Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.14 no.1 Piracicaba Jan./Mar. 2015
ORIGINAL ARTICLE
Civil liability related to imaging exams in Brazil
Mathias Pante Fontana I; Gabriela Salatino Liedke I; Helena da Silveira Fontoura II; Heraldo Luis Dias da Silveira I; Heloísa Emilia Dias da Silveira I
I Universidade Federal do Rio Grande do Sul - UFRGS, Dental School, Department of Surgery and Orthopedics, Porto Alegre, RS, Brazil
II Universidade Federal do Rio Grande do Sul - UFRGS, School of Law, Porto Alegre, RS, Brazil
ABSTRACT
Aim: To analyze all court lawsuits in Brazil in relation to civil liability involving radiographic and tomographic images up to February 2014. Methods: All Brazilian courts were surveyed for "civil liability, "error, "radiology, "radiography, and "tomography, returning 3923 second-instance lawsuits. Out of them were excluded labor legislation, health insurance coverage of radiological examinations, and criminal liability cases and 359 were selected. Compliance with expert reports, involvement of imaging exams, the defendant professional, the reasons of claims and convictions, and indemnity were evaluated. Results: Of the 359 selected lawsuits, physicians were defendants in 71%, radiologist physicians in 10.6% and dentists in 18.4%. The prevalence of physicians found liable was related to the lack or delay in requesting the imaging exams (49.6%), and among radiologist physicians, misdiagnosis (47.1%). Considering the dentists, imaging exams had mostly an indirect involvement, and failure of the proposed treatment (73.8%) was the most prevalent cause of dentists found liable; no radiologist was sued. Regarding indemnity, 50% of lawsuits resulted in compensation up to R$ 20,000 (US$ 8,583). Conclusions: Misdiagnosis was the main cause of claims and radiologists were found liable. The medical field showed the largest absolute number of claims and physicians were found liable, but the highest proportion was directed to dentists.
Keywords: damage liability; jurisprudence; malpractice; tomography; radiography.
Introduction
Diagnostic radiology focuses on the detection of abnormalities in an imaging examination and their accurate diagnoses. Discrepancies and misinterpretations were shown when physicians' and radiologists' interpretation were compared1; suggesting that image acquisition and interpretation should be the competency of a radiologist. This emphasizes the importance of expert knowledge for adequate image interpretation, particularly with respect to more advanced techniques.
The development of radiology services along with the increase in litigation, especially in medicine, has increased the radiologist's responsibilities2-4. Allegations of missed radiologic diagnosis accounted for an average of 42% of all cases over a 20-year period, according to a study conducted in the state of Illinois, USA4. However, the failure to detect abnormalities is not necessarily malpractice: negligence occurs when the error violates the basic principles of interpretation or is a substantial cause of injury to patient's health5-6.
According to the American College of Radiology, an official report must be made and filed following any examination. Where findings require immediate intervention, the report should be submitted to the referring physician7. Failure to communicate the results of the exam directly to the patient in case of selfreferral or if the physician cannot be reached, has been cause for lawsuits against radiologists2.
Lawsuits have also grown against dentists around the world8-16. A study in Germany found that dentistry was the second most frequent discipline confronted with claims of medical malpractice (16.4%), following surgery accidents and orthopedics (30.2%)17. Furthermore, surveys conducted in Denmark and the United Kingdom showed a condemnation ratio of 43% and 54%, respectively, in cases involving dentists18-19. In Brazil, complaints to the Regional Councils of Dentistry showed Orthodontics, Prosthodontics, Oral and maxillofacial surgery and implants as the specialties with the largest number of claims against dentists20-21. This trend was also observed in Brazilian courts, and has shown a growth tendency in the last years22. Even though no studies dealing with lawsuits involving dental radiologists have been found, dentists are intimately linked to imaging exams, and their acquisition, interpretation and storage are the dentists' responsibility23-24.
Brazil represents the largest population, economy, and land area of South America, but its unique reality seldom stands out in global policy. Bearing in mind the importance of the topic, as well as the growth of reports in the literature, the aim of this study was to analyze court decisions in Brazil relative to liability involving radiographic and tomographic images. This study focuses on the mentioned imaging exams because of the higher frequency of use in both areas of interest, allowing comparisons between the medical and dental fields.
