Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.14 no.2 Piracicaba Abr./Jun. 2015
ORIGINAL ARTICLE
Pharyngeal airspace in patients undergoing orthognathic surgery for mandibular advancement
Guilherme dos Santos TrentoI; Fernando Anunziato Ogg de Salles SantosI; Leandro Eduardo KlüppelI; Delson João da CostaI; Nelson Luis Barbosa RebellatoI; Rafaela ScariotI,II
I Universidade Federal do Paraná – UFPR, School of Dentistry, Department of Stomatology, Area of Oral and Maxillofacial Surgery, Curitiba, PR, Brazil
II Universidade Positivo - UP, School of Dentistry, Area of Oral and Maxillofacial Surgery, Curitiba, PR, Brazil
Abstract
Aim: To evaluate the increase of pharyngeal airway space (PAS) in patients undergoing mandibular advancement. Methods: A retrospective cross-sectional study was performed in thirteen patients who underwent mandibular advancement and were evaluated by cephalometric tracing in pre and postoperative lateral radiographs. In cephalometric tracing, the PAS was assessed by measuring the distance from the lower portion of the soft palate to the posterior pharyngeal wall (UP-PHW) and from the tongue base to the posterior pharyngeal wall (TB-PHW). Results: Patients' age ranged from 22 to 42 years with an average of 28.54 ± 2.23 years. A preoperative mean of 9.20 ± 4.56 mm in the UP-PHW measure and 10.53 ± 5.84 mm in the TB-PHW measure were obtained. The mean values found for those measurements in the postoperative period were 11.61 mm and 13.95 mm, respectively. There was an average increase of 2.4 mm in the UP-PHW and of 2.95 mm in the TB-PHW. The mean mandibular advancement in evaluated patients was 5 mm. There was no statistical correlation between PAS increase and the amount of mandibular advancement for UP-PHW (p=0.058) and TB-PHW (p=0.53), as there was no such correlation either between PAS increase and the age of patients for UP-PHW (p=0.16) and TB-PHW (p=0.26). A greater effect of the retrolingual dimension in mandibular advancement was observed, with an average increase of 24.52% while in the retropalatal dimension an average increase of 20.75% was obtained. Conclusions: Surgical advancement of the mandible increases the size of the pharyngeal airway space.
Keywords: mandible; pharynx; tongue; orthognathic surgery.
Introduction
Orthognathic surgery is one of the most used procedures for treatment and correction of dentofacial deformities. Changes in facial skeleton produced by the surgery affect the bones of the facial skeleton and their relationship with soft tissues. An aspect to be considered is the impact of the skeleton movement on the pharyngeal airspace (PAS) of patients undergoing orthognathic surgery1-2.
In this context, it is observed that the movement of the facial skeleton produces changes in the tension of the soft tissues and muscles inserted in the jaw. Soft palate, tongue, hyoid bone and associated musculature are directly or indirectly inserted in the jaw, therefore movements in those structures induce alterations in the oral and nasal cavity and on the PAS1-5.
Studies1,4-5 have been conducted to quantify the regular measurements of PAS, as well as the measurements in patients diagnosed with obstructive sleep apnea (OSA). Those studies are based on lateral cephalometric analysis1,6 and indicate that the most significant anatomic variation is the lower position of the hyoid bone and consequently the lower position of the tongue base in OSA patients4-5,7.
Surgeries for mandibular advancement, bimaxillary advancement and counterclockwise rotation of the occlusal plane of the maxillomandibular complex promote the increase in PAS bringing improvements in the respiratory status of patients with OSA. Arikasa et al.8, in 2014, argue that orthognathic surgery increases airway space and improves OSA. Faria et al.1, in 2013, stated that mandibular advancement significantly provokes an advancement of the lingual and suprahyoid increasing the inter-maxillary space.
