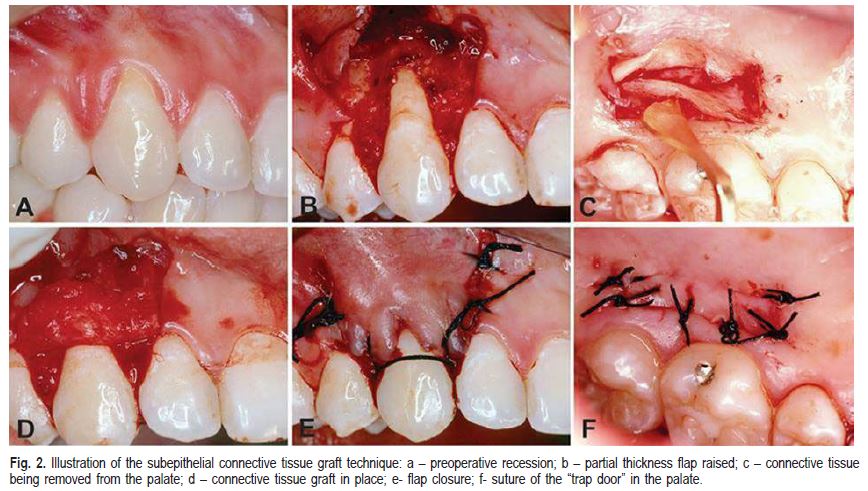
Patients who underwent the subepithelial connective tissue graft surgery were anesthetized by the same technique using 2% lidocaine with 1:100,000 epinephrine. The exposed root surface was scaled and planed with 5-6 Gracey curettes. Two vertical diverging incisions were made laterally from the gingival resection. An intrasulcular incision was made preserving the gingival papillae. A partial thickness flap was raised and the epithelium of the gingival papillae was removed. The graft was taken from the palate using a "trap door" technique and placed on the exposed roots and sutured using resorbable 5.0 Vicryl sutures (Ethicon, Inc., São José dos Campos, SP, Brazil). The flap was coronally positioned and sutured with 5.0 nylon interrupted sutures (Figure 2).
All patients received six 750-mg pills of paracetamol (Medley, São Paulo, SP, Brazil) to be used as a rescue medication every 6 h in case of pain, writing down on a form each time the medication was used. One day after surgery,the patients were instructed to use 0.12% chlorhexidine gluconate (Periogard; Colgate-Palmolive, São Bernardo do Campo, SP, Brazil) as a 15 mL mouthwash for 1 min, every 12 h for 15 days.
The time (in min) for performing the surgery and the size of the graft taken from the palate, measured with a periodontal probe (mm2) were recorded on the patient's file.
Postoperative pain intensity was recorded separately for the donor and the recipient site by the patient on a paper form every hour for the first eight hours after surgery and three times a day during the next three days. The 101-points numerical rating scale (NRS-101) was used, which consists of assigning a pain score from 0 (no pain) to 100 (pain as bad as it could be).
Statistical Analysis
The power calculation was performed using data previously published by the authors12. When the sample size in each of the three groups was 18, a two-sided test would have 82% power at an effect size of 0.45 and a 0.05 level. These calculations were made using specific software (G*Power 3 – http://www.psycho.uni-duesseldorf.de/ abteilungen/aap/gpower3/). Duration of the surgery, size of the graft (independent variables), NRS-101 scores for the donor and the recipient sites and rescue medication consumption (dependent variables) did not fit the Gauss normal distribution curve nor showed homoscedasticity among variances, even when data were transformed. Therefore, non-parametric Kruskal- Wallis test was used to compare the three groups. In case of any differences among the groups, pairs using the Mann- Whitney post hoc test. Pain scores for the donor and the recipient sites were analyzed separately at each time period. For all tests a 0.05 level of significance was used. All tests were performed using SPSS for Windows version 13.0 (SPSS 13.0 for Windows; SPSS, Chicago, IL, USA).
Results
Fifty-eight from the 60 patients initially enrolled completed the study. Two patients did not return the form with the pain scores. No side effects were reported for any used medication.
There was no statistically significant difference among the groups concerning the size of the graft (placebo- 56.9±10.0 mm2, dexamethasone-53.5±12.6 mm2 and etoricoxib-58.3±11.6 mm2 - p=0.36). The duration of the surgery in the placebo group (50.25±7.1) was shorter than in the other groups (dexamethasone-56.8±6.7; etoricoxib- 56.0±8.9 - p=0.015).