Material and methods
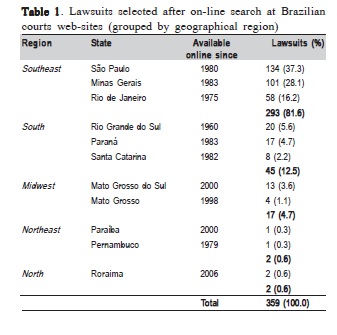
The official web pages of all Brazilian courts, available online up to February 2014, were surveyed for all second instance decisions involving civil liability and radiographic or tomographic images. The researched period varied according to the digitalization of the lawsuits in each Brazilian state (Table 1). The search strategy, comprising the terms "civil liability, "error, "radiology, "radiography, and "tomography, yielded 3923 lawsuits (Figure 1). The wide variety of terms used here aimed to identify the highest number of claims, since lawsuit language often lacks specific keywords or expressions regarding scientific vocabulary.
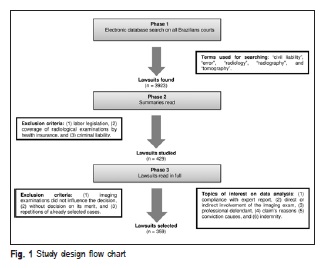
Two oral radiologists and a senior year law student examined the summary of each lawsuit, containing the claim and the verdict report. Claims dealing with labor legislation, coverage of radiological exams by health insurance and criminal liability were excluded. The remaining 429 lawsuits were reviewed in full, and those in which imaging exams did not influence the decision, those without decision on their merits and repetitions of previously selected cases were excluded. The final selection comprised 359 lawsuits that contemplated professional or entity civil liability related to radiographic or tomographic examination. Each one was thoroughly studied regarding the claim and its decision, as well as its legislative content, to allow grouping of data.
Data analysis: Six topics of interest were observed in each lawsuit: compliance with expert reports, direct or indirect involvement of the imaging exam, the defendant (professional), the claim's reasons, conviction causes and indemnity. Direct involvement was indicated when the image was the reason to instigate the lawsuit. Where the imaging exam was a probative element and not the merit of the claim, were considered as indirect involvement cases.
The defendants were divided into four groups: physicians of any specialty other than radiology, hospitals, and medical clinics (Group 1); radiologist physicians, radiology services linked to hospitals, and private radiology clinics (Group 2); dentists of any specialty other than radiology and dental clinics (Group 3); dentists and specialists in radiology and dental radiology clinics (Group 4).
The settlement in both material and moral harm, if present, was computed, and the amount paid was calculated in Brazilian Reais (R$) and U.S. Dollars (US$), updated to the completion of data collection. To allow pooling of data, the paid indemnity was categorized into six ranges of values. When the conviction also involved the payment of a monthly pension to the plaintiff, the amount to be paid and the duration of payments were also registered.
The institutional Research Committee approved the study (n. 20753). Data retrieved from the webpages of the courts are public and therefore Ethics Committee submission was waived. Data analysis was performed with the SPSS version 13.0 software package (SPSS, Chicago, IL, USA).
Results
Among the 27 Brazilian states, 11 featured claims involving imaging exams (Table 1). The South and Southeast regions accounted for 94.1% of total occurrences. Out of the studied 359 lawsuits, the expert report, whenever present was upheld by the judge in 96% of cases.
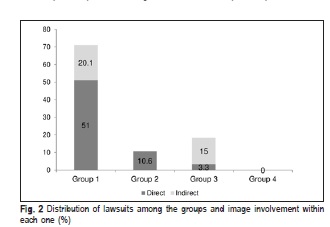
Image involvement was considered direct in 231 (64.3%) cases and indirect in 128 (35.7%) cases. Claims that gave rise to the lawsuits classified as direct involvement included misdiagnosis, lack of or delay in requesting the imaging exam, exchange of exams, failure in performance or in quality of the exam, complications in the use of contrast, and complications with the device. Treatment failure, on the other hand, was considered an indirect image involvement claim. Group 1 had defendants in 255 cases (71%), Group 2 in 38 cases (10.6%) and Group 3 in 66 cases (18.4%). No cases against Group 4 were found. Figure 2 shows the distribution of the type of image involvement among the groups.
