Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.13 no.4 Piracicaba Out./Dez. 2014
ORIGINAL ARTICLE
Intraoperative accidents associated with surgical removal of third molars
Aline Monise SebastianiI; Sara Regina Barancelli ToderoI; Giovana GabardoI; Delson João da CostaI; Nelson Luis Barbosa RebelattoI; Rafaela ScariotII
I Universidade Federal do Paraná – UFPR, School of Dentistry, Department of Stomatology, Area of Oral and Maxillofacial Surgery-Maxillo-facial, Curitiba, PR, Brazil
II Universidade Positivo - UP, School of Dentistry, Area of Oral and Maxillofacial Surgery-Maxillo-facial, Curitiba, PR, Brazil
ABSTRACT
Aim: To evaluate the prevalence of intraoperative accidents associated with extraction of third molars and identify possible risk factors. Methods: Prospective study with patients undergoing third molar surgery by residents of the Oral and Maxillofacial Surgery Service at the Federal University of Parana. Epidemiological data were collected from preoperative evaluation forms. During the surgical procedure were evaluated the radiographic position classifications of all third molars removed, using methods such as osteotomy and/or tooth section, time for the procedure and occurrence of any complication. Results: The students extracted a total of 323 teeth. The mean surgical time was 45 min. Conclusions: The prevalence of intraoperative accidents during extraction of third molars was 6.19%. The most prevalent accident was maxillary tuberosity fracture, followed by hemorrhage. Age, positioning of the teeth and use of the techniques of osteotomy and tooth section are possible risk factors.
Keywords: molar third; surgery oral; radiography; intraoperative complications; tooth extraction.
Introduction
Extraction of third molars is routinely performed by non-specialist dentists. However, it is a procedure associated with some difficulties, like the molar's close anatomical relationship with the noble anatomical structures, the angle of teeth crowns and impactions. Besides, there are surgical complications like bleeding, nerve damage, injuries to adjacent teeth, fracture of maxillary tuberosity, displacement of the tooth to other anatomical structures and fracture of the dental apex1.
Bleeding occurs in 0.2% to 5.8% of third molar extractions, transoperatively or postoperatively, locally or systemically. It's four times more common in mandibular third molars than maxillary third molars. The highest incidence is in the deeply impacted distoangular teeth and in older patients2. Injury to the inferior alveolar nerve after removal of third molars occurs in 0.4 to 8.4% of cases, less than 1% permanent. Lingual nerve damage ranges from 0 to 23%3.
Damage to the second molars is reported in 0.3% to 0.4% of these surgeries. The positions of third molars of greatest risk for this complication in maxilla are mesial associated with Class B (Pell and Gregory4), already in the mandible, the position is vertical2. The position of the maxillary third molar at the end of the dentoalveolar arch is such that the posterior portion cannot be supported, and the internal composition of the bone may be of the maxillary sinus, or porous bone. This facilitates fracture of maxillary tuberosity, which is more associated with erupted third molars and excessive use of force5. Moreover, these teeth have close anatomical relationship with the maxillary sinus. Thus, a tooth extraction can lead to an accidental opening of the sinus or displacement of the tooth in the sinus, especially due to inadequate use of extractors6. Displacement of the tooth into other adjacent structures may occur occasionally, such as the infratemporal fossa7. Another common complication, the fractured tooth root apex, may occur mainly in root lacerations such as hypercementosis and ankylosis, conditions that increase resistance to avulsion8.
According to Araujo, 20119, some variants are related to accidents and complications occurring during surgery of these teeth: patient age, tooth position, surgeon's experience and time of surgery. Attention to surgical details, including patient preparation, asepsis, careful handling of tissues, control of instrument force, control of hemostasis and adequate postoperative instructions, reduce the rate of complications.
The aim of this study was to evaluate the prevalence of intraoperative accidents in patients undergoing extraction of third molars and identify possible risk factors.
Material and methods
Data for the development of this research were collected by a prospective study. It was approved by Ethical Research Committee on Human Beings at the Human Health Department under number CEP/SD:1021.146.10.10 and CAAE:0086.0.091.000-10. All patients gave signed an informed consent.
