Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.14 no.3 Piracicaba Jul./Set. 2015
ORIGINAL ARTICLE
Masticatory performance with different types of rehabilitation of the edentulous mandible
Flávio Domingues NevesI; Francielle Alves MendesII; Tânia de Freitas BorgesII; Daniela Baccelli Silveira MendonçaIII; Marisa Martins da Silva PradoIV; Karla ZancopéI
I Universidade Federal de Uberlândia - UFU, School of Dentistry, Department of Occlusion, Fixed Prosthodontics and Dental Materials, Uberlândia, MG, Brazil
II Faculdade de Patos de Minas - FPM, School of Dentistry, Department of Prosthodontics, Patos de Minas, MG, Brazil
III University of North Carolina at Chapel Hill, Laboratory of Bone Biology and Implant Therapy, Department of Prosthodontics, Chapel Hill, NC, USA
IV Universidade Federal de Uberlândia - UFU, Technical School of Dentistry, Uberlândia, MG, Brazil
ABSTRACT
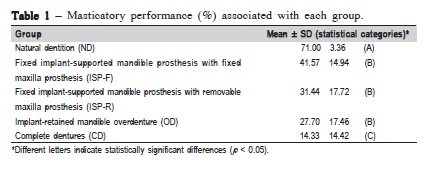
Aim: To compare the masticatory performance associated with different rehabilitation strategies for patients with edentulous mandibles. Methods: one portion of the test food "Optocal" was provided to groups: Natural Dentition (n = 15), Mandibular Fixed Implant-Supported Prosthesis with Maxillary Fixed Prosthesis (n = 8), Mandibular Fixed Implant-Supported Prosthesis with Maxillary Removable Prosthesis (n = 14), Mandibular Implant-Retained Overdenture with Maxillary Removable Prosthesis (n = 16), and Complete Dentures (n = 16). The portion was collected after 40 chewing strokes, and then passed through a stack of eight sieves with decreasing apertures. Masticatory performance was determined by weighing the portion of food on each sieve. Results: the masticatory performance was: 71.00% for Natural Dentition, 41.57% for Mandibular Fixed Implant-Supported Prosthesis with Maxillary Fixed Prosthesis, 31.44% for Mandibular Fixed Implant-Supported Prosthesis with Maxillary Removable Prosthesis, 27.70% for Mandibular Implant-retained Overdenture, and 14.33% for Complete Dentures. The data were statistically compared using Student's t-test (p < 0.05). Natural Dentition and Complete Denture groups were statistically different from all other groups, with the Natural Dentition and Complete Denture groups exhibiting the highest and lowest masticatory performance values, respectively. Conclusions: Osseointegrated implants improved the masticatory performance of all implant-supported groups compared to the Complete Dentures group.
Keywords: mastication; prostheses and implants; dental implants; dental prosthesis retention.
Introduction
Digestive enzymes and proper mastication must transform complex molecules into simple structures1. Deficient masticatory function often forces an individual to choose foods that are easier to chew rather than foods that fulfill daily nutritional needs. Complete denture wearers commonly avoid hard foods2, which typically leads to a poor-quality diet3. Even when these patients try to eat hard foods, they swallow larger portions, which decreases nutrient absorption and may not provide enough nutrients to maintain good general health4. Swallowing larger portions of food also increases the risk for gastrointestinal problems and diseases related to malnourishment3,5. However, gender-specific interventions and counseling aimed at slowing the rate of ingestion could be promising behavioral treatments for obese persons6.
For an edentulous patient, good masticatory performance is the most difficult function to reestablish. Prior to the development of dental implants, the only option was complete dentures. Oral rehabilitation using dental implants provides better retention and stability to prostheses. Previous studies have evaluated the effect of missing teeth on masticatory function7-9, but comparisons among these studies are difficult because the methods were not standardized. The sieves method, use of natural test food, the Optocal10 and optical scanning11 are the most usually employed test foods to evaluate masticatory efficiency.
The aim of this study was to compare masticatory performance between different rehabilitations for patients with edentulous mandibles. The hypothesis of the present study was that masticatory performance in patients with complete dentures would be improved by dental implants to retain and/or support the prosthesis.