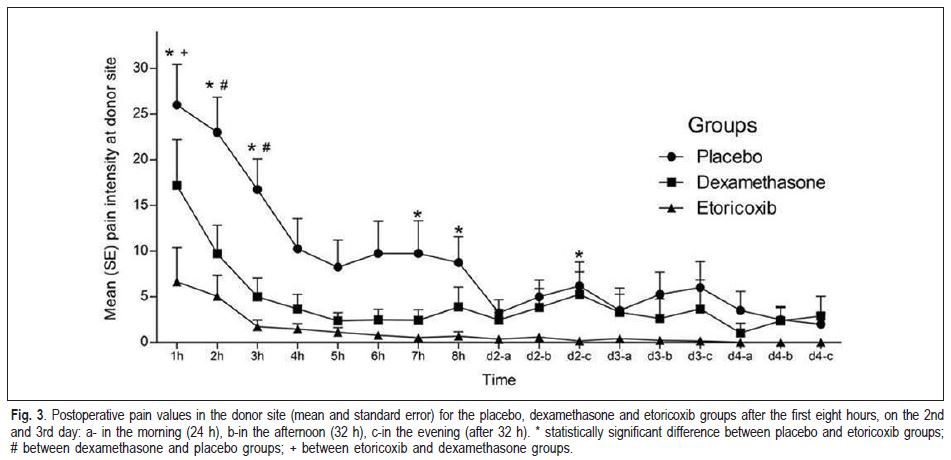
The mean and standard error for postoperative pain intensity in the donor site for the placebo, etoricoxib and dexamethasone groups are shown in Figure 3. There was a statistically significant difference between the placebo and the etoricoxib groups at 1 h, 2 h, 3 h, 7 h, 8 h and on the second day in the evening (p<0.05). Postoperative pain intensity in the dexamethasone group was statistically lower than in the placebo group at 2 h and 3 h periods. Finally, the etoricoxib group demonstrated statistically significant lower postoperative pain scores than the dexamethasone group only at the 1 h period.
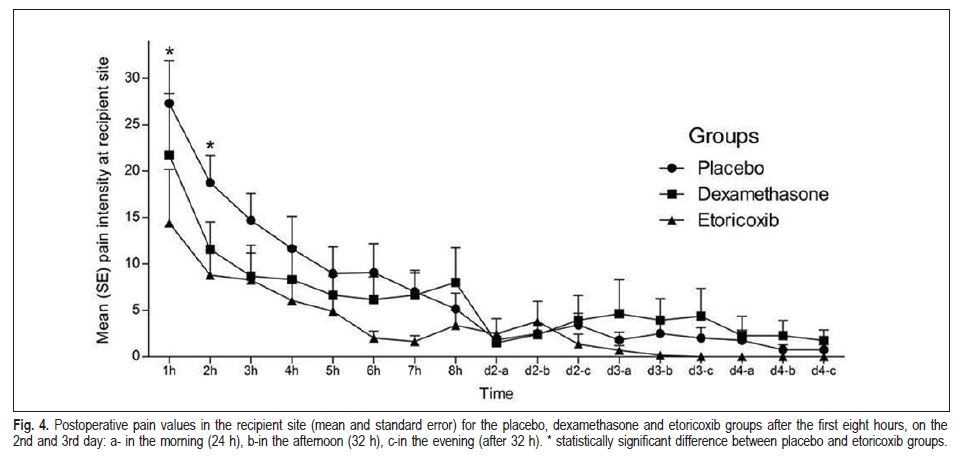
Figure 4 shows the mean and standard error for postoperative pain intensity in the recipient site for the placebo, etoricoxib and dexamethasone groups. There was a statistically significant difference between the placebo and etoricoxib groups only at the 1 h and 2 h periods.
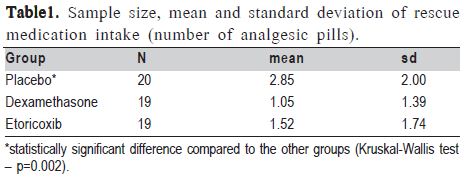
Table 1 shows the mean and standard deviation of rescue medication intake (number of analgesic pills) in each experimental group. Patients from the placebo group ingested a statistically significant higher number of analgesic pills (2.85±2.00) than the other 2 groups (dexamethasone: 1.05±1.39 and etoricoxib: 1.54±1.74; Kruskal-Wallis test – p=0.002).
Discussion
Pain after periodontal surgery is usually associated with tissue damage and has an extremely subjective nature. Some factors that influence the perception of pain are gender, type of surgery and duration of the procedure, in addition to psychological aspects such as stress and anxiety26.
