Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Brazilian Journal of Oral Sciences
versão On-line ISSN 1677-3225
Braz. J. Oral Sci. vol.15 no.2 Piracicaba Abr./Jun. 2016
ORIGINAL ARTICLE
Incisor proclination and gingival recessions: is there a relationship?
Márlio Vinícius de OliveiraI;Matheus Melo PithonII; Márcia Luzia Lacerda XavierI; Rodrigo Villamarim SoaresI; Martinho Campolina Rebello HortaI; Dauro Douglas OliveiraI
I Pontifícia Universidade Católica de Minas Gerais – PUC Minas, School of Dentistry, Department of Orthodontics, Belo Horizonte, MG, Brazil
II Universidade do Estado da Bahia – UNEB, School of Dentistry, Area of Orthodontics, Jequié, BA, Brazil
ABSTRACT
Aim: To test the hypothesis that there is no relationship between the amount of vestibular inclination of mandibular incisors and the appearance of gingival recession in this region. Methods: This study included 20 patients selected in accordance with the following inclusion criteria: 1. adult patients without gingival recession in the mandibular incisors before treatment (T0), 2. no previous orthodontic treatment, 3. treated without tooth extraction in the mandibular arch, 4. bonded mandibular splinting from one canine to another after the active stage of orthodontic treatment (T1), 5. no visible wear of the incisal edge of the mandibular incisors, 6. Pre- and post-treatment teleradiography and plaster casts, and plaster casts 3 years post-treatment (T2). Depending on the amount of inclination of the mandibular incisors after treatment, the sample was divided into two groups: Group 1- 10 individuals (IMPA T1-T0 ≤ 5˚) and Group 2- 10 individuals (IMPA T1-T0 > 5˚). The measurement of length of the clinical crown (LCC) of the four mandibular incisors, distance between the incisal edge and vestibular marginal gingiva were made in plaster casts at T0, T1 and T2. Results: In spite of Group 1 presenting a reduction in LCC at T2, there was no statistically significant difference in LCC in the 3 time intervals evaluated in the two groups. Conclusion: The null hypothesis was accepted. The variation in the amount of vestibular inclination of the mandibular incisors during orthodontic treatment and 3 years after conclusion of treatment did not promote the appearance of gingival recessions in this group of patients.
Keywords: Gingival Recession. Orthodontics, Corrective. Cephalometry.
Introduction
A gingival recession is defined as the displacement of the marginal tissue apical to the cementoenamel junction1-3. Although its etiology is unclear, periodontal disease and mechanical trauma are considered the primary factors in the pathogenesis of gingival recessions4. Orthodontic treatment might promote the development of recessions5, with a possible mechanism being that orthodontic tooth movement can result in root positions close to or outside alveolar cortical plates; this can lead to bone dehiscences6,7. As a result, a marginal gingiva without proper alveolar bone support can migrate apically, leading to root exposure8. Furthermore, a fixed orthodontic appliance creates retention areas for dental plaque. In case of inadequate plaque removal, gingival inflammation could lead to periodontal breakdown9.
Gingival recessions are more frequently observed in mandibular than in maxillary teeth. With increasing age, they are more frequent on buccal than on lingual surfaces10. Canines, first premolars, and first molars in the maxilla, and central incisors and first premolars in the mandible are at the highest risk for labial gingival recessions11. The data suggest that gingival recession is universal and a common manifestation in most populations. Prevalence varies from 3% to 100% depending on the population and the methods of analysis12, and appears to be lower in younger groups, in which the incidence increases over time13. It has been estimated that over half of the adults in the United States have gingival recession, and on average, it affects about one fourth of the dentition14.
Several studies have demonstrated that labial movement of incisors in humans may be a risk factor for gingival recessions, but their conclusions were contradictory15,16. Some publications have shown association between incisor proclination and development of recessions and others have demonstrated the lack of such correlation17,18.
To date, studies that have focused on the development of gingival recessions in orthodontic patients have evaluated samples either immediately17,18 or several years after treatment19. The latter types were, however, limited to only 1 long-term observation. Consequently, the dynamics of the development of gingival recessions could not have been evaluated. Moreover, the studies did not establish safe limits with regard to the amount of vestibular inclination of mandibular incisors allowed, so that clinicians may make their decisions at the time of leveling the curve of Spee5,12.
