Serviços Personalizados
Artigo
Links relacionados
Compartilhar
IJD. International Journal of Dentistry
versão On-line ISSN 1806-146X
IJD, Int. j. dent. vol.9 no.3 Recife Jul./Set. 2010
REVIEW ARTICLE REVISÃO DE LITERATURA
The use of chlorhexidine varnishes in children: what is out there?
O uso de verniz de clorexidina em crianças: o que há disponível?
Anna Galganny-AlmeidaI; Cristiane Tomaz RochaII; Beatriz Gonçalves NevesIII; Breno Rabelo RebouçasIV
IDDS, PhD in Pediatric Dentistry, Private Practice, Fortaleza, CE, Brazil
IIDDS, MSc, PhD Student, Department of Pediatric Clinics, Preventive and Community Dentistry, Dental School of Ribeirão Preto, University of São Paulo, Ribeirão Preto, SP, Brazil
IIIDDS, MSc, PhD student, Department of Operative Dentistry, Faculty of Pharmacy, Dentistry and Nursing, Federal University of Ceará, Fortaleza, CE, Brazil
IVDDS, PhD, Department of Periodontolgy and Oral Biology, Boston University, Boston, Massachussets, USA
ABSTRACT
The effect of innovative preventive measures in children highly infected with Mutans Streptococci is raising a significant impact in Pediatric Dentistry. Chlorhexidine varnishes are among the techniques in preventive dental research. The purpose of this paper is to introduce three chlorhexidine varnishes that are available in the world's market today and to illustrate the step-by-step procedure for its use in children, as well as its advantages and disadvantages. Chlorhexidine varnishes will soon be highly considered worldwide in combination with already established preventive methods against the development of dental caries in children.
Keywords: Chlorhexidine; Dental caries; Children
RESUMO
O efeito de medidas preventivas inovadoras em crianças altamente infectadas com Streptococcus Mutans está levantando um impacto significativo em Odontopediatria. Vernizes de clorexidina estão entre os materiais na pesquisa odontológica preventiva. O objetivo deste trabalho é introduzir três vernizes de clorexidina que estão disponíveis no mercado mundial atual e destacar o procedimento passo a passo para a sua utilização em crianças, bem como suas vantagens e desvantagens. Vernizes de clorexidina em breve serão altamente considerados a nível mundial, em combinação com os já estabelecidos métodos preventivos contra o desenvolvimento de cárie dental em crianças.
Palavras-chave: Clorexidina; Cárie dental; Crianças
INTRODUCTION
The increasing emphasis on the promotion of health has led to a growing interest in utilizing models based at early disease prevention. It is of unanimous knowledge that the etiology of dental caries is multifactorial, and that will not occur without the presence of the microorganism. The cariogenic bacteria Mutans Streptococcus (MS) plays a major role in the course of this disease1. Thus, the suppression and stabilization of MS to nonpathogenic levels for longer periods is of vital importance in the prevention of dental caries2. Nevertheless, it seems to be difficult to decrease MS in caries-active patients. For this purpose, several antimicrobial agents have been introduced in preventive regimens3. Chlorhexidine (CHX) has been proved to be the most potent chemotherapeutic agent against MS and dental caries4. A number of studies have used a variety of methods for delivering chlorhexidine in mouthrinses5, gels2, or dentifrices6 for caries prevention.
In 1985, Balanyk and Sandham7 developed a CHX-containing antibacterial varnish that brought a new concept into preventive dentistry. This vehicle was safe in humans, compatible with CHX and able to release the chemotherapeutic agent into the oral environment at low but bactericidal levels for approximately two weeks. This sustained release CHX varnish was proven to be successful at suppressing MS for prolonged periods and more effective than other CHX vehicles.8 In addition to the property of slow-release, the enhanced suppressive effect of varnish on the MS colonization is likely due to the prolonged contact time between CHX and teeth9,10.
According to Shaeken et al.11, the anticaries effect of the CHX varnishes is believed to consist of the reduced cariogenicity of dental biofilm after the suppression of MS, due to the high sensitivity of this microorganism to the CHX2.
Several studies have reported that the application of a CHX varnish was successful in reducing oral MS9,10,12-14 and caries increment.15,16 With a number of long-term controlled clinical trials being performed all around the world, CHX varnishes may soon be highly considered in combination with already established preventive methods against the development of dental caries.
Based on the existing literature, the purpose of this paper is to review current information regarding the utilization of three different CHX varnishes that are available in the world's market today and to illustrate the step-by-step procedure for its use in children.