Material and methods
The Federal University of Uberlândia Research Ethics Committee approved this research (141/07). A written, informed consent was obtained from each subject before the tests. Five groups of subjects were enrolled in this study: (ND) natural dentition or control group (n = 15, 20–28 years old), (ISP-F) mandibular fixed implant-supported prosthesis with maxillary fixed prosthesis (n = 8, 55-–80 years old), (ISP-R) mandibular fixed implant-supported prosthesis with maxillary removable prosthesis (n = 14, 55–80 years old), (OD) mandibular implant-retained overdenture and maxillary complete denture (n = 16, 30–76 years old), and (CD) mandibular and maxillary complete dentures (n = 16, 30– 76 years old).
All prostheses were made at the Dental School of Federal University of Uberlândia 3 to 48 months before the tests were conducted. Prior to implant treatment, rehabilitation strategies included partial or complete removable prostheses that were used for approximately 2 years. Twelve patients in both ISP groups received immediate loading of the implant prostheses.
The control group comprised 15 subjects with natural dentition. Subjects had all their second molars, no prior orthodontic treatment, and no signs or symptoms of traumatic occlusion, periodontal disease or temporomandibular dysfunction. Exclusion criteria for the CD and ISP groups were any signs or symptoms of temporomandibular dysfunction.
Methods used in this study have been previously published9. Masticatory performance of all subjects was determined by chewing cubes of Optocal test food for 40 sequential strokes. Preparation of the Optocal test food has been also already described9. After mixing all components, the homogenized paste was placed in an aluminum mold 12.5 ' 12.5 cm and 0.56 cm deep. Samples were placed in an electrical stove at 65 °C for 16 h to ensure complete polymerization. Cubes were obtained using a device developed by the School of Mechanical Engineering of the Federal University of Uberlândia. Shore A durometer (Mitutoyo, São Paulo, SP, Brazil) was used to confirm the hardness of the Optocal food, which ranged from 30 to 35 shore-A units. Each portion consisted of seventeen cubes.
During the experiment, subjects were comfortably seated in dental chair, and instructed to chew normally. The test food was provided in one portion of 17 cubes (~3 cm3). After 40 masticatory strokes the chewed particles were spit into a 300-mL plastic cup. The subject was then asked to rinse his/ her mouth carefully with water, which was spit into the same cup. The examiner confirmed clinically that no pieces of test food remained in the oral cavity. The triturated particles were disinfected with 2% chlorhexidine solution (Pharmus, Uberlândia, MG, Brazil), according to a previous study12.
The chewed particles were passed through a stack of eight sieves (Bertel, São Paulo, SP, Brazil) with apertures that ranged from 5.6 to 0.5 mm. Food particles were placed on the upper sieve and washed with 1000 mL of water for 30s. The sieves were then placed on a dental laboratory vibrator (Vibramold, São Paulo, SP, Brazil) set at 1/2 speed for 2 min. Chewed particles from each sieve were then collected and placed in individual rigid plastic recipients (2 cm diameter and 1 cm high). The particles were dried in an electrical stove at 60 °C for 3 h. After drying, the particles from each recipient were weighed on an analytic scale (Sauter KG, Ebingen, Germany) with 0.0001 g accuracy.
Based on the weight of Optocal retained on each sieve, the geometric mean diameter (GMD) of the chewed particles was calculated using Excel (Microsoft, Redmond, WA, USA). Superior masticatory performance was considered as breaking up the test food into smaller particles.
To quantify particle reduction during chewing, it was necessary to define the maximal GMD value. It was therefore simulated a situation in which all particles remained intact after chewing and were retained on the first sieve (5.6 mm). The maximal particle GMD was defined as 6,660 μm. For each patient, the mean particle-reduction value was the difference between GMD and 6,660 μm (maximum possible GMD). To compare masticatory performances of ISP-F, ISPR, OD, and CD groups to the control (ND), the particle reduction of the ND group was considered as 100%.
Since the data followed a normal distribution, a parametric test was used for the objective analysis. The differences between groups were analyzed using the Student's t-test (α≤ .05), performed with SPSS 15.0 (SPSS, Chicago, IL, USA).