Sample selection: All patients undergoing third molar surgery by residents of the Oral and Maxillofacial Surgery Service at the Federal University of Parana were invited to participate in the study (September 2010 to September 2011). For this purpose, the patients were informed about the research and invited to sign the term of consent, granting permission for the collection and use of information arising from the surgery, knowing that it would not influence their procedure. Surgeons prescribed preoperative (injectable steroids – betamethasone - one hour before the procedure) and postoperative (NSAIDs, analgesics and antibiotics if needed) medications. Inclusion criteria comprised patients who had their third molars removed during the period covered by the study under local anesthesia, 18 years of age or older, presenting records with panoramic radiographs, and signing the informed consent form. Patients with some systemic changes (hypertension, anemia, and diabetes) were excluded.
Data collection: Epidemiological data (age, gender and ethnics) were collected in preoperative evaluation files. The researcher in charge of data collection followed the entire surgical procedure, analyzing panoramic radiographs exposed in the operating room, giving the radiographic position of all removed third molars, following the classifications by Winter10 and Pell and Gregory4. Winter classified third molars as vertical, horizontal, mesioangular, and distoangular, according to the angulation of the long axis of the third molar in relation to the long axis of the second molar9. Pell and Gregory4 related the tooth to the ramus of the mandible. In their class I, the crown is completely in front of the anterior border of the ascending branch; in their class II, the tooth is partially within the mandibular branch, and in class III, the tooth is located completely in the ascending branch of the mandible. They also classify teeth in relation to the occlusal plane as follows: in A, the occlusal surface of the third molar is the occlusal plane of the second molar; in B, the occlusal surface of the tooth is not erupted between the occlusal plane and cervical line of the second molar; and in C, the occlusal surface of the unerupted tooth is below the cervical line of the second molar9. All radiographs were performed by the equipment at the Department of Dental Radiology, Orthophos model 90 kV/12 mA (Siemens Corp.,Erlangen, Germany) at preoperative evaluation of the patient.
The researcher recorded methods such as osteotomy and/ or tooth section, time of the procedure in minutes and any complications, such as hemorrhage, displacement of teeth to the adjacent spaces, damage to adjacent teeth, soft tissue injuries, maintenance apex/root, tuberosity fracture, and dislocation of the mandible. Any active bleeding observed during osteotomy, tooth section and avulsion which had not ceased after five minutes of compression with gauze was considered hemorrhage.
Statistics: Data of patients were entered in a Microsoft Excel for Windows® spreadsheet specifically developed for the study. Statistical evaluation was performed using frequency analysis and specific statistical tests (Statistical Package for Social Sciences-SPSS, version 15.0, SPSS Inc. Chicago, IL, USA), with a 95% confidence interval.
Results
The sample consisted of 150 patients who underwent surgery for removal of third molars. The mean age was 24 (18-62). There were more females than males (n=95/63.3%).
A total of 323 teeth were extracted: 164 maxillary third molars and 159 mandibular third molars. Osteotomy was performed in 26 maxillary third molars and in 113 mandibular third molars. Tooth section was not done in maxillary third molars, but it was in 84 mandibular third molars. The minimum surgical time was 15 min and the maximum was 1 h and 40 min, with a mean time of 45 min.
There was no statistical association between intraoperative accidents and gender (chi-square test p=0.526) or ethnics (chi-square test p=0.361). However, there was a significant correlation between accidents and age (Mann- Whitney test p=0.041). The most prevalent accident was fracture of maxillary tuberosity; the mean age of patients who had this complication was 24.3. The second most prevalent accident was hemorrhage; the mean age for these patients was 29. There was no relationship between intraoperative accidents and surgical time.
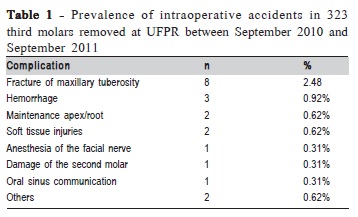
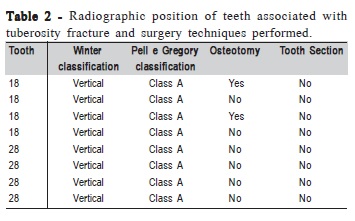
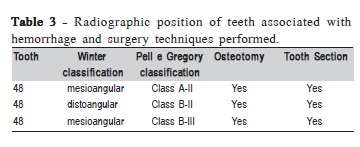
Intraoperative accidents occurred during the removal of 20 third molars (6.19%). Table 1 shows these accidents. Table 2 shows the relationship of tuberosity fracture with radiographic position of the teeth and use of osteotomy and tooth section. Table 3 relates hemorrhage to the same variables.