In previous studies of our research group, the prevention and control of postoperative pain was assessed using an openflap debridement surgery model12,22. In the first study in 2006, a statistically significant difference in pain scores was found between the placebo group and the 200 mg celecoxib group after 1, 2, 3, 4, 6 and 7 hours post surgery. However, despite the fact that 200 mg of celecoxib was superior to 4 mg of dexamethasone only at the 4-hour period, the dexamethasone group was superior to placebo, only at the 3-h period22.
In another study12, three pre-emptive anti-inflammatory protocols were evaluated using the same model of periodontal surgery. Etoricoxib (120 mg) was superior to placebo from the third to the eighth postoperative hour and the dexamethasone (8 mg) group was superior to placebo from the fourth to the eighth postoperative hour.
However, one of the major drawbacks of these studies was that most of the patients expressed low scores of pain, even in the placebo group. Therefore, the choice of a mucogingival surgeries model was adopted, since these surgeries are expected to cause more pain than open-flap surgeries for scaling and root planning1.
Different scales have been proposed for the clinical evaluation of acute pain intensity, such as the visual analogue scale9,10,14,17,19-22,27, the 101-point numerical rating scale (NRS- 101)13,16 and the 4-point verbal rating scale (VRS-4)2,12,22, demonstrating a good positive correlation among them. Nonetheless, NRS-101 was chosen because it seems to be better understood by patients and therefore easier to be used28.
In the present study, pain scores were assessed in the first 8 h and three times a day during the following two days after surgery. The higher postoperative pain scores are usually found in the first 24 h12,14,29. These studies support the assessment of postoperative pain at least in the first 8 h after surgery. Since an expressive pain decline was observed 8 h after periodontal surgery, it suggests that a single pre-emptive dose of an anti-inflammatory drug should offer a safe duration of action at least for the first 8 h2,12,14,22.
Although the sample size did not allow a reliable statistical comparison between donor versus recipient area, and also between surgical procedures (free gingival graft versus subepithelial connective tissue graft), pain intensity was higher in the donor than in recipient area, which agrees with Resende et al. (2009)30. Patients who underwent free gingival graft also expressed higher pain complaints than those from subepithelial connective tissue grafts group. This may be explained by the fact that the removal of connective tissue grafts in this study used a "trap door" technique which provides a complete wound closure in the palate31. On the other hand, the free gingival graft technique removes both epithelium and connective tissue. Therefore, it is not possible to close completely the wound with sutures. These may be considered as limitations of this study.
Dexamethasone is a synthetic corticosteroid which has a powerful anti-inflammatory action. The period required for dexamethasone to reach the peak plasma concentration ranges from 1 to 2 h8, and there are favorable results for drug administration both in one or two hours prior to a third molar surgery9. An effective pain control has also been reported for open flap periodontal surgeries with the use of dexamethasone, compared to the placebo group12,22.
The use of steroids with an analgesic purpose is still controversial. Dionne et al. 200332 measured prostaglandin E2 (PGE2) and thromboxane B2 (TxB2) at molar surgical sites using a microdialysis probe and concluded that the use of 4 mg of dexamethasone suppressed PGE2 and TxB2 levels in samples collected at pain onset but without any effect on the pain report. Therefore, a 4g dexamethasone dose does not suppress PGE2 release sufficiently to attenuate peripheral sensitization of nociceptors after tissue injury32,33. In a previous periodontal clinical trial this dexamethasone regimen did not lead also to impressive postoperative pain control compared to placebo after open flap periodontal surgery22.
However, Steffens et al. (2010)12 reported significant postoperative pain prevention and control with the use of dexamethasone 8 mg in open-flap debridement surgery, compared with placebo. Baxendale et al. (1993)17 reported significant pain prevention with the use of dexamethasone 8 mg after multiple third molar extraction compared to placebo. Lin et al. (2006)21 found favorable results in pain control after surgical endodontic treatment. In contrast, Laureano- Filho et al. (2008)25 had lower levels of swelling and trismus, but no effect on pain control with the administration of 8 mg of the dexamethasone in third molar surgery. Additional studies should be conducted to clarify the mechanisms of action and the most adequate dose of dexamethasone for pain control after dental surgeries.
Favorable results in postoperative pain control were achieved with the preemptive use of 8 mg dexamethasone12,22. In the present study this drug regimen was superior to placebo only at the 2nd and 3rd hour after surgery, considering the donor site. No statistically significant difference could be seen between placebo and dexamethasone at any other period. This may be explained by the pharmacokinetic profile of this drug, and also by the higher pain expectance in mucogingival surgeries.