Mehra et al.9, in 2001, showed a 76% increase in the retrolingual and oropharyngeal air dimensions in relation to a certain amount of mandibular advancement. On the other hand, some studies10-12 have reported that surgery for maxillomandibular advancement (7.5 mm mandibular advancement) with counterclockwise rotation (4.2º out of decrease in angulation of occlusal plane) increases 3.5 mm on the retropalatal region and 5.7 mm on the retrolingual region of the PAS. Given the potential for soft tissue adaptation and post-surgical recurrence of skeletal parts, it is important to know whether the changes produced by surgery in PAS will remain stable over time.
Yu et al.13 conducted a retrospective study with data from 26 patients of orthognathic surgery in which there were 16 mandibular advancements and 10 maxillomandibular advancements. Preoperative radiographs, immediate postoperative and late postoperative (15 months) lateral radiographs were evaluated. The patients were divided into two groups: group 1 comprised patients with preoperative PAS measure greater than 11 mm, and group 2 those with preoperative PAS measure under 11 mm. Patients from group 1, who underwent mandible advancement surgery, showed a bigger change in the dimension of their airways with an average of 3.5 ± 3.2 mm aspect ratio of increased airway, and the mandibular advancement reached a 0.62:1 ratio in late postoperative period13. Such results are similar to those found by other authors.10-12 Patients from group 2 reported minor changes, with a mean 0.9 ± 3.6 mm increase in PAS, measured in the late postoperative period, with a ratio between mandibular advancement and gain of airway dimension of approximately 0.19:113.
Within the aforementioned context, this study aims to quantify and correlate the changes of the PAS in patients undergoing orthognathic surgery for mandibular advancement in the Department of Oral and Maxillofacial Surgery of the Federal University of Paraná.
Material and methods
Sample selection
Records of 13 patients from the Department undergoing orthognathic surgery of mandibular advancement were selected in descending chronological order. In order to be part of the sample, the patient had to present mandibular retrognathia and to have undergone orthognathic surgery to advance the mandible with bilateral sagittal split osteotomy and stable internal fixation with plates and/or screws. The records should contain pre and postoperative lateral radiographs of the patients in the study.
This study was approved by the Ethics and Research Committee of the Department of Health Sciences, Federal University of Paraná, Brazil, with registration CEP/SD: 934.059.10.05 and CAAE: 0034.0.91.000-10.
Inclusion criteria
Patients with mandibular retrognathia who underwent orthognathic surgery for mandibular advancement with bilateral sagittal split osteotomy and stable internal fixation with plates and/or screws. The records should contain pre and postoperative lateral radiographs of the patients included in this study.
Exclusion criteria
Patients who underwent orthognathic surgery for mandibular advancement with vertical osteotomy. Records that do not contain pre and postoperative lateral radiographs or contain low-quality radiographs leading to an erroneous diagnosis.
Data collection
A single researcher collected the data. In all the charts, data such as gender and age of the patient included in the study were evaluated. Data were tabulated in a sheet for frequency analysis. In addition, lateral radiographs from the medical records of the patients were evaluated (one week before surgery and three months after surgery).
The lateral radiographs were obtained by an Orthophos® radiological equipment model (Siemens AG, Berlin, Germany) in the Dental Radiology department of the Federal University of Paraná. All the radiographs were taken with the patient in constant head position with the Frankfurt plane parallel to the ground. The radiographic interpretation was performed in a dark room with an appropriate light box. The radiographs were evaluated by the performance of cephalometric tracing while outlining craniofacial structures and the cephalometric points of interest for the assessment of changes introduced by orthognathic surgery in PAS. The pre and postoperative radiographs were drawn three times with a one-week interval between measurements in order to reduce the memory bias. In order to evaluate the reliability of the obtained data, the intraclass correlation coefficient was calculated (CCI=0.977) demonstrating that the measurements were reliable for the research.
The cephalometric tracing was performed by outlining all the important craniofacial structures for the study. Then, we assessed the amount of mandibular advancement produced by measuring the distance between the pogonion point and the nasion perpendicular line in pre and postoperative radiographs.