Discussion
Impacted third molars are developmental pathological medical deformities characteristic of modern civilization, accounting for 98% of all impacted teeth11. Transoperative accidents during third molar surgery are not uncommon and the professional who performs this procedure must be able to solve these possible operative complications. In the literature complications have been associated with the experience of the surgeon. Berge and Gilhuurs compared complications following surgical removal of third molar in two groups of patients. Surgery was performed in the first group by four general dental practioners and in the second group by consulting oral surgeons, who had fewer complications and shorter surgeries12.
In a retrospective study, Bui et al. (2003)13 found an operative complication rate of 2.2%. Chiapasco (2006)14, found an incidence of intraoperative accidents of 1.1% and side effects of mandibular third molar surgery of 4% for maxillary third molar surgery. In the present study, the prevalence of transoperative accidents was 6.19%, the difference due to varying definitions of complications, study design, and different methods of evaluating study variables. These two studies were retrospective, which reduces the authenticity of these prevalences: many trans-operative complications may have occurred and not registered in the records. In the Chuang (2007)15 prospective cohort study, the intraoperative complication rate was 3.9%, however, it does not mention the accidental maxillary tuberosity fracture, which was the most prevalent transoperative accident in this study, neither do the above cited studies13-14.
Kato et al. (2010)16, while investigating accident rates and complications in third molar surgery, found a higher rate of accidents and complications in female patients (73.91%) than in male patients (27.28%). However, in this study the vast majority of patients (70.45%) were females, thereby increasing the chances of an accident or complication in this group of patients. This study found no statistical relationship between gender or ethnics and the complications.
A statistically significant difference with age was found. The older the patients, the more complications associated with the procedure. A prospective cohort study of a sample of subjects having extracted at least one third molar found that those over 25 years old had an increased risk of complications14. In a study of Benediktsdóttir et al. (2004)17, older groups had more than twice the risk of a prolonged operating time than the youngest group. According to Hupp5, in cases of extreme age, surgical removal of the third molars is contraindicated because as the patient ages, the bone becomes increasingly more calcified and thus less flexible. As a result, more bone should be removed during the procedure. Postoperative reaction is less favorable in these patients and post-operative sequel more likely. Therefore, in older patients (usually over 40) with asymptomatic impacted teeth, removal is not indicated. The Osborn et al. (1985)18 prospective study evaluated surgical and postsurgical problems of patients of a wide range of ages who had third molars removed and concluded that removal during teenage years decreased operative and postoperative morbidity.
Oliveira (2006)1 correlated the incidence of accidents and complications with time of surgery. Dental extractions performed in less than 60 min, had an accident rate of 9.6% but those over 120 min had one of 83.33%. Those authors also observed more accidents and complications relative to the complexity of surgical procedures. Other studies show the post-operative morbidity increase with longer procedures19. This study found no relationship between complications and surgical time.
Bui et al. (2003)13 found in their study that the most prevalent complication was inferior alveolar damage (1%), followed by bleeding (0.7%), oroantral communication (0.3%), and incomplete root removal (0.2%). In the present study, no cases of inferior alveolar damage occurred. However, bleeding was the second most prevalent complication (0.92%), ahead of communication (0.31%) and incomplete root removal (0.62%). This study showed a higher prevalence of bleeding than nerve damage because only intraoperative complications were observed, unlike other studies that evaluated postoperative complications such as paresthesia.
The highest prevalent complication in this study can be seen in Table 2. All teeth associated with tuberosity fracture presented vertical position according to the classification of Winter and "class A" according to Pell and Gregory4, which means that the occlusal surface of the third molar was the same of the second molar, corresponding to completely erupted teeth. This occurs when the tooth is completely erupted, it gets occlusal load, reducing the periodontal ligament, therefore favoring fracture of the tuberosity. Bui et al.13 found a statistical relationship between position of the teeth according to the classification of Winter and complications. They never conducted tooth section, and only twice performed osteotomy, maneuvers that could have presented tuberosity fracture. Ngeow (1998)20 stated that if a pre-extraction radiograph revealed a large antrum, an appropriate technique to avoid fracture of the tuberosity would be sectioning of the tooth and removal of one root at a time, or removing an adequate amount of bone from the sides of the tooth to facilitate a gentle levering out of its socket without disturbing the fractured bone. If a maxillary tuberosity is fractured, the surgeon must determine the extent of the fracture by palpating the mobile fragment. If the fracture is small, the maxillary tuberosity is removed with the tooth. If the bony fragment is large, a sharp instrument should be inserted into the distobuccal cervical area of the tooth and used to separate the alveolar bone from its roots, keeping the remaining bone attached to the periosteum so that it will be perfused continuously, and it must be compressed against the communication. The gingiva should then be sutured. The sutures should be removed only after 2 weeks. In some cases the tuberosity fracture involves the maxillary sinus. In such cases, antibiotics, nasal decongestant, and antiinflammatory analgesics should be prescribed to help preventing maxillary sinusitis. The patient should be advised against blowing his or her nose20. In this study, only one patient had oral sinus communication.
