Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.13 no.4 Piracicaba Out./Dez. 2014
ORIGINAL ARTICLE
Efficiency of occlusal splints on police officers with TMD
Paulo Henrique Ferreira CariaI; Reinaldo José A. FariaII; Claudia Regina Sgobbi de FariaIII; Carla Scanavini CrociI; Fábio Renato Rubens Negrão FilhoI
I Universidade Estadual de Campinas - UNICAMP, Piracicaba Dental School, Department of Morphology, Piracicaba, SP, Brazil
II Universidade do Oeste Paulista - UNOESTE , Dental School, Department of Health Sciences, Presidente Prudente, SP, Brazil
III Universidade Estadual Paulista - UNESP, School of Science and Technology, Department of Physiotherapy, Presidente Prudente, SP, Brazil
ABSTRACT
Aim: To evaluate of the effect of two different occlusal splints on police officers with TMD. Methods: Thirty police officers were selected based on Research Diagnostic Criteria for TMD and on clinical exams. Volunteers (ten per group) were distributed according to occlusal splints: group A – Control, group B - Michigan Occlusal Splint (MOS), and group C – Planas Appliance (PA). Experimental groups were analyzed using a visual analog pain scale (VAPS), subject to a clinical evaluation of temporomandibular joint. Bilateral surface electromyographic activities of anterior and posterior temporal, masseter and suprahyoid muscles were analyzed at rest and during clenching, before and after four weeks using the occlusal splints. Results: The left and right temporal and masseter muscles sensitivity decreased after using both splints. Pain symptoms increased for group A (Control) and decreased for group C. Conclusions: Planas Appliance was more efficient on pain reduction than the Michigan Occlusal Splint.
Keywords: temporomandibular joint disorders; stress, physiological; electromyography, masticatory muscles, occlusal splints.
Introduction
Temporomandibular joint disorder, commonly referred to as TMD, is a compound of disorders characterized by orofacial pain, chewing dysfunction, or a combination of both. Common symptoms of facial pain include actual pain, headache, joint discomfort or dysfunction, earaches, tinnitus, dizziness, pain in the upper and lower back, or neck pain.
Stress is one of the most important factors causing temporomandibular disorder (TMD) and professional activity is a significant source of stress1. Police officers are exposed to high levels of stress and therefore susceptible to chronic diseases and disorders like TMD2. The incidence of signs and symptoms associated with TMD includes 6% to 93% of the population, but only 3.6% to 7% requires treatment3. Some studies report high incidence of signs and symptoms associated with TMD in war veterans4-5, but few reports evaluated incidence of TMD in police officers6.
Stressful situations may intensify TMD symptoms, which are frequently treated using occlusal splints. In most cases, this therapy balances the masticatory muscles' activity and reduces bruxism and TMD symptoms7.
Surface electromyography is a non-invasive exam that enables the evaluation of muscle activity in people with TMD as well as the analysis of the occlusal splints' effect on masticatory muscles8-11.
Based on the connection between stressful activity and TMD, this study suggests that the effect of two different occlusal splints on the temporal, masseter and suprahyoid muscles of police officers with TMD be evaluated based on clinical symptoms and electromyographic activity.
Material and methods
Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD).
RDC/TMD is a dual-axis system developed by Dworkin and LeResche in order to define the subtypes of TMD and to standardize their diagnosis. Axis I is a physical measure that outlines the clinical characteristics of TMDs, separating them into three categories: myofascial pain disorder (MPD); disc displacements (DD); and degenerative joint conditions (DJD). Axis II assesses psychosocial factors commonly seen in patients with TMD.
Volunteers
A total of 905 police officers in the State of São Paulo completed the RDC/TMD Axis II12 after being approved by the Human Research Ethics Committee of UNICAMP in Brazil. 256 volunteers were selected and subject to RDC Axis I, including the ones who showed myogenic or mixed TMD, TMJ pain for at least three months and joint tenderness on palpation on at least one side. Thirty volunteers (15 women and 15 men) with mean age of 29 years and an indicative diagnosis of myogenic or mixed TMD were selected. Each volunteer filled out a visual analog pain scale (VAPS) questionnaire to evaluate muscle pain sensibility.