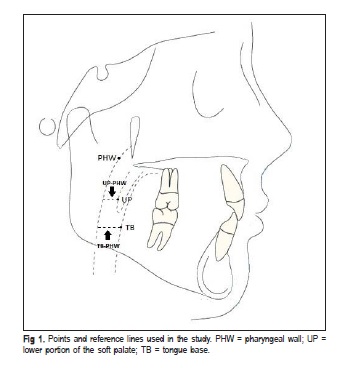
The dimension of the PAS was evaluated by two lines parallel to the Frankfurt plane, one passing by the gonion (Go) while intersecting the base of the tongue and the posterior pharyngeal wall (PHW-TB), and another drawn from the lower portion of the soft palate to the posterior pharyngeal wall (UP-PHW) (Figure 1). Afterwards, the anteroposterior dimension of the PAS from those lines on lateral radiographs was measured with a digital caliper (Vonder®, Curitiba, PR, Brazil).
Statistical analysis
Data were recorded on individual sheets and tabulated using Microsoft Excel 2007® software for Windows XP. Furthermore, correlations between variables were performed with statistical tests (SPSS for WINDOWS 15.0 – SPSS Inc., Chicago, IL, USA) with a confidence interval of 95%.
Results
Thirteen patients, twelve female and one male were included in the survey.
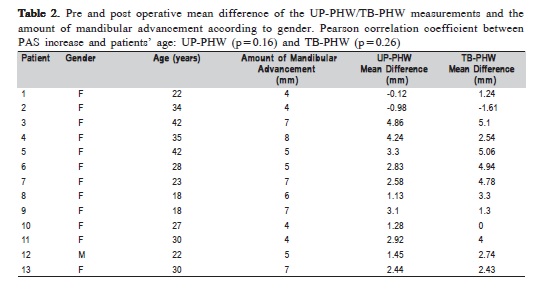
Patients' age ranged from 22 to 42 years with an average of 28.54 ± 2.23 years. No statistically significant correlation was observed between the increase of PAS and the age of patients undergoing surgery for mandible advancement in UP-PHW (p = 0.16) and TB-PHW (p=0.26) measurements by the Pearson's correlation coefficient.
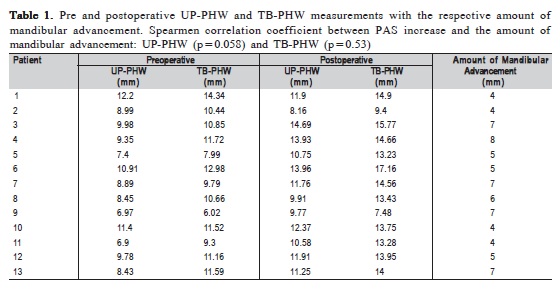
The values found for PAS to measure UP-PHW and TBPHW, both pre and postoperatively, and the amount of mandibular advancement is shown in Table 1. The PAS average for UP-PHW was 9.20 ± 4.56 mm and 11.61 ± 5.14 mm pre and postoperatively, respectively. In the preoperative period, the PAS average for TB-PHW was 10.53 ± 5.84 mm. The postoperative TB-PHW mean was 13.95 mm (11.97 – 15.01). A greater effect in the retrolingual dimension was observed by mandibular advancement with an average of 24.52%, while an average increase of 20.75% was obtained in the retropalatal measure.
The mean mandibular advancement in patients undergoing surgery was 5 mm (4 - 8). The average increase of the UPPHW dimension was 2.4 ± 0.4 mm and for the TB-PHW measurement it was 2.95 ± 0.5 mm. There was no statistically significant correlation between mandibular advancement and PAS increase in both the UP-PHW (p=0.058) and TB-PHW (p=0.53) measurements by the Spearman correlation coefficient. The impact of surgical advancement of the mandible on the PAS is very variable and unpredictable, because patients with larger mandibular advancement do not always have the greatest impact on PAS. Gender, age, amount of advancement of the mandible and the difference in PAS for both measurements are shown in Table 2.