The aim of this retrospective study was to test the following null hypothesis: there is no relationship between the amount of buccal inclination of mandibular incisors and the appearance of gingival recession in this region. In addition, an evaluation was made of whether an increase in the inclination of these teeth promoted increase in the length of their clinical crown (LCC).
Material and methods
This study was approved by the Research Ethics Committee (44066415000005137). The sample was selected from the files of patients treated at the Orthodontic clinic. The patients were selected in accordance with the following inclusion criteria: 1. adult patients without gingival recession in the mandibular incisors before treatment (T0), 2. no previous orthodontic treatment, 3. treated without tooth extraction in the mandibular arch, 4. bonded mandibular splinting from one canine to another after the active stage of orthodontic treatment (T1), 5. no visible wear of the incisal edge of the mandibular incisors, 6. Pre- and post-treatment teleradiography and plaster casts, and plaster casts 3 years post-treatment (T2).
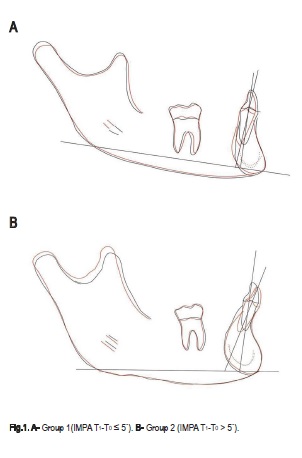
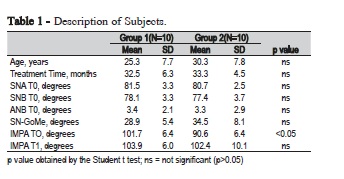
This retrospective study included 20 patients who met the inclusion criteria (13 men and 7 women). To evaluate the alteration that occurred in the inclination of the mandibular incisors after treatment, the measurement of the angle formed between the long axis of the mandibular incisor and the mandibular plane was used (IMPA). Depending on the amount of inclination of the mandibular incisors after treatment, the sample was divided into two groups: Group 1- 10 individuals (IMPA T1- T0 ≤ 5˚) and Group 2- 10 individuals (IMPA T1-T0 > 5˚) (Table 1). After obtaining the cephalometric tracing, the following points were marked: mandibular incisor edge and root apex, mentum (most inferior point of the mandibular symphysis), and gonium (the most inferior and posterior point of the mandibular angle). To identify the alterations in the inclination of the mandibular incisors after treatment, tracings were superimposed according to the mandibular superimposition technique, with stable natural structures used as reference16. The radiographic tracings were oriented, based on: 1- anterior contour of the pogonion region; 2-internal cortical contour at the level of the inferior edge of the mandibular symphysis; 3-trabecular structure of the mandibular symphysis; 4- mandibular canal contour; and 5- contour of the inferior edge of the mandible. References in stable anterior and posterior structures of the mandible were used in the pretreatment tracing (T0) and were transferred to the post-treatment tracing (T1) by means of superimposition.
All the cephalograms were traced and digitized by a single investigator. The teleradiographs were digitized in the resolution of 9.600 x 4.800 dpi in a Microtek ScanMaker i800 scanner (Microtek International, Inc., Carson, USA), coupled to a Pentium microcomputer. The images were transferred to the Dolphin Imaging Premium 10.5 program (Dolphin Imaging & Management Solutions, Chatsworth, USA), by means of which the cephalometric points of interest were marked and the superimpositions were made (Figure 1).
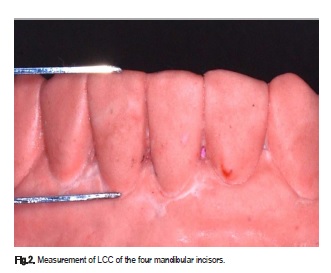
The measurement of LCC of the four mandibular incisors, distance between the incisal edge and vestibular marginal gingiva were made in plaster casts at T0, T1 and T2 (Figure 2). The measurements were taken by a single researcher, by using a digital pachymeter (Model 100.174B, Digimess, São Paulo, Brazil) with a precision of 0.01mm. Renkema et al.20 validated this method of evaluating the clinical crown by means of plaster casts. To determine the intra-examiner agreement, all the measurements were made twice, in an interval of one month. The Intraclass Correlation Coefficient (ICC) showed an excellent intra-examiner agreement.
