Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Odontologia Clínico-Científica (Online)
versão On-line ISSN 1677-3888
Odontol. Clín.-Cient. (Online) vol.10 no.1 Recife Jan./Mar. 2011
CASE REPORT RELATO DE CASO
Diagnosis of acute promyelocytic leukemia after complication of dental procedure - Case report
Diagnóstico de leucemia pró-mielocítica aguda através de complicação de procedimento odontológico - Relato de caso
Roberto Tiago Alves PinheiroI; Belmiro Cavalcanti do Egito VasconcelosII; Suzana Célia de Aguiar S. CarneiroIII; Jefferson Luiz Figueiredo LealIV; Gabriela Granja PortoV
IEspecialist in Oral and Maxilofacial Surgery, Restauração Hospital – Recife/PE, Brazil
IICoordinator in Oral and Maxilofacial Surgery Master and PhD Program, University of Pernambuco – Recife/PE, Brazil
IIIMSc in Oral and Maxilofacial Surgery, University of Pernambuco – Recife/PE, Brazil
IVEspecialist in Oral and Maxilofacial Surgery, University of Pernambuco – Recife/PE, Brazil
VPhD-MSc in Oral and Maxilofacial Surgery, University of Pernambuco – Recife/PE, Brazil
ABSTRACT
Extraction may present risks and complications like any another dental procedure. It is a surgical procedure that represents a great challenge for the hemostatic mechanisms of the organism for several reasons. Considering the many possibilities of post-extraction bleeding, preventing hemorrhage is the best way to avoid complications. Patients with a history of hematoma or hemorrhage are a frequent problem in emergency rooms. The correct diagnosis and treatment of these patients depend on the knowledge of normal hemostasis mechanisms and the results of laboratory tests that evaluate these mechanisms. The present paper reports the case of a patient whose promyelocytic leukemia was diagnosed after hemorrhage resulting from the simple extraction a tooth.
Keywords: Occurrence, Denture Stomatitis, Actinic Cheilits
RESUMO
Exodontias podem apresentar riscos e complicações como qualquer outro procedimento odontológico. A exodontia é um procedimento cirúrgico, que representa uma grande mudança para os mecanismos de hemostasia do organismo por muitas razões. Considerando as muitas possibilidades de sangramento pós-exodontia, a hemorragia é um problema frequente nas salas de emergência. O diagnóstico correto e o tratamento desses pacientes dependem do conhecimento dos mecanismos normais de hemostasia e do conhecimento dos resultados de testes laboratoriais que avaliam esses mecanismos. O presente estudo relata o caso de um paciente cujo diagnóstico de leucemia promielocítica foi realizado após sangramento resultante de uma simples exodontia.
Descritores: Leucemia; cirurgia oral; morte.
INTRODUÇÃO
Extraction is a routine procedure in dental practice. However, it may present risks and complications like any another dental procedure1. Extraction is a surgical procedure that represents a great challenge for the hemostatic mechanisms of the organism for several reasons: facial tissues are highly vascularized; the surgical wound is open in soft and (bone) tissue; it is nearly impossible to perform an effective tamponment during surgery; the tongue causes constant displacement of the blood clot; and salivary enzymes may lyse the blood clot before the growth of granulation tissue2.
Considering the many possibilities of post-extraction bleeding, preventing hemorrhage is the best way to avoid complications. One of the most important procedures is a careful history taking to collect information on any previous3 history of bleeding episodes occurred with the patient and/or family, the use of medication that interferes with coagulation, coagulopathies, and specific systemic diseases, such as arterial hypertension, liver diseases and leukemia. Dentists should always be on guard to observe any unusual clinical signs that may lead to the early diagnosis of systemic disease processes.3,4.
Leukemia is a malignant disease that attacks leukocytes. It begins with a malignant transformation of a stem cell from bone marrow that reproduces and finally reaches the patient's periferic blood. Problems start when leukemia cells become more numerous than normal cells and erythrocyte precursor cells5. The disease may be acute or chronic, according to its clinical course. Acute leukemia affects immature cell lineages or blastic cells and, when not diagnosed and treated, results in rapid debility of the individual's general condition. The diagnosis of leukemia is established, through a myelogram, by the presence of more than 25% of leukemic cells on a bone marrow aspirative on puncture6.
The present paper reports the case of a patient whose promyelocytic leukemia was diagnosed after hemorrhage resulting from the simple tooth's extraction.
CASE REPORT
Patient APO, a 43 year-old male, was admitted to the emergency room of Hospital da Restauração – Recife/PE, Brazil, presenting alveolar hemorrhage after the extraction of an inferior canine tooth. The extraction had been performed about 6 hours prior to admission, and the patient developed intense bleeding through the surgical wound during this period. He had no history of bleeding or other symptoms before the extraction.
