Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.12 no.3 Piracicaba Jul./Set. 2013
Original Article
Screw loosening of different UCLA-type abutments after mechanical cycling
Marcela C. JunqueiraI; Ricardo F. RibeiroI; Adriana Claudia L. FariaI; Ana Paula MacedoI; Rossana P. AlmeidaI
I Department of Dental Materials and Prosthodontics, Dental School of Ribeirão Preto, University of São Paulo, Ribeirão Preto, SP, Brazil
ABSTRACT
AIM: To evaluate the loss of applied torque (detorque) values in cast and pre-machined abutments for external hex abutment/implant interface of single implant-supported prostheses subjected to mechanical cycling. METHODS: Ten metal crowns were fabricated using two types of UCLA abutments: cast and pre-machined with metal base in NiCrTi alloy and tightened to regular external hex implants with a titanium alloy screw, with an insertion torque of 32 N.cm, measured with a digital torque gauge. Samples were embedded with autopolymerizing acrylic resin in a stainless steel cylindrical matrix, and positioned in an electromechanical machine. Dynamic oblique loading of 120 N was applied during 5 x 105 cycles. Then, each sample was removed from the resin and detorque values were measured using the same digital torque gauge. The difference of the initial (torque) and final (detorque) measurement was registered and the results were expressed as percentage of initial torque. The results of torque loss were expressed as percentage of the initial torque and subjected to statistical analysis by the Student's t-test (p<0.05) for comparisons between the test groups. RESULTS: Statistical analysis demonstrated that mechanical cycling reduced the torque of abutments without significant difference between cast or pre-machined UCLA abutments (p=0.908). CONCLUSION: Within the limitations of this in vitro study, it may be concluded that the mechanical cycling, corresponding to one-year use, reduced the torque of the samples regardless if cast or pre-machined UCLA abutments were used.
Keywords: dental implant, single tooth implant, external hexagon.
Introduction
The mechanical stability of implant-supported fixed restorations may be considered to improve long-term stability and minimize complications1. The stability of the connection between different implant parts is important for the success of the rehabilitation, especially for single tooth restorations. Loosening of abutment screws, mainly with the external hex implants, has been a technical problem that occurs in the first two years of use2. The stability of the external implant-abutment connection has been improved by altering the screw alloys and their surfaces and applying proper torque values to establish higher initial preloads3-5.
A systematic review compared the complications of screw-retained prosthesis showing that the most frequent complication was related to abutment screw loosening (10-55.5%). The incidence of abutment screw loosening was 4.3% in short-term studies and 10% in long-term studies1.
Mechanical factors, such as the implant-abutment fit and the abutment screw preload are involved in the success of implant rehabilitation6. The preload loss during the occlusal load favors the misfit of the implant-abutment connection and may cause screw loosening and fracture. Implant biological factors may be affected due to microgap formation, which can cause periimplantitis7. In vitro and clinical studies have demonstrated the correlation between rotation of the abutment and prosthetic screw loosening and showed the importance of reducing to a minimum the implant-abutment misfit in order to avoid mechanical complications8-9.
The hexagonal configuration prevents abutment rotation on the implant surface and provides a stable screw joint assembly. The amount of freedom between the implant hexagonal extension and its abutment counterpart has also been implicated as a factor in screw joint instability. The applied torque and the masticatory load could generate micromovements, deforming the implant hexagon. Studies have indicated a direct correlation between implant-abutment rotational misfit and screw loosening9-12.
Preload is the tension on a screw generated when a torqueing force is applied to the screw head. Occlusal forces play an important role in screw loosening of hexagonal connection implants; preload is the only force that resists to functional occlusal forces in order to maintain the abutment stability, preventing its separation from the implant. When the preload is exceeded by the occlusal force, the screw will loosen13-14. Several mechanisms can cause screw loosening; one is the embedment relaxation of mating thread surfaces15. Normally, when a screw is tightened, most of the screw responds elastically (plastic deformation occurs only at spots of machining microroughness and asperities at thread flanks). Thus, preload produces a clamping force between the screw head and its seat. The behavior and life of a screw joint depends mainly on the magnitude and stability of that clamping force. In general, the greater the clamped force (preload), the tighter the clamped joint. However, preload values should not be too high and should be within the elastic limit, because retaining screws may yield or break under repeated functional bite forces. On the other hand, the preload values should not be too low in order to retain loose screws under repeated functional forces16.