LITERATURE REVIEW
Efficacy in MS reduction/ Antimicrobial activity
Numerous studies demonstrate the effect of CHX varnishes in the suppression of MS in saliva and dental biofilm9,10,12-14,17. Nevertheless, the extent of this suppression depends of the concentration and frequency of exposure to CHX12. Several authors reported that after use of CHX in the form of varnish, bacterial growth can be supported for three months or more9,18.
Schaeken et al.18 tested the effect of several CHX concentrations (0%, 10%, 20%, 40°%) within the varnish and concluded that the optimal concentration for this varnish was approximately 40°%. In 1989, Schaeken and de Haan18 treated twelve subbects with a 50°% CHX varnish once or twice within one week and a significant suppression of MS was found in the interdental biofilm until the fourth week. In addition, the saliva samples showed MS suppression for the entire experimental period approximately 6 weeks. On the other hand, Schaeken et al.9proved that a single application of a 40°% CHX varnish with a reduced contact time of 15 minutes was sufficient to achieve a long-term suppression of MS levels in interproximal dental biofilm until 16 weeks. Ie and Schaeken12 analyzed the effects of one or two applications of 40°% of CHX varnish on the numbers of MS in human dental fissure biofilm from molar and premolar teeth. According to their findings, a stronger suppression of MS can be obtained after repeated treatment with 40°% CHX varnish, particularly for premolars.
Placement of fixed orthodontic appliances is normally followed by an increase in oral colonization by MS concomitant with an elevated risk for the development of dental caries19. Eronat and Alpöz20 evaluated the efficiency of a 1% chlorhexidine-containing varnish on the levels of MS in saliva of patients with fixed orthodontic appliance. The results from their study suggested that 1% CHX varnish reduced salivary MS levels for 1-month period and that the application should be repeated every 3 months to get antibacterial effect. Sandham et al.21also indicated that CHX varnish was also effective in suppressing MS levels for long periods in child orthodontic patients, with a significant reduction of MS counts until three months of post-treatment.
From a brief microbiologic perspective, after intensive treatment, CHX varnish kills all bacteria on the treated surface of the teeth. After a few hours, the surface of teeth will be recolonized by a range of bacteria which adhere from the saliva and start to multiply. Species of bacteria that are less sensitive to CHX, such as oralis streptococci, have the best chance to multiply. In contrast, within the streptococci group, the MS are the most sensitive to CHX. Therefore, CHX varnish causes a shift in the oral microflora and, consequently, the selective suppression of MS. Other species takes the place of MS in the ecosystem, thus long-term reduction in the counts of MS in biofilm leads to a noticeable reduction in caries incidence11.
Caries prevention
Joharji and Adenubi22 evaluated the prevention of pit and fissure caries using a 1% CHX varnish during a period of nine months. Their results concluded that the application of the antimicrobial varnish on occlusal surfaces of permanent molars significantly reduced the development of fissure caries. Similar findings were confirmed by Bratthall et al.15and Arauujo et al.16showing that occlusal fissures of permanent molars treated with CHX varnish developed significantly less carious lesions in a two-year period.
Recently, Baca et al.23 demonstrated that schoolchildren in three-monthly applications of 1% CHX varnish with no decayed or filled primary teeth at baseline showed a significantly lower incidence of caries lesions in primary molars (at 24 months) compared with a control group.
On the other hand, a study performed using 40% CHX varnish in a population with low caries prevalence demonstrated no caries-reducing effect on occlusal surfaces in recently erupted permanent molars24. Furthermore, Twetman25 in a review of the effect of the antibacterial methods concluded that the use of CHX varnishes for the prevention of caries in high-risk subbects has inconclusive evidence. This author suggested that the antibacterial treatments should always be accompanied by other preventive measures in caries-active children.
The utilization of CHX varnish in Early Childhood Caries (ECC)
ECC is a particularly virulent form of dental caries characterized by an overwhelming infectious challenge, with MS being the most likely causative agent. This bacterial accumulation is most often associated with inappropriate bottle habit or nocturnal bottle and breast-feeding practices, which plays a critical role in the early acquisition and clinical expression of this infection26. Furthermore, deleterious feedings practices in conjunction with inadequate oral hygiene practices have also been described as responsible for MS proliferation. According to Berkowitz27, the elevated of levels MS in ECC children regularly exceeded 30°% of the cultivable biofilm.
Treatment of ECC is generally restricted to early extraction of teeth and comprehensive restorative procedures with recommendations regarding improvement of dietary and feeding habits26. However, restorative dentistry has little impact on oral levels of MS28 . In addition, apparently, the available fluoride therapies do not give sufficient protection to high active-caries individuals29, such as those diagnosed with ECC. Since there is considerable evidence that children who experience ECC continue to be at high risk for new lesions in later years, it seems reasonable that additional antimicrobial therapies are necessary to modify the course of the disease and to prevent the future development of carious lesions in children who experienced ECC30.