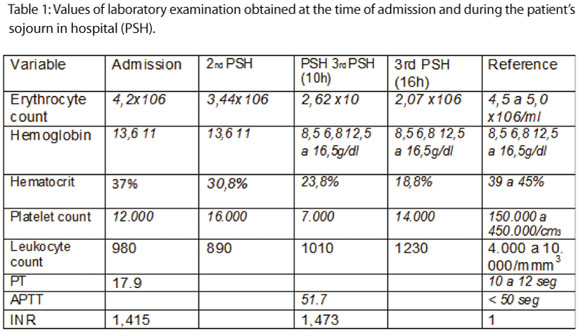
At the time of his hospitalization, the patient was conscious, oriented, eupneic, of pale coloration (+++/4+), afebrile, acyanotic, presenting diffused ecchymosis on the lower and upper limbs, heart rate of 89 bpm, arterial pressure of 150/110mmHg and a fair general condition. Local examination revealed isolated suture stitches and active bleeding of considerable intensity on the alveolus of tooth 33 (Figure 1). The patient remained under observation and laboratory tests such as clotting test count and coagulogram were requested. Their results indicated pancytopenia, especially because the number of platelets and leukocytes (Table 1), suggesting a clinical picture of leukemia. The clinical opinion of a hematologist was request, who suggested the diagnostic hypothesis of disseminated intravascular coagulation. Due to the gravity of the case, the patient was reffered to the Intensive Therapy Unit – ITU, where a myelogram led to a diagnosis of acute promyelocytic leukemia.

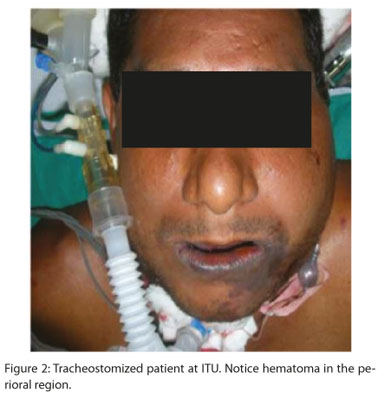
During the first 24 hours after admission to the ITU, the patient's general condition worsened and he developed severe dyspnea due to the formation of a hematoma in the mental, submandibular and sublingual regions (Figure 2) that was obstructing the upper airways. Orotracheal entubation was unsuccessfully tried, so an emergency tracheostomy was performed to protect the airways.
Hemotherapy was administered with transfusion of platelets and erythrocytes, without any improvement of the patient's general condition with progressed to severe pancytopenia on the 3rd day in the ITU. On the 6th day of hospitalization after the start of treatment for leukemia, the patient died.
DISCUSSION
Patients with a history of hematoma or hemorrhage are a frequent problem in emergency rooms. The correct diagnosis and treatment of these patients depend on the knowledge of normal hemostasis mechanisms and the results of laboratory tests that evaluate these mechanisms. Procedures performed in the oral cavity, especially those that may cause bleeding, represent major risk to patients suffering from hemostatic disorders. The type of leukemia diagnosed is related to the age prediliction of patients. The incidence of leukemia is higher in males than in females. The most common manifestations of leukemia are lymphadenopathy, laryngeal, gingival bleeding, oral ulceration, and gingival enlargement. Fever was the most common symptom in patients with all types of leukemia. Platelet counts from 25,000 mm-3 to 60,000 mm-3 are at sufficiently low levels to result in spontaneous bleeding. Most of the patients had WBC counts of greater than 10,000 mm-3. Only 12.6% of patients had normal WBC counts.7,8.
It is important to emphasize that most minor bleeding that occurs after oral surgery may be related to local factors dependent on the integrity of the closest anatomic elements. However, severe bleeding after oral surgery related to hemostatic systemic problems, such as liver diseases and hypertension9.
Hemostatic problems represent a complete interaction between blood vessels, platelets and the plasma coagulation system. These hematological impairments are classified according the the stage of coagulation that is affected, as follows: primary hemostatic disorder (responsible for the formation of the plate thrombus) and secondary hemostatic disorder, dependent on the plasmatic proteins and coagulation factors10.
Thus, if hemorrhage occurs immediately after a traumatism or a surgical procedure, it is a disturbance of the primary hemostasis. This type of hemorrhage is superficial and involves the oral mucosa, skin and nose, manifesting clinically through petechia, ecchymosis or purple lesions. Local treatment is usually satisfactory with immediate responses. Nevertheless, IF hemorrhage lasts for hours or days, it represents an alteration in the secondary hemostasis, involving deeper zones such as joints, muscles and retroperitoneal spaces. It manifests clinically through hematomas and the treatment requires systemic therapy11. In the case reported, hemorrhage began a few hours after extraction, local treatment had no success and hematomas were observed in the cervicofacial region, characterizing a picture of secondary coagulopathy. Secondary hemostatic disorders may be also divided into two groups: 1) congenital alterations, which include hemophilia A, hemophilia B and Von Willebrand disease, and 2) acquired alterations, including vitamin K metabolism disturbances, liver diseases and intravascular disseminated coagulation,9 the last of these having been developed by the patient in the present study.