According to Boulox et al. (2007)2, hemorrhage is more prevalent in older patients with deeply impacted teeth and four times more associated with mandibular third molars than maxillary third molars. In this study the mean age in patients who suffered hemorrhage was 29, higher than the general mean (24). All teeth associated with hemorrhage were mandibular third molars and bent, with some portion localized in the mandibular branch (Table 3), therefore harder to extract. In all cases, there was osteotomy and tooth section, which can lead directly to bleeding, because when the drill breaks the bone marrow, it may cause a medullar bleeding. In some cases the inferior alveolar vascular-nervous plexus is reached, causing a vascular hemorrhage. In both hemorrhage cases in this study, hemostasis was done with gauze and fibrin sponge. Agrawal et al. (2014) 21 found in their study that extractions associated with both osteotomy and odontotomy are associated with higher risk of complications21. For Delamare (2012)22, the panoramic radiograph should be routinely used as an auxiliary examination for treatment planning of mandibular third molar removal, due to its wide availability, low cost, and relatively low exposure dose. Other traditionally accepted options for estimation of difficulty and risk during lower third molar removal are the classifications of Pell & Gregory and Winter. The association of intraoperative accidents with the radiographic position of the third molars in this study shows the usefulness of both methods.
Fractured roots are the most common problem associated with tooth extraction, according to Hupp (2009)5. This accident is usually associates with long, curves and diverge roots', in a dense bone. In some situations, the risks of removing a small fragment of the fractured apex may outweigh the benefits, like a risk of moving it to any anatomical structure. The two teeth that had their apexes buried were mandibular third molars and were near to alveolar nerves. If the root meets the following four conditions, it should be left in the alveolar process: the fragment has to be less than 5 mm long, deeply inserted into the bone, free of infection and showing no radiolucent areas around the root apex.
This study also had two cases of injury to the soft tissues, which may occur when instruments such as a lever straight line or periosteal peeler slip from the surgical field and puncture or lacerate adjacent tissues. This can be avoided with controlled force, with special attention to the support of a finger or hand stand against the anticipation of sliding. Abrasions or burns of the lips can still occur due to oral commissure or patchwork resulting from rotational friction rod. The surgeon and his assistant should be vigilant against this5.
Malamed (2012)23 mentioned transient facial paralysis as a possible complication of the inferior alveolar nerve block anesthetic technique. This was commonly caused by the introduction of local anesthetic into the capsule of the parotid gland, which is on the posterior border of the mandibular branch, where the terminal branches of the facial nerve extend. Symptoms include the inability to close the eyelid and lower slope of the upper lip on the affected side. The reflex protective cover of the eye is abolished, but it retains its corneal reflex and lubricates with tears when irritated. The loss of motor function of the muscles will not last more than a few hours. The problems are cosmetic. When the needle tip is in contact with the bone (on the medial branch) prior to deposition of the solution, it keeps the local anesthetic solution off the parotid gland. The patient was informed of what was happening and was monitored with a cap holding the eye closed until the anesthesia effect passed.
Damage to adjacent teeth can be minimized if care is taken to visualize the entire operating field rather than the tooth being extracted. Susarla (2003)24 noted that a surgeon aware of the periphery of the operating field is often able to anticipate possible damage and take action to prevent its occurrence24. Teeth with large restorations or carious lesions are always at risk of fracture or damage upon elevation. Correct use of surgical elevators and bone removal can help to prevent this. Preoperative discussion should take place with highrisk patients2. If an adjacent tooth is luxated or avulsed inadvertently, the most common course of action is repositioning the tooth followed by fixation.
The conclusion of this study is that the possible risk factors of intraoperative accidents identified in this study were age, positioning of teeth, and use of osteotomy and tooth section. The surgeon who performs the surgical removal of third molars should be aware of the risk factors and able to solve possible complications during the procedure.
References
1. Oliveira LB, Schmidt DB, Assis AP, Gabrielli MAC, Vieira EH, Pereira Filho VA. Review of accidents and complications associated with extraction of third molars. Rev Cir Traumatol Buco-Maxilo-Fac. 2006; 6: 51-6. [ Links ]
2. Bouloux GF, Steed MB, Perciaccante VJ. Complications of Third Molar Surgery. J Oral Maxillofacial Surg Clin N Am. 2007; 19:117-28.