Discussion
Dentofacial deformities are congenital or growth malformations during the development which may cause functional and aesthetic problems2-3. Changes in the airways after orthognathic surgery have been the subject of great interest in recent years1,4,8,13. Some studies have shown that repositioning of both the maxilla and mandible generate changes in pharyngeal airspace10,13. Moreover, cases of respiratory disorders after mandibular setback have been reported related to narrowing of the pharyngeal airspace1.
The PAS may become reduced under various conditions including obesity, hypertrophy of the tonsils, adenoids, macroglossia and decrease in the size of the jaws. A narrow PAS causes increased resistance to airflow accounting for possible respiratory disorders including obstructive sleep apnea and snoring14.
The final study sample included twelve females and one male patient, which made it impossible to conduct any statistical test to compare the effects of mandible advancement surgery in different genders.
The average age of patients participating in the survey was 28.54 years; however, there was no statistically significant correlation between changes in PAS and the age at which patients underwent the procedure, probably due to the small amplitude of the age range of patients included in the study.
Rilley et al.10, in 1993, reported an increase of the PAS dimension with an average of 5 to 6 mm after maxillomandibular advancement surgery in a group of patients with obstructive sleep apnea. Mehra et al.9, in 2001, reported 76% increase in the retrolingual and oropharyngeal dimensions related to the amount of mandibular advancement, compared to other studies10-12 which related an average increase of 42% to 51% in the same dimensions and to the current study that obtained an average increase of 20.75% in the retropalatal dimension (UP-PHW) and of 24.52% in the retrolingual dimension (TB-PHW).
The mean mandibular advancement in patients in the survey was 5 mm, resulting in a 2.40 mm average increase of the UP-PHW and of 2.95 mm in the TB-PHW. These results contrast with the findings of Yu et al.13, in 1994, which had an average increase in the PAS size of 3.5±3.2 mm in patients with a PAS preoperative measurement under 11 mm, and of 0.9±3.6 mm in patients with a PAS preoperative measure greater than 11 mm.
Changes in pharyngeal airway space after mandibular setback surgery are controversial since some studies show changes in the airways space dimension, but do not affect their capacity15-16. In most studies1,6 PAS was measured by radiograph in lateral view in which the position of the head (craniofacial angulation) was not always constant. Additionally, the lateral radiographs show a two-dimensional aspect of the patient.
Mandibular advancement surgery has a greater impact on lower airways, whereas patients showed more changes in airways space17. This probably occurs because the tension of the suprahyoid muscles and other muscles inserted in the jaw causes a greater shift in the lower pharyngeal airway space. Furthermore, the inter-maxillary dimension increases and the tongue proportion decreases leading to an increase of the tongue space for its function, resulting in a more anterior position while extending the retroglossal airway.
According to the data, age presented no influence on the relationship between the amount of mandibular advancement and PAS changes. Moreover, skeletal alterations produced by mandibular advancement surgery have repercussions on PAS dimensions, particularly on the retrolingual dimension. However, it was not found significant association between the amount of mandibular advancement and the changes produced in the PAS, both for the retropalatal and for retrolingual measures.
References
1. Faria AC, Xavier SP, Silva Jr SN, Voi Trawitzcki LV, de Mello-Filho FV. Cephalometric analysis of modification of pharynx due to maxillamandibular advancement surgery in patients with obstructive apnea. Int J Oral Maxillofac Surg. 2013; 42; 579-84. [ Links ]
2. Freire EF, Freire Filho FWV, Valdrighi HC, Degan VV, Vedovello SAS. Changes in pharyngeal airway space and soft tissue after maxillary advancement and bimaxillary surgery. Braz J Oral Sci. 2014; 13: 93-7.