According to Funayama et al. 12, the obstruction of the airways is a rare consequence of post-extraction bleeding. However, in the case reported the patient developed severe dyspnea, requiring protection of the airways which was achieved only by means of a tracheostomy.
The airways, breathing and circulation must be reestablished as rapidly as possible, as this is the first step towards the patient's clinical stabilization.
Uncontrollable intra-oral hemorrhage may lead to the rapid obstruction of the airways, as well as hematomas expanding into cervical region or the accumulation of blood in the airways13. In view of this, maintaining the permeability of the airways and the attempts at hemostasis became priorities from the moment that the patient developed dyspnea due to the hematomas in the submandibular, sublingual and submental regions.
According to Suchman & Mushlin14, it is inappropriate to request routine laboratory tests prior to surgery in patients without medical history of coagulation disorder. However, it is possible that some patients that have no bleeding history and even those submitted to previous extractions without complications may develop the disease asymptomatically, being diagnosed only13after some serious complication results in the patient's death, as in the case reported. The patient had been admitted with ecchymosis on the lower and upper limbs that had been overlooked unnoticed by himself and by the professional who performed the extraction.
Considering from the above, it is concluded that a simple extraction may result in serious complications, especially when an adequate history taking is not performed and the necessary laboratory tests are not requested.
Patients may present coagulation disorders whether asymptomatic or acquired, after a previous surgical procedure, leading to serious complications and consequently to the diagnosis of these hematological disorders.
REFERENCES
1. Goldberg MH, Nemarick, AN, Marco WP. Complications after mandibular third molar surgery: a statistical analysis of 500 consecutive procedures in private practice. J Am Dent Assoc 1985;111:277-35. [ Links ]
2. Peterson LJ, Ellis E, Hupp JR, Tucker MR. Contemporary Oral and Maxillofacial Surgery. St. Louis. Mosby: 2005. 800p. [ Links ]
3. Gleeson P. Spontaneous gingival haemorrhage: case report. Aust Dent J. 2002 Jun;47(2):174-5. [ Links ]
4. Gillette WB. Re: Oral manifestations of acute myelomonocytic leukemia: a case report and review of the classification of leukemias. Wu J, Fantasia Je, Kaplan R. (2002;73:664-668). J Periodontol. 2002 Oct;73(10):1228. [ Links ]
5. Neville BW, Damm DD, Allen CM, Bouquot JE. Hematologic disorders. In:__.Oral & maxillofacial pathology. Philadelphia: Sauders; 2004. p.416-42. [ Links ]
6. Epstein JB, Stevenson-Moore P. Periodontal disease and periodontal management in patients with cancer. Oral Oncol 2001 Jan; 37(8): 613-9. [ Links ]
7. Hou GL, Huang JS, Tsai CC. Analysis of oral manifestations of leukemia: a retrospective study. Oral Dis. 1997 Mar;3(1):31-8. [ Links ]
8. Quintero Parada E, Sabater Recolons MM, Chimenos Kustner E, López López J. Hemostasia y tratamiento odontológico. Av. Odontoestomatol 2004; 20-5: 247-261. [ Links ]
9. BermudoAñino L, Gutierres JL. Manejo del paciente con trastornos hemorrágicos. En: BermudoAñino L, Palma Gómez de la casa A, editores. [ Links ]
Tratamiento del paciente odontológico con hemopatías. Madrid: Glaxo-Smith- LilineIntigraf; 2001. p. 39-54.
10. Joseph R. Introducción a los trastornos hematológicos. En: Roce L, Kaye D, editores. Medicina interna en odontología. Barcelona: Salvat; 1992. p. 343-8. [ Links ]
11. Cutando A, Gil-Montoya JA. El paciente dental con alteraciones de la hemostasia. Revisión de la fisiopatología de la hemostasia para odontólogos. Med Oral 1999;4:485-93. [ Links ]
12. Funayama M, Kumagai T, Saito K, Watanabe T. Asphyxial death caused by postextraction hematoma. Am J Forensic Med Pathol 1994; 15(1):87–90. [ Links ]
13. Moghadam HG,. Caminiti MF. life-Threatening Hemorrhage after Extraction of Third Molars: Case Report and Management Protocol.J Can Dent Assoc 2002; 68(11):670-4. [ Links ]
14. Suchman AL, Mushlin AI. How well does activated partial thromboplastin time predict postoperative hemorrhage? JAMA 1986; 256(6):750–3. [ Links ]
 Corresponding author address:
Corresponding author address:
Belmiro Cavalcanti do Egito Vasconcelos
Av. General Newton Cavalcanti, 1650
Camaragibe/PE - Brasil
e-mail: belmiro@pesquisador.cnpq.br
Recebido para publicação: 29/12/10
Encaminhado para reformulação: 10/01/11
Aceito para publicação: 17/01/11