3. Ziccardi VB, Zuninga JR. Nerve injuries after third molar removal. Oral Maxillofacial Surg Clin N Am. 2007; 19: 105-15.
4. Pell GJ, Gregory GT. Report a ten-year study of a tooth division technique for the removal of impacted teeth. Am J Orthod. 1942; 28: 660.
5. Hupp JR, Ellis E, Tucker MR. Oral maxillofacial surgery and contemporary. 5. ed. Rio de Janeiro: Elsevier; 2009.
6. Graziani, M. Oral and maxillofacial surgery. 8. ed. Rio de Janeiro: Guanabara Koogan; 1995.
7. Primo BT, Stringhini DJ, Klüppel LE, Costa DJ, Rebellato NLB, Moraes RS. Delayed removal of maxillary third molar displaced into the infratemporal fossa. Rev Esp Cir Oral Maxilofac. 2014; 36: 78-81.
8. Gregori, C. Dental surgery for the general practitioner. New York: Sarvier; 1988.
9. Araújo OC, Agostinho CNLF, Marinho LMRF, Rabêlo LRS, Bastos EG, Silva VC. Accidents and complications incidence in third molar surgeries. Rev Odontol UNESP. 2011; 40: 290-5.
10. Winter L. Operative oral surgery. Saint Louis: Mosby; 1941.
11. Egbor PE, Saheeb BD.A prospective randomized clinical study of the influence of primary closure or dressing on post-operative morbidity after mandibular third molar surgery. Niger J Surg. 2014, 20: 59-63.
12. Berge TI, Gilhuus-MOE ET. Per-and post-operative variables of mandibular third-molar by oral maxillofacial surgery and general dentistry residentes. Spec Care Dentist. 1993, 13: 122-6.
13. Bui CH, Seldin EB, Dodson TB. Types frequencies and risk factors for complication after third molar extractions. J Oral Maxillofac Surg. 2003; 61: 1379-89.
14. Chiapasco M, Cicco L, Marrone G. Side effects and complications associates with third molar surgery. Oral Surg Oral Med Oral Pathol. 2006; 76: 412-20.
15. Chuang SK, Perrott DH, Susarla SM, BA, Dodson TB. Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg. 2007; 65:1685-92.
16. Kato RB; Bueno RBL, Oliveira PJ Neto, Ribeiro MC; Azenha MR. Accidents and complications associated with third molar surgery performed by dental students. Rev Cir Traumatol Buco-Maxilo-Fac. 2010; 10: 45-54.
17. Benediktsdóttir IS, Wenzel A, Petersen JK, Hintze H. Mandibular third molar removal: Risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 97: 438-46. 18. Osborn TP, Frederickson G Jr, Small IA, Torgerson TS. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg. 1985; 43: 767-9.
19. Pathak S, Vashisth S, Mishra S, Singh SP, Sharma S. Grading of extraction and its relationship with post-operative pain and trismus, along with proposed grading for trismus. J CLin Diagn Res. 2014; 8: ZC09-11.
20. Ngeow WC. Management of the fracture maxillary tuberosity: an alteramtive method. Quintessence Int. 1998, 29: 189-90.
21. Agrawal A, Yadav A, Chandel S, Singh N, Singhal A. Wisdom toothcomplications in extraction. J Contemp Dent Pract. 2014; 15: 34-6.
22. Delamare EL, Liedke GS, Vizzotto MB, Silveira HLD, Azambuja TWF, Silveira HED. Topographic relationship of impacted third molars and mandibular canal: correlation of panoramic radiograph signs and CBCT images. Braz J Oral Sci. 2012, 11: 411-5.
23. Malamed SF. Handbook of local anesthesia. 6. ed. Saint Louis: Mosby Elsevier; 2012.
24. Susarla SM, Blaeser BF, Maganalnick D. Third molar surgery and associated complications. Oral Maxillofacial Surg Clin N Am. 2003; 15: 177-86.
 Correspondence:
Correspondence:
Aline Monise Sebastiani
Rua Maurício Nunes Garcia, 250 - Apto 603
Jardim Botânico
CEP: 80210-150 Curitiba, PR, Brasil
E-mail: sebastiani.aline@gmail.com
Received for publication: August 14, 2014
Accepted: November 26, 2014