Volunteers were randomly divided into three different groups according to occlusal splints as follows:
Group A – Control
Group B – Michigan Occlusal Splint (MOS);
Group C – Planas Appliance (PA).
After four weeks of treatment, volunteers completed again the RDC Axis I and Axis II12 in the morning, supervised by the same examiner.
Occlusal Splints
Occlusal splits were used during four weeks while the volunteers were sleeping.
1. MOS – A 4.5mm thick rigid acrylic resin plate which was checked every 7 days. All necessary adjustments were performed on it.
2. PA –Two (maxillary and mandibular) bilateral rigid acrylic resin plates parallel to Campers' plane.
Volunteers were instructed to avoid contact with each other during treatment to keep differences between occlusal splints and control groups confidential.
Instrumentation
Electromyography (EMG) records were performed on temporal, masseter and suprahyoid muscles before and after using occlusal splints for four weeks. Volunteers remained seated, facing forward, feet on the floor, legs at a 90º angle, hands resting on thighs and Frankfort plane parallel to the floor. Occlusal splints were removed during EMG documentation.
All EMG signals were obtained by Lynx Data Acquisition System (MCS1000-V2) with 16 channels, 12-bit resolution of dynamic range, Butterworth filter, 500 Hz band pass, 20 Hz high-pass filter and unit gain of 2000 times. Software Aqdados 5, Lynx was used with a sampling frequency of 1000 Hz and active single differential surface electrodes with entrance impedance of 10 G, CMRR (Common Mode Rejection Ratio) of 80 dB, impedance of 1012 W / % pF, and unit gain of 20 times. A reference electrode was positioned on the sternum bone of the volunteers.
Surface electrodes were bilaterally placed on the masseter, temporal and suprahyoid muscles, according to muscle palpation and their function. Electrodes were attached to the skin (previously cleaned with alcohol) using double-sided adhesive tape over the center of the muscle and parallel to the muscle fibers, placing the silver bars perpendicular to their direction to maximize signal capture and minimize noise interference.
EMG analysis was performed in three different moments:
First: 5 seconds of muscle resting.
Second: Maximum voluntary contraction (MVC) bilaterally biting two pieces of elastic cord (Lemgruber® no. 201), each 2.5cm long.
Third: Maximum voluntary contraction of the suprahyoid muscle at maximal mouth opening (MMO). Signals were stabilized using RMS (Root Mean Square) of three MVC measurements. Each EMG exam was performed after 3 minutes of rest to physiologically recover and to avoid muscle fatigue.
The statistical analyses were: Tukey's test (5% level of significance) and Student's t-test for EMG data; Shapiro-Wilk tests (5% level of significance) for normality; Mann-Whitney and Student t-test for data from the clinical evaluation and RDC.
Results
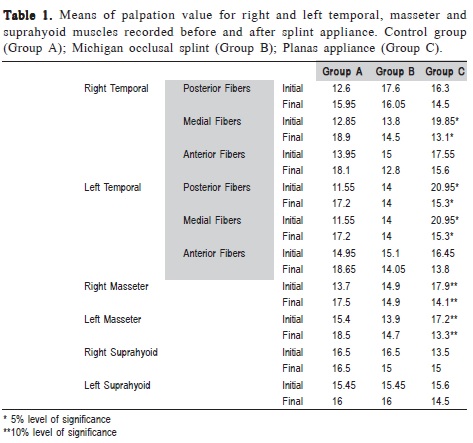
Palpation in group C (PA) showed statistically significant reduction (p<0.05) to sensitivity on the left side of the posterior fibers of the temporal muscle and on both sides of the medial fibers, as well as on both sides of the superficial fibers of the masseter muscle (p<0.10) (Table 1). Control Group did not show statistically significant differences.