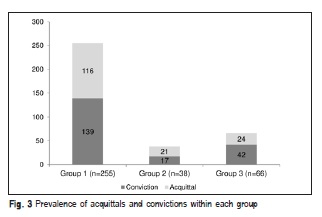
Figure 3 shows the prevalence of lawsuits in each group, and the proportion of acquittals and convictions within each case. In 198 cases (55.2%), the professionals or health entities involved were convicted, including 139 cases (54.5% of the group total) in Group 1, 17 cases (44.7% of the group total) in Group 2, and 42 cases (63.6% of the group total) in Group 3.
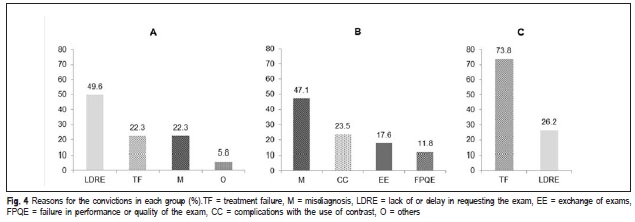
Figure 4 shows the reasons that gave rise to convictions in relation to the professionals involved in each group. The highest frequency of convictions in Group 1 related to the lack of an imaging exam or delay in requesting it (49.6%), while in Group 2 the main reason was misdiagnosis (47.1%). On the other hand, most convictions in Group 3 were due to the failure of a proposed treatment (73.8%); here, imaging exams were used as evidence in the lawsuit. Only two dentists were sued for misdiagnosis, but none was found liable.
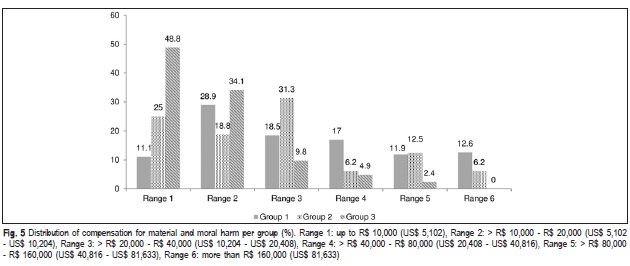
Regarding the quantum of indemnity, 49.5% convictions resulted in compensation for damages amounting up to R$ 20,000 (US$ 8,583), with compensation in 9.4% of cases exceeding R$ 160,000 (US$ 68,670). Group 1 had the highest amount of compensations, reaching R$ 715,116.30 (US$ 306,916.90). Figure 5 shows the distribution of compensation for material and moral harm per group. Twenty-seven convicted professionals from Group 1 (19.6%) and two from Group 2 (12.5%) were sentenced to pay a monthly pension.
Discussion
Currently, physicians and dentists have increased responsibilities regarding the request for, performance and interpretation of imaging exams. Considering the increase of claims against these professionals, studies conducted in the United States, United Kingdom, Australia and Italy warn about the legal implications of errors in radiology, and suggest solutions to minimize the number of faults and their consequences2,4-6,24-26. Lacking information about this reality in Brazil, the aim of this study was to analyze court decisions covering imaging exams in medicine and dentistry. The study specifically addressed radiographic and tomographic images to allow comparison between the two areas, excluding other exams, such as ultrasonography, and mammography, which are seldom or not performed by dentists.
The data search strategy selected 359 lawsuits, 94.1% of which were cases from Southern and Southeastern Brazil, following the country's size and development in those regions.
The main reason for litigation against non-radiologist physicians and hospitals were the lack or delay in requesting the imaging exam (38.8%). The absence of a thorough investigation of a patient's complaint that could be assessed by specific exam, or the excessive time spend to request it, causing sequelae or even death, were responsible for the conviction of 49.6% professionals from Group 1.
Data from the United States showed that diagnostic error was responsible for 42% of lawsuits involving radiologists4. In the present study, 26.7% of the claims against Group 1 and 52.6% against Group 2 were due to misdiagnosis. Among radiologists, 47.1% of them resulted in conviction. There were two false-negative and three false-positive cases of cancer. In three other cases, the diagnoses were a false negative for fracture, bleeding, and presence of a foreign body. Driscoll, Halpenny and Guiney25 (2012) also observed that most errors were due to false-negative diagnoses, and occurred more frequently in radiographs (46.85%), followed by computed tomography (41.44%).