Etoricoxib is a second generation of the coxib's NSAID group. It is highly selective for COX-2, quickly absorbed and reaches optimum plasma levels one hour after administration. It has an elimination half-life of approximately 25 h23. It has a high power of pain relief with an NNT=1.6, according to the Oxford League Table (2007). These data support the use of this medication in the protocol proposed by this study, promoting analgesia for a sufficient length of time. The use of a single 90 mg dose of etoricoxib prior to mucogingival surgery led to a statistically significant lower pain level in the donor site at 1 h, 2 h, 3 h, 7 h and 8 h period, compared to the placebo group. Etoricoxib was also superior to dexamethasone in the first postoperative hour.
Comparing the three experimental groups regarding postoperative pain intensity in the donor site, the etoricoxib group was superior to the placebo group in the 1 h, 2 h, 3 h, 7 h, 8 h periods, and also after 32 h. On the other hand, the dexamethasone group reported less pain compared to the placebo group in the periods of 2 and 3 h after surgery. Similar results were found in the study of Pilatti et al. (2006)22, in which the dexamethasone group was superior to the placebo group in the period of 3 h after surgery.
The etoricoxib group was superior to the dexamethasone group for controlling postoperative pain only in the period of 1 h. The efficacy of etoricoxib over dexamethasone in the first period may be due to pharmacokinetics, since etoricoxib reaches peak plasma concentration in about 1 h, while dexamethasone may take up to 2 h.
In the recipient site, the postoperative pain intensity was lower in the etoricoxib group compared to the placebo group in the 1 h and 2 h periods. No statistically significant difference could be found at any other time periods. Therefore, the major concern of the surgeon with postoperative pain in these modalities of mucogingival surgeries seems to be mostly related to the donor site.
The use of dexamethasone and etoricoxib as preemptive drugs resulted in a statistically significant lower rescue medication intake (paracetamol 750 mg) compared to the placebo group. These findings also agree with those of previous studies12,14.
Any comparison between the present study and the literature is quite limited because so far there are no studies comparing the use of anti-inflammatory drugs administered in a single-dose for pain prevention and control in cases of mucogingival surgery. However, based on our findings, it may be suggested that the use of a pre-emptive single dose of 90 mg etoricoxib or 8 mg dexamethasone may be a valuable and effective protocol for postoperative pain prevention and control in patients undergoing mucogingival surgery.
Acknowledgments
The authors would like to thank Coordination for the Improvement of Higher Education Personnel (CAPES), Brasília, DF - Brazil, for the MSc scholarship (LNZ) that partially funded the study.
References
1. Matthews DC, McCulloch CA. Evaluating patient perceptions as short-term outcomes of periodontal treatment: a comparison of surgical and non-surgical therapy. J Periodontol. 1993; 64:990-7. [ Links ]
2. Vogel RI, Desjardins PJ, Major KVO. Comparison of presurgical and immediate postsurgical ibuprofen on postoperative periodontal pain. J Periodontol. 1992; 63:914-918. [ Links ]
3. American Academy of Periodontology (2001) Glossary of periodontal terms. 4 ed. [cited 2013 Oct 28] Available from: http://www.perio.org/sites/default/files/files/PDFs/Publications/GlossaryOfPeriodontalTerms2001Edition.pdf. [ Links ]
4. Bjorn H. Coverage of denuded root surfaces with a lateral sliding flap. Use of free gingival grafts. Odontol Revy. 1971; 22:37-44. [ Links ]
5. Miller PD Jr. Root coverage using the free soft tissue autograft following citric acid application.III. A successful and predictable procedure in areas of deepwide recession. Int J Periodontics Restorative Dent. 1985; 5: 14-37. [ Links ]
6. Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of localized recessiontype defects. Cochrane Database Syst Rev. 2009; April15: CD007161. [ Links ]
7. Kissin I. Pre-emptive Analgesia. Anesthesiology. 2000; 93: 1138-1143. [ Links ]
8. Czock D, Keller F, Rasche FM, Häussler U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet. 2005; 44: 61-98. [ Links ]