Eccentric and compressive forces are generated during chewing movements and influence the screw retention3,8,17-20. The optimal preload values for the implant/abutment screw joint have not been fully identified and in single tooth implants this value is critical for screw joint stability21.
The purpose of this study was to evaluate the loss of applied torque (detorque) values in cast and pre-machined (UCLA) type abutments for external hex abutment/implant interface of single implant-supported prostheses subjected to mechanical cycling. The null hypothesis was that torque loss of cast and pre-machined UCLA abutments submitted to the mechanical cycling is similar.
Material and methods
Ten implants with external hexagon (Titamax Ti Cortical; Neodent, Curitiba, PR, Brazil) measuring 3.75 mm in diameter and 13 mm long, five castable UCLA abutments (Neodent) and five Tilite pre-machined UCLA abutments (Neodent), both with 4.1 mm platform size, were used in this study.
Ten metal crowns were fabricated using the two types of abutments: cast and pre-machined UCLA abutments. All crowns were fabricated according to a silicone matrix (Silicone Master; Talmax, Curitiba, PR, Brazil) to present similar dimensions. The patterns were invested in a rapid cycle, carbonfree, phosphate-bonded investment (Castorit Super C; Dentaurum, Ispringen, Germany) and cast using a nickelchromium alloy (Ni-Cr, Verabond II; Aalba Dent Inc., Cordelia, CA, USA) to the castable UCLA abutments and nickelchromium- titanium alloy (Ni-Cr-Ti, Tilite Omega; Talladium, Valencia, CA, USA) to the pre-machined UCLA abutments. Castings were allowed to bench cool and after divesting were lightly abraded by airborne particles of 100-μm aluminum oxide (Polidental, São Paulo, SP, Brazil) at 90 psi pressure, followed by water washing and air drying. No further polishing or finishing was performed. The abutments were fixed to each implant using titanium screws (Ti6Al4V) (Neodent).
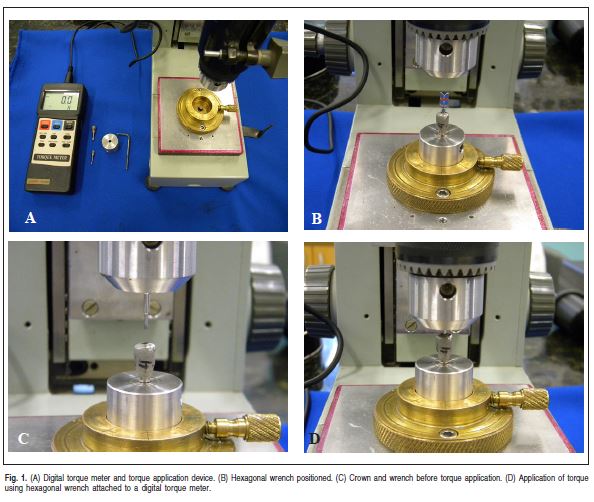
The implants were fixed in a metallic matrix with a lateral screw in order to prevent implant rotation. The set implant/metallic matrix was placed at the base of a torque application device developed in the Department of Dental Materials and Prosthodontics of the Dental School of Ribeirão Preto, University of São Paulo. A digital torque meter was attached to the top of the device (TQ-680; Instrutherm, São Paulo, SP, Brazil). Initially, the crowns were slightly screwed to the implants by hand22. Then the set was placed in a socket at the device base. This socket allows only rotational movement. The crowns were torqued to the implants (32 N.cm), according to manufacturer's recommendation, using a hexagonal wrench. After 3 min, the screw was retightened to the same torque to minimize embedment relaxation23. The placement torque was measured by the digital torquemeter with a 0.1 precision. The sequence is shown on Figure 1 (A-D).