The data were initially submitted to the Kolmogorov-Smirnov test of normality, which demonstrated their normal distribution. The groups were divided by using two criteria: Time (T0, T1 and T2) and variation in IMPA between T1 and T0 (≤5˚ and >5˚). The repeated measurements two-way ANOVA test, followed by the Bonferroni post hoc test for comparison between pairs was used to evaluate whether there were differences in LCC between the times (T0, T1 and T2). This evaluation was performed separately for each variation of the IMPA (≤5˚ and >5˚).
The two-way ANOVA test, followed by the Bonferroni post hoc test for comparison between pairs was used to evaluate whether there were differences in LCC between each IMPA (≤5˚ and >5˚). This evaluation was made separately for each of the times (T0, T1 and T2).
The Student t test was used to assess if the two evaluated groups were well paired. The level of significance was established at 5%. The analyses were performed with the use of GraphPad Prism 6.05 software (GraphPad Software, San Diego, California, USA).
Results
The two groups evaluated were well paired and their characteristics are presented in Table 1. The IMPA at T0 was greater in Group 1 (101.6˚) than in Group 2 (90,6˚), whereas, at the end of treatment (T1), their values were similar, due to the greater vestibular inclination that occurred in Group 2. None of the groups evaluated presented gingival recession after the active stage of treatment (T1) or during the post-splinting period (T2), in spite of the greater vestibular inclination of the mandibular incisors in Group 2 after treatment.
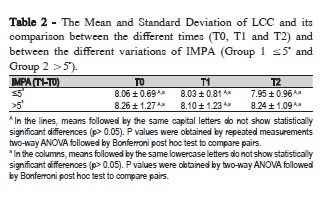
The Mean and Standard Deviation of LCC and its comparison between the different times (T0, T1 and T2) and between the different variations of IMPA (Group 1 ≤5˚ and Group 2 >5˚) are presented in Table 2. In spite of Group 1 presenting a reduction in LCC at T2, there was no statistically significant difference in LCC in the 3 time intervals evaluated in the two groups.
Discussion
Wedrychowska-Szulc and Syrynska21 verified that the majority of patients seek orthodontic treatment for esthetic reasons. Therefore, gingival recessions may compromise the esthetic results in addition to causing tooth hypersensitivity. Although its etiology has not been completely elucidated, gingival recession may be associated with orthodontic treatment20,22. Therefore, knowing that gingival recession may be a side effect of orthodontic therapy, identifying the factors that may contribute to the development of recessions is of great importance5. In this study, we investigated the relationship between the amount of change in inclination of the mandibular incisors during orthodontic treatment, and the changes that occurred in the LCC of these teeth, immediately after removal of the appliance, and three years later.
Our results showed that in spite of the difference in the amount of vestibular inclination of the mandibular incisors during treatment, the LCC remained unaltered in the two groups. Even in Group 2, in which there was greater vestibular inclination of the incisors, no appearance of gingival recessions had occurred in this region 3 years after orthodontic treatment. Thus, our results are in agreement with the findings of Yared et al.19, Ruf et al.23 and Djeu et al.24. Yared et al19evaluated the periodontal condition of mandibular incisors after orthodontic treatment and concluded that there was no correlation between gingival recession and the amount of vestibular inclination of these teeth. Ruf et al.23, in a sample of adolescents treated with the Herbst appliance, analyzed the alterations in the inclination of mandibular incisors and the development of gingival recessions 6 months after treatment. They verified that a mean vestibular inclination of 8.9 degrees of the mandibular incisors did not increase the risk of recession. Djeu et al.24 concluded that an inclination of 5 degrees in the mandibular incisors after orthodontic treatment in adolescents and adults, had no correlation with gingival recession. After a vestibular inclination of 5 degrees in the mandibular incisors, Allais and Melsen25 found no association between the amount of vestibular inclination of the mandibular incisors during orthodontic treatment in adults, and the prevalence and severity of gingival recession. Furthermore, they reported that around 5% of the patients had a reduction in gingival recession after treatment.