9. Antunes AA, Avelar RL, Martins Neto EC, Frota R, Dias E. Effect of two routes of administration of dexamethasone on pain, edema, and trismus in impacted lower third molar surgery. Oral Maxillofac Surg. 2011; 15: 217-23. [ Links ]
10. Peres MF, Ribeiro FV, Ruiz KG, Nociti-Jr FH, Sallum EA, Casati MZ. Steroidal and non-steroidal cyclooxygenase-2 inhibitor anti-inflammatory drugs as pre-emptive medication in patients undergoing periodontal surgery. Braz Dent J. 2012; 23: 621-8. [ Links ]
11. Mehlisch DR, Aspley S, Daniels SE, Bandy DP. Comparison of the analgesic efficacy of concurrent ibuprofen and paracetamol with ibuprofen or paracetamol alone in the management of moderate to severe acute postoperative dental pain in adolescents and adults: a randomized, double-blind, placebo-controlled, parallel-group, single-dose, two-center, modified factorial study. Clin Ther. 2010; 32: 882-895. [ Links ]
12. Steffens JP, Santos FA, Sartori R, Pilatti GL. Pre-emptive Dexamethasone and Etoricoxib for Pain and Discomfort Prevention After Periodontal Surgery: A Double-Masked, Crossover, Controlled Clinical Trial. J Periodontol. 2010; 81: 1153-1160. [ Links ]
13. Sotto-Maior BS, Senna PM, de Souza Picorelli Assis NM. Corticosteroids or cyclooxygenase 2-selective inhibitor medication for the management of pain and edema after third-molar surgery. J Craniofac Surg. 2011; 22: 758-762. [ Links ]
14. Steffens JP, Santos FA, Pilatti GL. The Use of Etoricoxib and Celecoxib for Pain Prevention After Periodontal Surgery: A Double-Masked, Parallel-Group, Placebo-Controlled Randomized Clinical Trial. J Periodontol. 2011; 82: 1238-44. [ Links ]
15. Joshi A, Parara E, Macfarlane TV. A double-blind randomised controlled clinical trial of the effect of preoperative ibuprofen, diclofenac, paracetamol with codeine and placebo tablets for relief of postoperative pain after removal of impacted third molars. Br J Oral Maxillofac Surg. 2004; 42: 299-306. [ Links ]
16. Aoki T, Yamaguchi H, Naito H, Shiiki K, Izawa K, Ota Y et al. Premedication with cyclooxygenase-2 inhibitor meloxicam reduced postoperative pain in patients after oral surgery. Int J Oral Maxillofac Surg. 2006; 35: 613-17. [ Links ]
17. Baxendale BR, Vater M, Lavery KM. Dexamethasone reduces pain and swelling following extraction of third molar teeth. Anaesthesia. 1993; 48: 961-4. [ Links ]
18. Al-Sukhun J, Al-Sukhun S, Penttilä H, Ashammakhi N, Al-Sukhun R. Preemptive analgesic effect of low doses of celecoxib is superior to low doses of traditional nonsteroidal anti-inflammatory drugs. J Craniofac Surg. 2012; 23:526-9. [ Links ]
19. Shah R, Mahajan A, Shah N, Dadhania AP. Preemptive analgesia in third molar impaction surgery. Natl J Maxillofac Surg. 2012; 3:144-7. [ Links ]
20. Aznar-Arasa L, Harutunian K, Figueiredo R, Valmaseda-Castellón E, Gay-Escoda C. Effect of preoperative ibuprofen on pain and swelling after lower third molar removal: a randomized controlled trial. Int J Oral Maxillofac Surg. 2012; 41: 1005-9. [ Links ]
21. Lin S, Levin L, Emodi O, Abu El-Naaj I, Peled M. Etodolac versus dexamethasone effect in reduction of postoperative symptoms following surgical endodontic treatment: a double-blind study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101: 814-7. [ Links ]
22. Pilatti GL, Santos FA, Bianchi A, Cavassim R, Tozetto CW. The use of celecoxib and dexamethasone for the prevention and control of postoperative pain after periodontal surgery. J Periodontol. 2006; 77: 1809-1814. [ Links ]
23. Shi S, Klotz U. Clinical use and pharmacological properties of selective COX-2 inhibitors. Eur J Clin Pharmacol. 2008; 64: 233-52. [ Links ]
24. Franchimont D. Overview of the actions of glucocorticoids on the immune response: A good model to characterize new pathways of immunosuppression for new treatment strategies. Ann N Y Acad Sci. 2004; 1024: 124-137. [ Links ]
25. Laureano-Filho JR, Maurette PE, Allais M, Cotinho M, Fernandes C. Clinical comparative study of the effectiveness of two dosages of dexamethasone to control postoperative swelling, trismus and pain after the surgical extraction of mandibular impacted third molars. Med Oral Patol Oral Cir Bucal. 2008; 13: 129-132. [ Links ]
 Correspondence:
Correspondence:
Ligia Nadal Zardo
Universidade Estadual de Ponta Grossa
Departamento de Periodontia
Avenida Carlos Cavalcanti 4748, CEP: 84030-900
Ponta Grossa, PR, Brasil
E-mail: ligizardo@hotmail.com
Received for publication: August 12, 2013
Accepted: December 17, 2013