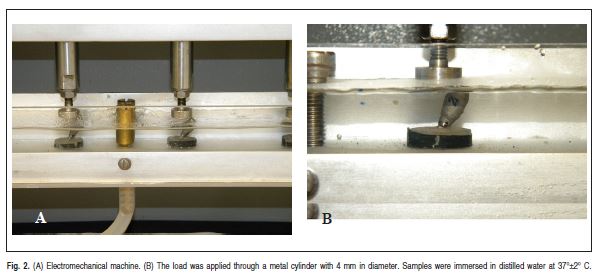
The implant and metal crown were embedded in autopolymerizing acrylic resin (Jet; Clássico Produtos Odontológicos Ltda., São Paulo, SP, Brazil) in a stainless steel cylindrical matrix to standardize the positioning with a 30° inclination relative to the vertical axis24. An autopolymerizing acrylic resin was used due to its appropriate elastic modulus (3GPa) for a bone analog material25. The replicas were positioned in an electromechanical machine (MSFM; Elquip, São Carlos, SP, Brazil) and immersed in distilled water at 37±2 °C. Dynamic oblique loading of 120 N was applied to each replica during 5x105 cycles. The load was applied with a metal cylinder with 4 mm in diameter. The machine was set to work at a frequency of 101 cycles per minute, simulating to the human chewing frequency26 (Fig. 2).
After mechanical loading, each sample was removed from the resin and returned to the torque application equipment in the same initial position, and detorque values were measured with the digital torquemeter. To remove the screw, torque was applied in a counterclockwise direction, using a hexagonal wrench attached to the digital torquemeter. The digital torque was recorded immediately after releasing the screw.
The results of torque loss were expressed as percentage of the initial torque and subjected to statistical analysis by Kolmogorov-Smirnov normality test. The Student's t-test (p<0.05) was used for comparisons between the groups, using the statistical program SPSS 17.0 (Statistic Package for the Social Science, version 17; SPSS Inc., Chicago, IL, USA).
Results
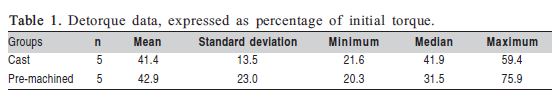
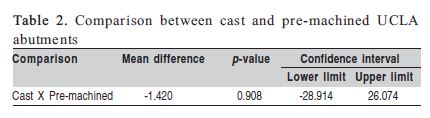
Table 1 shows the results obtained for the different samples after mechanical cycling. No statistically significant difference was observed (p=0.908) when the two types of UCLA abutments (cast or pre-machined) were compared (Table 2).
Discussion
Since the Branemark system was introduced in the market with an external hexagon to facilitate the implant insertion rather than to provide an antirotational device, several competing systems have used well this design over the years27. Even though there were some failures and other design connections were introduced to overcome these failures, many patients received this design connection. Currently, there is lack of conclusive evidence regarding abutment screw loosening to external hexagon implants, mainly those related to single restorations25. Several factors may cause reduction or loss of preload in single tooth restorations such as casting procedures, superstructure inaccuracy, occlusal morphology and insertion torque, occlusal overload and physical properties of the screw materials28-29.
Kano et al.21 studied the casting effect on torque maintenance by detorque measurements of UCLA-type abutments and observed a detorque mean of 92.3% for the machined titanium abutments, 81.6% for the pre-machined palladium abutments cast with palladium, 86.4% for plastic abutments cast with nickel-chromium, and 84.0% for plastic abutments cast with cobalt-chromium alloy.
In this study, there was no statistically significant difference between cast and pre-machined abutments (p=0.908). The detorque measurement after mechanical cycling revealed a reduction to 13.26±4.32 N.cm (41.4%) for the cast abutment and 13.72±7.36 N.cm (42.9%) for the pre-machined. Despite the use of different abutments, torque reduction was observed for both groups, suggesting changes in the mating surfaces. Any irregularities in the mating surfaces will likely result in preload reduction28. The casting procedures may have contributed to these results since integrity of screw joint23 and material properties of metal components may be altered during casting21. Therefore, it is important to point out that any irregularity in the mating surfaces should be detected, as changes occur between contacting parts when the screw is tightened because all the metallic contacting surfaces flatten slightly and the microscopic distance between contacting surfaces decreases21.
Other studies also compared plastic, pre-machined and machined abutments and concluded that lower preload has developed for all components subjected to casting15,21,30. This study confirms such results and shows that casting procedures can decrease detorque values even in pre-machined cast abutments, like those used. The reason seems to be the irregularities and roughness of contacting surfaces that may result from the casting process, which causes greater embedment relaxation and consequent preload loss15,30.