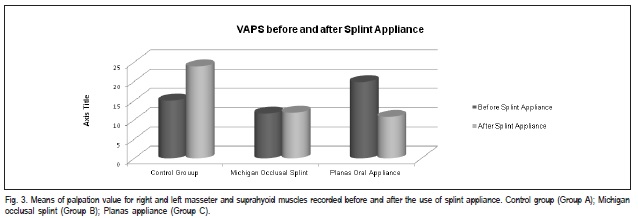
VAPS data showed a statistically significant difference in the means of groups A and C compared to group B, indicating an increase of pain symptoms in group A (Control Group) and symptom alleviation in group C (PA) (Figure 3).
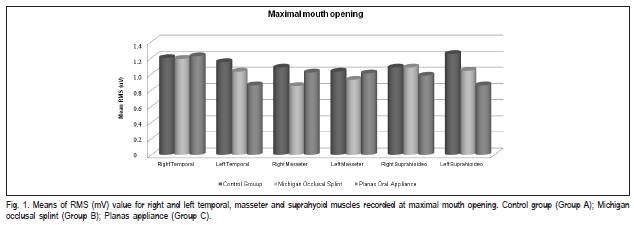
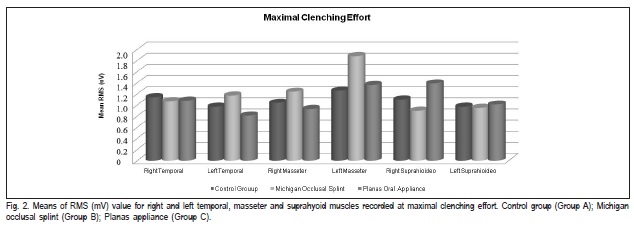
RMS values of EMG exam (Figures 2 and 3) showed association with the clinical aspects. EMG signal analysis showed a statistically significant difference (p<0.05) only for the right masseter muscle during maximal clenching effort in groups B and C.
Discussion
Most epidemiological studies about the association between occlusal factors and TMD have used samples representing general populations13 In addition, studies about TMD often evaluate heterogeneous samples in patients with different kinds and degrees of TMD that compromise repeatability and data comparison and limit clinical application14. Police work is highly stressful, since it is one of the few occupations where employees are constantly asked to face physical dangers and put their lives on the line any time15 .Hence, we decided to use this specific population, divided in homogenous subgroups, matched by age and gender, and evaluated by standardized criteria and blind experimental designs to reduce observer bias.
Occlusal splints have been the preferred modalities in the management of myofascial temporomandibular disorders (TMDs)16. Some authors advocate the use of these splints as a first step for therapeutic treatment in order to minimize the neuromuscular unbalance since it is the prevalent factor in this kind of dysfunction16-17. The use of occlusal splints seems to relieve TMD symptoms18-19. A significant number of clinical works evaluated the therapeutic effect of occlusal splints on muscular hyperactivity20-22. EMG is a valuable resource that evaluates muscle activity able to recognize signs related to TMD, thus helping establish differential diagnosis23-24.
Differences in the clinical protocols used to establish TMD diagnoses may be responsible for the high result variability between studies. The introduction of Research Diagnostic Criteria for Temporomandibular Disorders (RDC/ TMD) in 199212 was expected to increase the level of consistency between studies by the use of standardized diagnostic criteria. RDC/TMD provides criteria for a dualaxis diagnosis, i.e. the patient receives physical diagnosis (axis I) along with a psychosocial assessment (axis II).
Clinical exam showed statistically significant reduction to bilateral palpation sensitivity in group C's temporal and masseter muscles, which means a reduction of muscle hyperactivity, since occlusal mechanoreceptor splints cancel neuromuscular activity, favor blood flow and remove unnecessary substances resulting from excessive muscle contraction25. In group A any statistically significant difference was noticed because volunteers did not receive any kind of TMD treatment and so the symptoms remained.
The results obtained by VAPS showed significant muscle pain reduction in group C. This confirms the clinical results, in which the use of occlusal splints relieves TMD symptoms19 and reinforces the theory about blood flow increase and unnecessary substance removal inside the muscle25. In addition, occlusal splints change the maxillomandibular relation repositioning articular structures while balancing the muscular action3.
MOS had already been tested as a TMD treatment26, whereas PA had no scientific report as such. In our research, PA also caused muscle stretching by increasing vertical dimension of occlusion and eliminating occlusal interferences, which reduced periodontal proprioception causing muscle relaxation.