Radiological error is multifactorial, and could arise from poor technique, failures of perception, lack of knowledge and misjudgment27. An objective classification suggests dividing cases into procedural or diagnostic errors; errors can also be classified in observer errors, interpretation errors, failure to suggest the next appropriate procedure, and failure to communicate in a timely and clinically appropriate manner6,26,28. Perception error is the failure to identify an abnormal radiological finding, while interpretation error is the failure to correctly interpret a radiological abnormality5. Perception errors may be due to human fallibility, and can be explained by external factors (excessive time load and inappropriate workplace), technical mistakes, presence of abnormalities that were not under investigation, and by different lesions found in the same exam. On the other hand, interpretation errors may be influenced by inexperience, insufficient knowledge, or underestimation of radiographic signs that could lead to the correct diagnosis5,29.
Failures in detection are generally attributed to the subtlety of an abnormality, low incidence, or its poor definition: when the incidence of a particular disease is very low, most cases are correctly diagnosed (true negatives), but very rarely the lesion is present and not detected (false positives)28,30. However, the phenomenon of nonidentification of "obvious and easily recognized abnormalities in a second analysis was not yet satisfactorily explained. Misinterpretations may result in harm to the patient and legal consequences to the professional. For this reason, errors are often kept secret. Even though disclosure is important to the patient, reducing suffering, increasing quality of care and limiting the consequences of damage, there seems to be no evidence that it modifies the likelihood that the professional will be sued26.
In the present study, the second largest cause of convictions in Group 2 was due to complications arising from the use of contrast. The convictions were mainly due to the failure in obtaining informed consent, and failing to investigate the medical history of patients, which could avoid the risks involved with the procedure. In one case, a minor with microencephaly underwent a computed tomography scan and had complications triggered by the use of contrast, which placed the minor in a vegetative state. The radiologic clinic was fined in R$ 89,672.85 (US$ 38,486.20) as moral harm, and a monthly pension was paid to the victim until age 60. There is no consensus in the literature regarding the requirement of informed consent to the use of contrast in imaging exams, and the decision to obtain it or not from the patient depends on local legislation and policy of the hospital31. In the authors' view, this case suggests that informed consent should be adopted by health professionals to avoid the risk of legal complications, corroborating Mavroforou, et al.32 (2003).
Imaging exams, when properly requested after a careful clinical investigation, help establishing the diagnosis, treatment plan and follow-up routine. In this study, 27.8% of claims against Group 1 and 75.8% against Group 3 were due to treatment failure, generating 22.3% and 73.8% of convictions, respectively. The most litigated areas in dentistry were orthodontics, surgery, endodontics and implantology, in which imaging exams play an important role regarding the planning and monitoring of cases, corroborating previous findings in the literature9-12,14-16,18,20-22. Moreover, 26.2% of convictions in Group 3 were due to the lack of a request for an imaging exam, mainly in cases of tooth extractions without radiograph analysis, dental implant surgeries made unsuccessful by the lack of tomographic planning, and orthodontic movement resulting in root resorption that was not diagnosed and monitored. These results emphasize the importance of imaging exams requested by the professional, when appropriate, to start and follow-up treatment. This behavior allows proving that the professional acted with all expected carefulness and used the best techniques available to the case. The knowledge regarding ethical and legal implications of exercising a profession is fundamental33. Giffoni Filho et al.21 (2013) suggest that the study of ethics and bioethics should be part of the dental curriculum, to teach the student legal aspects of the career and to reduce future infractions.
Most lawsuits against health professionals included an expert report performed by a physician or dentist; when available, they were upheld by the judge in 96% of cases. However, complying with the report is the judge's choice, according to his own conviction. Additionally, the use of imaging exams as evidence in lawsuits involving dentists is common and its non-presentation when otherwise indicated for the correct diagnosis and treatment may suggest condemnation of the professional.