Results
The masticatory performance test revealed a statistically significant difference between ND and all other groups. CD group also exhibited a statistically significant difference in relation to all other groups. No significant difference was shown between ISP-F group and ISP-R or OD. ND group demonstrated the highest value for masticatory performance and the CD group was the least effective (Table 1).
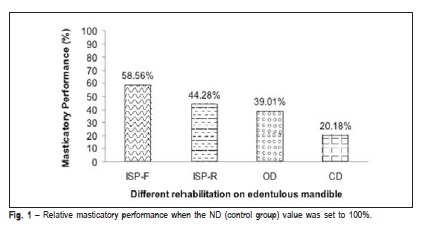
Figure 1 shows the corrected masticatory performance values after the ND value was set as 100%.
Discussion
The hypothesis of the present study was accepted, since the dental condition influenced the masticatory performance. The number of teeth rather than the extension of occlusal restoration13, the number of posterior teeth and the type of antagonist14 influence the chewing performance. Subjects with natural dentition showed the highest level of masticatory performance2. To set the masticatory performance score of the ND group to 100%, a group of patients with natural dentition was selected for the present study, with the highest level of masticatory performance. It is important to emphasize that even the ND group did not achieve 100% masticatory performance (Table 1), explaining the importance of higher numbers of chewing cycles before swallowing, decreasing the risk for gastrointestinal problems and diseases related to malnourishment3,5.
For populations with fewer resources, complete dentures are often the only choice for edentulous mandible rehabilitation. Therefore it is necessary to improve the conventional management of edentulous patients. Although a large number of edentulous patients are satisfied using complete dentures, a small number of patients are unable to adapt15. The best option for these patients is the dental implant. For other patients, the knowledge of their level of masticatory performance could help them choose between treatment strategies, and a period of adaptation, before choosing a treatment with dental implants, should be considered16. When possible, the implant-retained overdenture should be offered to edentulous patient to provide a better masticatory condition rather than a complete denture.
Patients with complete dentures often complain about the lack of retention and stability. These events are associated with aging, loss of muscle strength, reduced salivary flow and other factors, often forcing individuals to change their dietary pattern by choosing soft foods. This could lead to patient malnutrition8. In this study, patients with complete dentures exhibited only 20% of the masticatory performance of individuals with natural dentition. This finding raises questions about the efficiency of complete dentures in providing satisfactory oral rehabilitation. Oral rehabilitation with dental implants leads to better masticatory function in edentulous patients17. Previous study18 revealed a decrease in electromyographic amplitude for the masseter muscles during swallowing in elderly individuals with mandibular fixed implant-supported prostheses. This may indicate adaptation to new conditions of stability provided by fixation of the complete denture in the mandibular arch. Studies have demonstrated that the retention of complete dentures also influences the masticatory performance level of patients19, and treating complete denture wearers with implants to support the denture improves the chewing efficiency, increases maximum bite force and improves satisfaction20.
A multidisciplinary approach is necessary to evaluate the general health of patients with "poor oral condition" and to determine how chewing performance has affected their systemic health. The digestive system depends on the stomatognathic system, and the dentist must inform patients about the importance and potential benefits of improving the retention and stability of complete dentures by installing two dental implants, at least. This is a simple treatment that could improve a patient's masticatory and psychological condition19.
The present study indicated that subjects with natural dentition exhibited better masticatory performance than completely edentulous patients, but the use of osseointegrated implants improved the masticatory performance of all implantsupported groups when compared to the CD group.
Acknowledgements
The authors would like to thank Adérito Soares da Mota and Carlos José Soares for their assistance and critical reading of the manuscript. They also would like to thank Gustavo Mendonça for reviews and comments while preparing this manuscript, FAPEMIG, CAPES, CNPq and NEPRO Research Group for their support.
References
1. Kay RF. The functional adaptations of primate molar teeth. Am J Phys Anthropol. 1975; 43: 195-216. [ Links ]
2. Manly RS, Braley LC. Masticatory performance and efficiency. J Dent Res. 1950; 29: 448-62.
3. Hutton B, Feine J, Morais J. Is there an association between edentulism and nutritional state? J Can Dent Assoc. 2002; 68: 182-7.