The applied torque is distributed to the friction between the screw and the abutment, and between the threads of the screw and the implant, causing loosening. Thus, screw loosening is only avoided if the applied preload remains constant. Preload is a tension created in screw when a torque force is applied to the screw head and is affected by the screw material's properties. Preload produces a clamping force between the screw head and its seat. The behavior and durability of a screw joint depends mainly on the magnitude and stability of that clamping force. In this study, titanium screws were used, which have a higher friction coefficient than other materials, like gold.
Although the torque values have decreased after mechanical cycling, no movements of the replicas were observed macroscopically, which may indicate the maintenance of screw stability. Then, this torque loss may not immediately reflect in an evident loosening of the joint, but if the process is allowed to continue, it may result in joint instability and separation of abutment from the implant15,31, fracture, patient discomfort and biological complications, such as periimplantitis, because of the microgap created at the interface7. Further studies are required to verify the effects of a larger number of cycles on the longterm retention and stability of different abutments with external connection.
It is difficult to predict clinical results by in vitro studies because there are many factors affecting the oral environment, but the results of the present study allow suggesting that the use of cast or pre-machined UCLA abutments can present similar values of preload and torque loss after simulated use. It is also important to evaluate the mechanisms of the abutment/implant retention screw joint with the study of stress distribution. Additional studies would be helpful to establish the clinical relevance of the present findings.
Within the limitations of this in vitro study, it may be concluded that the mechanical cycling, corresponding to one year of use, reduced the torque of the samples regardless if cast or pre-machined UCLA abutments were used.
References
1. Chaar MS, Att JR, Strub JR. Prosthetic outcome of cement-retained implant-supported fixed dental restorations: a systematic review. J Oral Rehabil. 2011; 38: 697-711. [ Links ]
2. Simon RL. Single implant-supported molar and premolar crowns: A tenyear retrospective clinical report. J Prosthet Dent. 2003; 90: 517-21.
3. Siamos G, Winkler S, Boberick KG. The relationship between implant preload and screw loosening on implant-supported prostheses. J Oral Implantol. 2002; 28: 67-73.
4. Ricomini Filho AP, Fernandes F, Staioto FG, Silva WJ, Del Bel Cury AA. Preload loss and bacterial penetration on different implant-abutment connection systems. Braz Dent J. 2010; 21: 123-9.
5. Guzaitis KL, Knoernschild KL, Viana MAG. Effect of repeated screw joint closing and opening cycles on implant prosthetic screw reverse torque and implant and screw thread morphology. J Prosthet Dent. 2011; 106: 159-69.
6. Weng D, Nagata MJ, Bell M, Bosco AF, Melo LG, Richter EJ. Influence of microgap location and configuration on the periimplant bone morphology in submerged implants. An experimental study in dogs. Clin Oral Implants Res. 2008; 19:1141-7.
7. Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP. A systematic review of the 5-year survival and complication rates of implantsupported single crowns. Clin Oral Implants Res. 2008; 19: 119-30.
8. Binon PP. The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont. 1996; 9: 149-60.
9. Lang LA, Wang RF, May KB. The influence of abutment screw tightening on the screw joint configuration. J Prosthet Dent. 2002; 87: 74-9.
10. Vigolo P, Majzoub Z, Cordioli G. Measurement of the dimensions and abutment rotational freedom of gold-machined 3i UCLA-type abutments in the as-received condition, after casting with a noble metal alloy and porcelain firing. J Prosthet Dent. 2000; 84: 548-53.
11. Theoharidou A, Petridis HP, Tzannas K, Garefis P. Abutment screw loosening in single-implant restorations: a systematic review. Int J Oral Maxillofac Implants. 2008; 23: 681-90.
12. Malaguti G, Denti L, Bassoli E, Franchi I, Bortolini S. Dimensional tolerances and assembly accuracy of dental implants and machined versus cast-on abutments. Clin Implant Dent Relat Res. 2011; 13: 134-40.