In this study, most of the claims, in absolute numbers, were against those in the medical field. However, dentists showed a higher frequency of convictions. Comparing indemnity ranges, higher amounts were paid by Groups 1 and 2, and Group 3 had 48.8% of convicted professional within the first range.
The present study has some limitations. The search was limited to digitized decisions of lawsuits, which vary according to the region (Table 1). Since it is a time consuming and ongoing process, not all Brazilian states retrieved results. In addition, only second instance decisions were included, since they generally are the final judgment of the court, except in case of extraordinary appeals. However, while only one country was studied, Brazil is a continental country, representing the largest population, economy and land area of South America. Other studies have also assessed the legal situation in a single country4,17-19,24-25, each one with its specific legal structure. Law and liability depends on each country's construction doctrine and jurisprudence. Most of Brazilian courts understand the duty assumed by health professionals as being of means and not of results, except in cases of aesthetic treatments. The duty is not to cure the patient, but to use the most appropriate treatment according to the state of science, carefully and consciously. Nevertheless, in some cases the judges considered guilty those professionals who have not achieved the results expected by the patients. In other lawsuits, healthcare entities and radiology clinics were sentenced due to strict liability, based on Article 14 of the Brazilian Consumer Defense Code34, which states that the service provider must respond, regardless the presence of guilt, to compensate for damages caused to the patient by faults in provided services, as well as those secondary to inadequate or insufficient information pertaining to the risks inherent in the provided care. Strict liability, however, does not apply to liberal professionals.
Reasons for conviction in cases directly or indirectly involving imaging exams varied according to the studied occupational group. Misdiagnosis was the highest cause of claims and convictions against radiologists and radiologic clinics. Despite the largest number of physicians accused and convicted, the highest proportion of convictions occurred among dentists.
References
1. Alfaro D, Levitt MA, English DK, Williams V, Eisenberg R. Accuracy of interpretation of cranial computed tomography scans in an emergency medicine residency program. Ann Emerg Med. 1995; 25: 169-74. [ Links ]
2. Berlin L. Are radiologists contracted by third parties to interpret radiographs liable for not communicating results directly to patients? AJR Am J Roentgenol. 2002; 178: 27-33.
3. Smith JJ, Berlin L. The infected or substance abuse-impaired radiologist. AJR Am J Roentgenol. 2002; 178: 567-71.
4. Berlin L, Berlin JW. Malpractice and radiologists in Cook County, IL: trends in 20 years of litigation. AJR Am J Roentgenol. 1995; 165: 781-8.
5. Olivetti L, Fileni A, De Stefano F, Cazzulani A, Battaglia G, Pescarini L. The legal implications of error in radiology. Radiol Med. 2008; 113: 599- 608.
6. Pinto A, Brunese L, Pinto F, Reali R, Daniele S, Romano L. The concept of error and malpractice in radiology. Semin Ultrasound CT MR. 2012; 33: 275-9.
7. American College of Radiology. Practice guideline for communication of diagnostic imaging findings - Resolution 11. Reston: ACR, 2010. 7p.
8. Baker P, Needleman I. Risk management in clinical practice. Part 10. Periodontology. Br Dent J. 2010; 209: 557-65.
9. Curley AW. The law and dentoalveolar complications: trends and controversies. Oral Maxillofac Surg Clin North Am. 2011; 23: 475-84.
10. Givol N, Rosen E, Bjorndal L, Taschieri S, Ofec R, Tsesis I. Medico-legal aspects of altered sensation following endodontic treatment: a retrospective case series. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112: 126-31.
11. Henderson SJ. Risk management in clinical practice. Part 11. Oral surgery. Br Dent J. 2011; 210: 17-23.
12. Maglad AS, Wassell RW, Barclay SC, Walls AW. Risk management in clinical practice. Part 3. Crowns and bridges. Br Dent J. 2010; 209: 115-22.
13. Manfredini D, Bucci MB, Montagna F, Guarda-Nardini L. Temporomandibular disorders assessment: medicolegal considerations in the evidence-based era. J Oral Rehabil. 2011; 38: 101-19.
14. Mizrahi E. Risk management in clinical practice. Part 7. Dento-legal aspects of orthodontic practice. Br Dent J. 2010; 209: 381-90.