4. N'Gom P I, Woda A. Influence of impaired mastication on nutrition. J Prosthet Dent. 2002; 87: 667-73.
5. Papas AS, Palmer CA, Rounds MC, Russell RM. The effects of denture status on nutrition. Spec Care Dentist. 1998; 18: 17-25.
6. Park S, Shin WS. Differences in eating behaviors and masticatory performances by gender and obesity status. Physiol Behav. 2015; 138: 69-74.
7. Borges T de F, Mendes FA, de Oliveira TR, Gomes VL, do Prado CJ, das Neves FD. Mandibular overdentures with immediate loading: satisfaction and quality of life. Int J Prosthodont. 2011; 24: 534-9.
8. Borges T de F, Mendes FA, de Oliveira TR, do Prado CJ, das Neves FD. Overdenture with immediate load: mastication and nutrition. Br J Nutr. 2011; 105: 990-4.
9. Mendonca DB, Prado MM, Mendes FA, do Prado CJ, das Neves FD. Comparison of masticatory function between subjects with three types of dentition. Int J Prosthodont. 2009; 22: 399-404.
10. Oliveira NM, Shaddox LM, Toda C, Paleari AG, Pero AC, Compagnoni MA. Methods for evaluation of masticatory efficiency in conventional complete denture wearers: a systematized review. Oral Health Dent Manag. 2014; 13: 757-62.
11. Eberhard L, Schneider S, Eiffler C, Kappel S, Giannakopoulos NN. Particle size distributions determined by optical scanning and by sieving in the assessment of masticatory performance of complete denture wearers. Clin Oral Investig. 2015; 19: 429-36.
12. Campos SS, Pereira VP, Zangerônimo MG, Marques LS, Pereira LJ. Influence of disinfectant solutions on test materials used for the determination of masticatory performance. Braz Oral Res. 2013; 27: 238-44.
13. Akeel R, Nilner M, Nilner K. Masticatory efficiency in individuals with natural dentition. Swed Dent J. 1992; 16: 191-8.
14. Julien KC, Buschang PH, Throckmorton GS, et al. Normal masticatory performance in young adults and children. Arch Oral Biol. 1996; 41: 69-75.
15. Carlsson GE, Omar R. The future of complete dentures in oral rehabilitation. A critical review. J Oral Rehabil. 2010; 37: 143-56.
16. Farias-Neto A, Carreiro Ada F. Changes in patient satisfaction and masticatory
17. efficiency during adaptation to new dentures. Compend Contin Educ Dent. 2015; 36: 174-7; quiz 178,190.
18. Vieira RA, Melo AC, Budel LA, Gama JC, de Mattias Sartori IA, Thomé G. Benefits of rehabilitation with implants in masticatory function: is patient perception of change in accordance with the real improvement? J Oral Implantol. 2014; 40: 263-9.
19. Berretin-Felix G, Nary Filho H, Padovani CR, Trindade Junior AS, Machado WM. Electromyographic evaluation of mastication and swallowing in elderly individuals with mandibular fixed implant-supported prostheses. J Appl Oral Sci. 2008; 16: 116-21
20. Thomason JM, Feine J, Exley C, Moynihan P, Müller F, Naert I, et al. Mandibular to implant-supported overdentures as the first choice standard of care for edentulous patients—the York Consensus Statement. Br Dent J. 2009; 207: 185-6.
21. Boven GC, Raghoebar GM, Vissink A, Meijer HJ. Improving masticatory performance, bite force, nutritional state and patient's satisfaction with implant overdentures: a systematic review of the literature. J Oral Rehabil. 2015; 42: 220-33.
 Correspondence:
Correspondence:
Flávio Domingues das Neves
Av. Pará, 1720, Bloco 4LA sala 4LA-42, Campus Umuarama
CEP: 38405-320
Uberlândia, Minas Gerais, Brasil
E-mail: neves@triang.com.br
Received for publication: May 27, 2015
Accepted: August 05, 2015