EMG activity of the masseter and temporal muscles in patients with TMD using occlusal appliances is a controversial subject. Some authors report reduction of EMG activity in these muscles27 while others stated that there are no statistically significant differences in the muscle activity11,28. Even after following ISEK recommendations, personal dissimilarities can develop different outcomes and interfere on EMG results, as well as different muscle structures29.
In this study, EMG values for the right masseter muscle in groups B and C showed statistically significant differences during maximal clenching effort. The contraction of the masseter muscle during mouth opening occurs as a response to a protective reflex in patients who have muscle pain while opening their mouths25. The temporal muscle is a mandibular positioner, and since occlusal splints interrupt the proprioceptive information of the mechanoreceptors located in the periodontal ligament, which balances muscular activity, they provide a better mandible positioning and therefore loosen that muscle30.
EMG activity of muscles studied in these circumstances did not show significant changes. However, there was a clinically significant reduction in the palpation sensitivity of temporal and masseter muscles in group C, indicating relief for TMD symptoms, as stated by other authors11.
EMG activity and pain sensation are probably distinct due to longer latency of EMG responses, when compared to pain reduction, so a prolonged time in the use of oral appliances could improve EMG results, relieving muscle pain. On the other hand, PA keeps teeth without occlusal contact and its prolonged use can lead to occlusal alterations17.
In conclusion, Planas appliance was more efficient in pain reduction than the Michigan occlusal splint; the type of occlusal splints chosen did influence on pain reduction; occlusal splints showed advanced clinical outcomes.
Acknowledgements
This research was supported by CAPES. The authors wish to thank the force unit commander of the 18th district Presidente Prudente Police Department.
References
1. Slade GD, Diatchenko L, Bhalang K, Sigurdsson A, Fillingim RB, Belfer I et al. Influence of psychological factors on risk of temporomandibular disorders. J Dent Res. 2007; 86: 1120-5. [ Links ]
2. Collins PA, Gibbs AC. Stress in police officers: a study of the origins, prevalence and severity of stress-related symptoms within a county police force. Occup Med (Lond). 2003; 53: 256-64.
3. LeResche L, Mancl L, Sherman JJ, Gandara B, Dworkin SF. Changes in temporomandibular pain and other symptoms across the menstrual cycle. Pain. 2003; 106: 253-61.
4. Uhac I, Kovac Z, Muhvic-Urek M, Kovacevic D, Franciskovic T, Simunovic-Soskic M. The prevalence of temporomandibular disorders in war veterans with post-traumatic stress disorder. Mil Med. 2006; 171: 1147-9.
5. Uhac I, Kovac Z, Valentic-Peruzovic M, Juretic M, Moro LJ, Grzic R. The influence of war stress on the prevalence of signs and symptoms of temporomandibular disorders. J Oral Rehabil. 2003; 30: 211-7.
6. Carvalho AL, Cury AA, Garcia RC. Prevalence of bruxism and emotional stress and the association between them in Brazilian police officers. Braz Oral Res. 2008; 22: 31-5.
7. Ekberg E, Vallon D, Nilner M. The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial. J Orofac Pain. 2003; 17: 133-9.
8. Weggen T, Schindler H, Kordass B, Hugger A. Clinical and electromyographic follow-up of myofascial pain patients treated with two types of oral splint: a randomized controlled pilot study. Int J Comput Dent. 2013; 16: 209-24.
9. Hugger S, Schindler H, Kordass B, Hugger A. Surface EMG of the masticatory muscles. (Part 4): Effects of occlusal splints and other treatment modalities. Int J Comput Dent. 2013; 16: 225-39.
10. Hugger S, Schindler H, Kordass B, Hugger A. Clinical relevance of surface EMG of the masticatory muscles. (Part 1): Resting activity, maximal and submaximal v
11. Landulpho AB, E Silva WA, E Silva FA, Vitti M. Electromyographic evaluation of masseter and anterior temporalis muscles in patients with temporomandibular disorders following interocclusal appliance treatment. J Oral Rehabil. 2004; 31: 95-8.
12. Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992; 6: 301-55.