15. Rosen E, Tsesis I, Tamse A, Bjorndal L, Taschieri S, Givol N. Medicolegal aspects of vertical root fractures in root filled teeth. Int Endod J. 2012; 45: 7-11.
16. Webber J. Risk management in clinical practice. Part 4. Endodontics. Br Dent J. 2010; 209: 161-70.
17. Knaak JP, Parzeller M. Court decisions on medical malpractice. Int J Legal Med. 2014; 128: 1049-57.
18. Bjorndal L, Reit C. Endodontic malpractice claims in Denmark 1995-2004. Int Endod J. 2008; 41: 1059-65.
19. Gulati A, Herd MK, Nimako M, Anand R, Brennan PA. Litigation in National Health Service oral and maxillofacial surgery: review of the last 15 years. Br J Oral Maxillofac Surg. 2012; 50: 385-8.
20. Neta NBD, Torres PF, Nogueira LT, Carvalho CMRS. Civil liability of dentists based on reports filed to the Regional Council of Dentistry. Braz J Oral Sci. 2011; 10: 109-12.
21. Giffoni Filho RIR, Menezes LMB, Oliveira PMC, Chaves MG. Labor disputes on grounds of discipline in a Brazilian regional council of dentistry: a critical analysis. Rev Gaúcha Odontol. 2013; 61: 245-53.
22. De Paula FJ. Survey on jurisprudences of civil liability lawsuits against dentists in Brazilian Courts via the Internet. #91;Doctor's thesis#93;. São Paulo: University of São Paulo; 2007. 142p.
23. Dym H. Risk management in the dental office. Dent Clin North Am. 2012; 56: 113-20, viii.
24. Wright B. Contemporary medico-legal dental radiology. Aust Dent J. 2012; 57 (suppl 1): 9-15.
25. Driscoll DO, Halpenny D, Guiney M. Radiological error - an early assessment of departmental radiology discrepancy meetings. Ir Med J. 2012; 105: 172-4.
26. Magnavita N, Magnavita G, Fileni A, Bergamaschi A. Ethical problems in radiology: medical error and disclosure. Radiol Med. 2009; 114: 1345-55.
27. Pinto A, Acampora C, Pinto F, Kourdioukova E, Romano L, Verstraete K. Learning from diagnostic errors: a good way to improve education in radiology. Eur J Radiol. 2011; 78: 372-6.
28. Robinson PJ. Radiology's Achilles' heel: error and variation in the interpretation of the Rontgen image. Br J Radiol. 1997; 70: 1085-98.
29. Golfieri R, Pescarini L, Fileni A, Silverio R, Saccavini C, Visconti D, et al. Clinical Risk Management in radiology. Part I: general background and types of error and their prevention. Radiol Med. 2010; 115: 1121-46.
30. Toms AP. The war on terror and radiological error? Clin Radiol. 2010; 65: 666-8.
31. Iserson KV. Is informed consent required for the administration of intravenous contrast and similar clinical procedures? Ann Emerg Med. 2007; 49: 231-3.
32. Mavroforou A, Giannoukas A, Mavrophoros D, Michalodimitrakis E. Physicians' liability in interventional radiology and endovascular therapy. Eur J Radiol. 2003; 46: 240-3.
33. Pereira MMAF, Silva RF, Maia LVA, Silva RHA, Daruge Junior E, Paranhos LR. Perception of dental surgeons on the ethical and legal aspects of exercising their profession as personal and corporate entities. Braz J Oral Sci. 2011; 10: 246-9.
34. Brazil. Law Nº 8.078, of 1990 Sep 11. Code of Consumer Protection. Brasilia: Presidency of Brazil. #91;updated 2013 Jun 17; cited 2014 Feb 11#93;. Available from: http://www.planalto.gov.br/ccivil_03/leis/l8078.htm.
 Correspondence:
Correspondence:
Heloisa Emilia Dias da Silveira
Faculdade de Odontologia - Universidade Federal do Rio Grande do Sul
Rua Ramiro Barcelos 2492.
CEP: 90035-003 Porto Alegre, RS, Brasil
E-mail: heloisa.silveira@ufrgs.br
Received for publication: December 16, 2014
Accepted: March 04, 2015