3. Soh CL, Narayanan V. Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgery—A systematic review. Int J Oral Maxillofac Surg. 2013; 42: 974–80
4. Zinser MJ, Zachow S, Sailer HF. Bimaxillary ‘rotation advancement' procedures in patients with obstructive sleep apnea: a 3-dimensional airway analysis of morphological changes. Int J Oral Maxillofac Surg. 2013; 42: 569-78.
5. Candido MSC, Monazzi MS, Gabrielli MAC, Spin-Neto R, Gabrielli MFR, Pereira-Filho VA. Pharyngeal airway space cephalometric evaluation in transverse maxillary deficient patient after SARME. Braz J Oral Sci. 2014; 13: 288-91.
6. Kim S, Kim K, Park J, Kim S. Cephalometric predictors of therapeutic responde to multilevel surgery in patients with obstructive sleep apnea. J Oral Maxillofac Surg. 2012; 70: 1404-12.
7. Mickelson SA. Hyoid advancement to the mandible (hyo-mandibular advancement). Oper Tech Otolaryngol. 2012; 23: 56-9.
8. Arikasa T, Ito C, Sato K, Tonogi M, Yamane G, Nakajima T. Examination of changes in the pharyngeal airway space under anterior traction of the mandible: Influence of detachment of the periosteum during orthognathic surgery. J Oral Maxillofacial Surg Med Pathol. 2014; 26: 540-4.
9. Mehra P, Downie M, Pita MC, Wolford LM. Pharyngeal airway space changes after counterclockwise rotation of the maxillomandibular complex. Am J Orthod Dentofacial Orthop. 2001; 120: 154-9.
10. Riley RW, Powell NB, Guilleminault C. Maxillary, mandibular, and hyoid advancement for treatment of obstructive sleep apnea: A review of 40 patients. J Oral Maxillofac Surg. 1990; 48: 20-6.
11. Li KK, Guilleminault C, Riley RW, Powell NB. Obstructive sleep apnea and maxillomandibular advancement: an assessment of airway changes using radiographic and nasopharyngoscopic examinations. J Oral Maxillofac Surg. 2002; 60: 526-31.
12. Farole A, Mundenar MJ, Braitman LE. Posterior airway changes associated with mandibular advancement surgery: implications for patients with obstructive sleep apnea. Int J Adult Orthodont Orthognath Surg. 1990; 5: 255-8.
13. Yu LF, Pogrel AM, Ajayi M. Pharyngeal airway changes associated with mandibular advancement. J Oral Maxillofac Surg. 1994; 52: 40-4.
14. Mannarino M, Di Filippo F, Pirro M. Obstructive sleep apnea syndrome. Eur J Intern Med. 2012; 23: 586-93.
15. Park J, Kim N, Kim J, Kim M, Chang Y. Volumetric, planar, and linear analyses of pharyngeal airway change on computed tomography and cephalometry after mandibular setback surgery. Am J Orthod Dentofacial Orthop. 2010; 138: 292-9.
16. Fernandez-Ferrer L, Montiel-Company J, Pinho T, Almerich-Silla A, Bellot- Arcís C. Effects of mandibular setback surgery on upper airway dimensions and their influence on obstructive sleep apnoea - a systematic review. J Craniomaxillofacl Surg. 2015; 43: 248-53.
17. Becker O, Avelar R, Göelzer J, Dolzan A, Haas Júnior O, Oliveira R. Pharyngeal airway changes in class III patients treated with double jaw orthognathic surgery – maxillary advancement and mandibular setback. J Oral Maxillofac Surg. 2012; 70: 639-47.
 Correspondence:
Correspondence:
Rafaela Scariot
Rua Professor Pedro Viriato Parigot de Souza, 5300
Curitiba - PR - Brazil - CEP 81280-330
E-mail: rafaela_scariot@yahoo.com.br
Received for publication: February 10, 2015
Accepted: May 28, 2015