13. Alanen P. Occlusion and temporomandibular disorders (TMD): still unsolved question? J Dent Res. 2002; 81: 518-9.
14. Suvinen TI, Kemppainen P. Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects. J Oral Rehabil. 2007; 34: 631-44.
15. Territo L, Vetter HJ. Stress and Police Personnel. J Police Sci Admin. 1981; 9: 195-208.
16. Zhang F, Wang X, Dong J, Zhang J, Lü Y. Effect of occlusal splints for the management of patients with myofascial pain: a randomized, controlled, double-blind study. Chin Med J. 2013; 126: 2270-5.
17. Wood GN. Centric relation and the treatment position in rehabilitating occlusions: a physiologic approach. Part II: The treatment position. J Prosthet Dent. 1988; 60: 15-8.
18. Alajbeg I, Gikiæ M, Valentiæ-Peruzoviæ M. Changes in pain intensity and oral health-related quality of life in patients with temporomandibular disorders during stabilization splint therapy-a pilot study. Acta Clin Croat. 2014; 53: 7-16.
19. Forssell H, Kalso E, Koskela P, Vehmanen R, Puukka P, Alanen P. Occlusal treatments in temporomandibular disorders: a qualitative systematic review of randomized controlled trials. Pain. 1999; 83: 549-60.
20. Chen T, Liao T, Zhan R, Wu L. Effect of two different kinds of occlusal splints on temporomandibular disorders. Shanghai Kou Qiang Yi Xue. 2013; 22: 547-50.
21. Sheikholeslam A, Holmgren K, Riise C. Therapeutic effects of the plane occlusal splint on signs and symptoms of craniomandibular disorders in patients with nocturnal bruxism. J Oral Rehabil. 1993; 20: 473-82.
22. Dimitroulis G, Gremillion H, Dolwick M, Walter J. Temporomandibular disorders. 2. Non-surgical treatment. Aust Dent J. 1995; 40: 372-6.
23. Visser A, Naeije M, Hansson TL. The temporal/masseter co-contraction: an electromyographic and clinical evaluation of short-term stabilization splint therapy in myogenous CMD patients. J Oral Rehabil. 1995; 22: 387-9.
24. Kawazoe Y, Kotani H, Hamada T, Yamada S. Effect of occlusal splints on the electromyographic activies of masseter muscles during maximum clenching in patients with myofascial pain-dysfunction syndrome J Prosthet Dent. 1980; 43: 578-80.
25. Lund JP, Donga R, Widmer CG, Stohler CS. The pain-adaptation model: a discussion of the relationship between chronic musculoskeletal pain and motor activity. Can J Physiol Pharmacol. 1991; 69: 683-94.
26. Proff P, Richter EJ, Blens T, Fanghanel J, Hutzen D, Kordass B et al. A michigan-type occlusal splint with spring-loaded mandibular protrusion functionality for treatment of anterior disk dislocation with reduction. Ann Anat. 2007; 189: 362-6.
27. Ciancaglini R, Gherlone EF, Radaelli G. Unilateral temporomandibular disorder and asymmetry of occlusal contacts. J Prosthet Dent. 2003; 89: 180-5.
28. Sato S, Nasu F, Motegi K. Analysis of post-treatment electromyographs in patients with non-reducing disc displacement of the temporomandibular joint. J Oral Rehabil. 2002; 29: 1126-30.
29. Vianna-Lara MS, Caria PH, Tosello Dde O, Lara F, Amorim MM. Electromyographic activity of masseter and temporal muscles with different facial types. Angle Orthod. 2009; 79: 515-20.
30. Vitti M. Electromyographic analysis of the musculus temporal in basic movements of the jaw. Electromyography. 1971; 3(Suppl 4): 389.
 Correspondence:
Correspondence:
Paulo Henrique Ferreira Caria
Faculdade de Odontologia de Piracicaba,
UNICAMP - Caixa Postal 52
CEP: 13414-903, Piracicaba, SP, Brasil
E-mail: phcaria@fop.unicamp.br
Received for publication: September 01, 2014
Accepted: December 05, 2014