Other studies, however, found association between the alteration in inclination of the mandibular incisors and increase in the risk of gingival recession. In the study of Slutzkey and Levin26 the prevalence of recession was correlated with previous orthodontic treatment and the use of dental piercing. They examined 303 young adults (18-22 years) and found strong correlation between severity and extension of recession, and orthodontic treatment. Choi et al.22, in Class III patients decompensated before orthognathic surgery, evaluated whether the periodontal alterations in the mandibular incisors that underwent minimal vestibular inclination were similar to those that were highly tipped bucally. They observed that the mandibular incisors that had been very inclined towards the vestibular region during dental decompensation presented greater retraction of the vestibular cortical bone as well as a reduction in the strip of keratinized gingiva. Nevertheless, the amount of gingival recession appears to be clinically insignificant. The difference between our results and those found by the cited studies may be explained by the fact that none of our patients had gingival recession before treatment, which would show a more favorable periodontal biotype.
Previous studies have used intraoral photographs to evaluate periodontal alterations8,14. However, in some patients this method of evaluation was not ideal, because the retractors generally covered some part of the gingiva. Consequently, we opted to use the method of measuring the LCC directly in plaster casts, as described and validated by Renkema et al.20. Other factors, such as inflammation and gingival biotype, a narrow strip of keratinized gingiva are considered predisposing factors for gingival recession. A systematic review conducted by Joss- Vassalli et al.27 evaluated the effects of orthodontic treatment on the inclination of mandibular incisors and the occurrence of gingival recession. The authors concluded that further randomized clinical studies that included an examination of oral hygiene and the gingival condition before, during and after treatment are necessary in order to demonstrate the axial changes of the incisors, and the occurrence of gingival recession. The limitation of the present study was that some of the above-mentioned periodontal parameters were not evaluated. However, as regards oral hygiene care, all the patients were monitored and were able to perform adequate plaque control during orthodontic treatment, and in the post-splinting period.
Our results indicate that further prospective clinical studies that control the primary etiological factors of gingival recession, before, during and after treatment should be conducted. These studies must also classify patients according to their periodontal biotype.
The null hypothesis was accepted. The variation in the amount of vestibular inclination of the mandibular incisors during orthodontic treatment and 3 years after conclusion of treatment did not promote the appearance of gingival recessions in this group of patients. Even in Group 2, in which there was greater vestibular inclination of the incisors, there was no development of gingival recession in this region.
References
1. Garcia-De-la-Fuente AM, Aguirre-Zorzano LA, Estefania-Fresco R, Roig-Odena L, Aguirre-Urizar JM. Histologic and Clinical Study of Gingival Recession Treated with Subepithelial Connective Tissue Graft (SCTG): A Case Report. Int J Periodontics Restorative Dent. 2017 Jan/Feb;37(1):89-97. doi: 10.11607/prd.2638. [ Links ]
2. Gulati M, Saini A, Anand V, Govila V. Esthetic dentistry for multiple gingival recession cases: Coronally advanced flap with bracket application. J Indian Soc Periodontol. 2016 Mar-Apr;20(2):207-10. doi: 10.4103/0972-124X.175178.
3. Thankkappan P, Roy S, Mandlik VB. Comparative evaluation of management of gingival recession using subepithelial connective tissue graft and collagen membrane by periodontal microsurgical technique: A clinical study of 40 cases. J Indian Soc Periodontol. 2016 Mar-Apr;20(2):189-94. doi: 10.4103/0972-124X.176394.
4. Dandu SR, Murthy KR. Multiple Gingival Recession Defects Treated with Coronally Advanced Flap and Either the VISTA Technique Enhanced with GEM 21S or Periosteal Pedicle Graft: A 9-Month Clinical Study. Int J Periodontics Restorative Dent. 2016 Mar- Apr;36(2):231-7. doi: 10.11607/prd.2533.
5. Jati AS, Furquim LZ, Consolaro A. Gingival recession: its causes and types, and the importance of orthodontic treatment. Dental Press J Orthod. 2016 Jun;21(3):18-29.
6. Bansal A, Kulloli A, Kathariya R, Shetty S, Jain H, Raikar S. Comparative Evaluation of Coronally Advanced Flap with and without Bioactive Glass Putty in the Management of Gingival Recession Defects: A Randomized Controlled Clinical Trial. Journal of the International Academy of Periodontology. 2016 Jan 14;18(1):7-15.
7. Moraschini V, Barboza Edos S. Use of Platelet-Rich Fibrin Membrane in the Treatment of Gingival Recession: A Systematic Review and Meta-Analysis. J Periodontol. 2016 Mar;87(3):281-90.