13. Schwarz MS. Mechanical complications of dental implants. Clin Oral Implants Res 2000; 11 Suppl: 156-8.
14. Coppedê AR, Mattos MGC, Rodrigues RCS, Ribeiro RF. Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: an in vitro study. Clin Oral Implants Res. 2009; 20: 624-32.
15. Binon PP. The external hexagonal interface and screw-joint stability: A primer on threaded fasteners in implant dentistry. Quint Dent Technol. 2000; 23: 91-105.
16. Jabbari YSA, Fournelle R, Ziebert G, Toth J, Iacopino AM. Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 3: preload and tensile fracture load testing. J Prosthodont. 2009; 17:192-200.
17. Sotto-Maior BS, Senna PM, Silva WJ, Rocha EP, DelBel Cury AA. Influence of crown-to-implant ratio, retention system, restorative material, and occlusal loading in stress concentration in single short implants. Int J Maxillofac Implants. 2012; 27:.e13-8.
18. Akour SN, Fayyad MA, Nagy WW, Fournelle RA, Dhuru VB, Tzenakis GK, et al. Finite element analyses of two antirotational designs of implant fixtures. Implant Dent. 2005; 14: 77-81.
19. Kitagawa T, Tanimoto Y, Odaki M, Nemoto K, Aida M. Influence of implant/ abutment joint designs on abutment screw loosening in a dental implant system. J Biomed Mater Res Part B Appli Biomater. 2005; 75B: 457-63.
20. Yousef H, Luke A, Ricci J, Weiner S. Analysis of changes in implant screws subject to occlusal loading: a preliminary analysis. Implant Dent. 2005; 14:378-85.
21. Kano SC, Binon P, Bonfante G, Curtis DA. Effect of casting procedures in UCLA-type abutments. J Prosthodont. 2006; 15: 77-81.
22. Cardoso M, Torres MF, Lourenço EJV, Telles DM, Rodrigues RCS, Ribeiro RF. Torque removal evaluation of prosthetic screws after tightening and loosening cycles: an in vitro study. Clin Oral Implants Res. 2012; 23: 475-80.
23. Jorge JR, Barão VAR, Delben JA, Assunção WG. The role of implant abutment system on torque maintenance of retention screws and vertical misfit implant-supported crowns before and after mechanical cycling. Int J Oral Maxillofac Implants. 2013; 28: 415-22.
24. International Organization for Standardization. ISO 1480. (2003) Dentistry Fatigue Test for Endosseous Dental Implants. 2007: 1-9.
25. Tsuge T, Hagiwara Y. Influence of lateral-oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J. 2009; 28: 373-81.
26. Piermatti J, Yousef H, Luke A, Mahevich R, Weiner S. An in vitro analysis of implant screw torque loss with external hex and internal connection implant systems. Implant Dent. 2006; 15: 427-35.
27. Gracis S, Michalakis K, Vigolo P, Von Steyern PV, Zwahlen M, Sailer I. Internal vs. external connections for abutments/reconstructions: a systematic review. Clin Oral Implants Res. 2012; 23: 202-16.
28. Hanses G, Smedberg JI, Nilner K. Analysis of a device for assessment of abutment and prosthesis screw loosening in oral implants. Clin Oral Implants Res. 2002; 13: 666-70.
29. Tavarez RRJ, Bonachela WC. Effect of cyclic load on vertical misfit of prefabricated and cast implant single abutment. J Appl Oral Sci. 2011; 19: 16-21.
30. Dixon DL, Breeding LC, Sadler JP, McKay ML. Comparison of screw loosening, rotation and deflection among three implant-designs. J Prosthet Dent. 1995; 74: 270-8.
31. Gracis S, Michalakis K, Vigolo P, Von Steyern PV, Zwahlen M, Sailer I. Internal vs. external connections for abutments/reconstructions: a systematic review. Clin Oral Implants Res. 2012; 23: 202-16.
 Correspondence:
Correspondence:
Rossana Pereira de Almeida
Faculdade de Odontologia de Ribeirão Preto
Universidade de São Paulo
Av. do Café S/N, CEP: 14040-904
Ribeirão Preto, SP, Brasil
E-mail: rpaa@forp.usp.br
Received for publication: May 28, 2013
Accepted: September 20, 2013