8. Schwartz JP, Raveli TB, Schwartz-Filho HO, Raveli DB. Changes in alveolar bone support induced by the Herbst appliance: a tomographic evaluation. Dental Press J Orthod. 2016 Mar-Apr;21(2):95-101.
9. Kurtz B, Reise M, Klukowska M, Grender JM, Timm H, Sigusch BW. A randomized clinical trial comparing plaque removal efficacy of an oscillating-rotating power toothbrush to a manual toothbrush by multiple examiners. Int J Dent Hyg. 2016 Nov;14(4):278-83.
10. Thalmair T, Fickl S, Wachtel H. Coverage of Multiple Mandibular Gingival Recessions Using Tunnel Technique with Connective Tissue Graft: A Prospective Case Series. Int J Periodontics Restorative Dent. 2016 Nov/Dec;36(6):859-67.
11. Renkema AM, Navratilova Z, Mazurova K, Katsaros C, Fudalej PS. Gingival labial recessions and the post-treatment proclination of mandibular incisors. Eur J Orthod. 2015 Oct;37(5):508-13.
12. Rajapakse PS, McCracken GI, Gwynnett E, Steen ND, Guentsch A, Heasman PA. Does tooth brushing influence the development and progression of non-inflammatory gingival recession? A systematic review. J Clin Periodontol. 2007 Dec;34(12):1046-61.
13. Susin C, Haas AN, Oppermann RV, Haugejorden O, Albandar JM. Gingival recession: epidemiology and risk indicators in a representative urban Brazilian population. J Periodontol. 2004 Oct;75(10):1377-86.
14. Albandar JM, Kingman A. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988-1994. J Periodontol. 1999 Jan;70(1):30-43.
15. Kalha A. Gingival recession and labial movement of lower incisors. Evid Based Dent. 2013 Mar;14(1):21-2.
16. Aziz T, Flores-Mir C. A systematic review of the association between appliance-induced labial movement of mandibular incisors and gingival recession. Aust Orthod J. 2011 May;27(1):33-9.
17. Villard NM, Patcas R. Does the decision to extract influence the development of gingival recessions? A retrospective long-term evaluation. J Orofac Orthop. 2015 Nov;76(6):476-92.
18. Renkema AM, Fudalej PS, Renkema A, Kiekens R, Katsaros C. Development of labial gingival recessions in orthodontically treated patients. Am J Orthod Dentofacial Orthop. 2013 Feb;143(2):206-12.
19. Yared KF, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J Orthod Dentofacial Orthop. 2006 Jul;130(1):6 e1-8.
20. Renkema AM, Fudalej PS, Renkema A, Bronkhorst E, Katsaros C. Gingival recessions and the change of inclination of mandibular incisors during orthodontic treatment. Eur J Orthod. 2013 Apr;35(2):249-55.
21. Wedrychowska-Szulc B, Syrynska M. Patient and parent motivation for orthodontic treatment--a questionnaire study. Eur J Orthod. 2010 Aug;32(4):447-52.
22. Choi YJ, Chung CJ, Kim KH. Periodontal consequences of mandibular incisor proclination during presurgical orthodontic treatment in Class III malocclusion patients. Angle Orthod. 2015 May;85(3):427-33.
23. Ruf S, Hansen K, Pancherz H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession? Am J Orthod Dentofacial Orthop. 1998 Jul;114(1):100-6.
24. Djeu G, Hayes C, Zawaideh S. Correlation between mandibular central incisor proclination and gingival recession during fixed appliance therapy. Angle Orthod. 2002 Jun;72(3):238-45.
25. Allais D, Melsen B. Does labial movement of lower incisors influence the level of the gingival margin? A case-control study of adult orthodontic patients. Eur J Orthod. 2003 Aug;25(4):343-52.
26. Slutzkey S, Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop. 2008 Nov;134(5):652-6.
27. Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C. Orthodontic therapy and gingival recession: a systematic review. Orthod Craniofac Res. 2010 Aug;13(3):127-41.
 Corresponding author:
Corresponding author:
Dauro Douglas Oliveira
Pontifícia Universidade Católica de Minas Gerais
Av. Dom José Gaspar 500, Prédio 46 - Sala 101
CEP 30535-901 Belo Horizonte
MG - Brazil
E-mail: dauro.bhe@gmail.com
Received for publication: December 06, 2016
Accepted for publication: March 08, 2017