There is one study in the literature that demonstrated the efficacy of CHX varnish in the prevention of the ECC31. According to their results, the DMFS scores were significantly lower in a group of children that were treated with 3-mothly applications of CHX varnish when compared to a control group. However, there are no studies in the literature using CHX varnish in youngsters being treated for ECC and highly susceptible to new carious lesions.
The use of CHX varnish is suitable and safe for very young child. The amount used is smaller than that for use of gel or mouthrinses and also does not rely on patient compliance. It also should be stressed that CHX varnishes are of significant benefit, because reduce costs and causes less trauma to the young child by early prevention of dental caries22.
Types of CHX varnish
For antimicrobial therapy against MS, treatments for professional and for home use are available commercially. Three types of CHX varnishes are available in the market:
1. Cervitec® (Ivoclar/Vivadent AG, Schaan, Liechtenstein) (Figure 1) is a 1% CHX and 1% thymol formulation in a viscous polyvinyl butyral base, in addition to < 41% ethanol and < 50°% ethyl acetate contents. Each milliliter of varnish contains 10 mg of CHX. Cervitec® is marketed by Ivoclar/Vivadent and it is supplied in a box containing 7 bottles, which includes a supply of 50 applicators "Vivabrushes" and 2 handles. Each bottle contains 1.5 ml of the varnish.
2. EC40® (Biodent BV, Nijmegen, The Netherlands) (Figure 2) is a highly supersaturated solution of CHX diacetate in alcohol which is stabilized by sandarac, a naturally occurring resin. The concentration of CHX diacetate in EC40® is 35%, in addition to 27% sandarac and 37% ethanol. EC40® is supplied in a box with 10 cartridges. Each EC40® cartridge contains 1.5 ml of varnish.
BioC® (Biodent BV, Nijmegen, The Netherlands) (Figure 3) is a solution of CHX diacetate in alcohol. The solution is too stabilized by sandarac that also has an antimicrobial potential. The percentage composition of CHX diacetate in BioC® is 20%, in addition to 37% sandarac and 43% ethanol. BioC® is delivered in handy plastic syringes. The box containing 4 syringes of 1.2 ml.

Frequency of CHX varnish application
Caries risk assessment is a critical step in the frequency of CHX varnish application. According to Messer32, numerous factors must be identified for the appropriate classification of children into risk groups such as "high", "moderate", and "low" caries risk. In high risk children, the CHX varnish application should be more frequent than those with moderate or low caries risk. However, there is no protocol of frequency application in the reviewed literature. Fennis-Ie et al.24 analyzed a group of children who received treatment with EC40® in addition to the standard treatment, which also included a chlorhexidine application every six months. After a period of three years, it was found that EC40® had a 35% caries reduction in addition to that achieved by six-monthly chlorhexidine applications alone. Moreover, Twetman and Peterson 33 evaluated proximal caries incidence and progression in schoolchildren at high risk. Cervitec® was applied three times within a two-week period. The results of their study showed an appreciable reduction in caries incidence and progression. In a prospective clinical trial carried out by Galganny-Almeida et al. (2004) with Brazillian children diagnosed with ECC, three-monthly Cervitec® varnish applications demonstrated a 43% reduction in caries in the varnish group when compared to a group receiving three-monthly fluoride applications alone34.
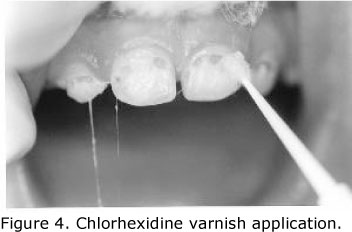
Step-by-step CHX varnish application procedure
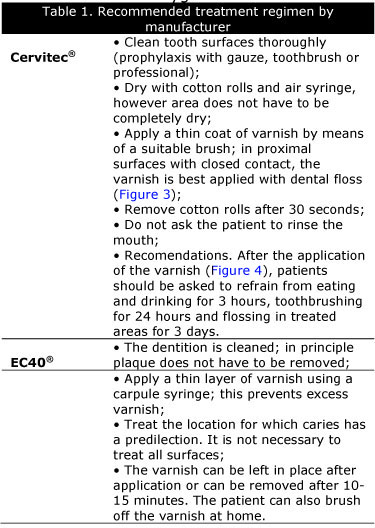
The most important aspects of treatment with CHX varnish are summarized in Table 1. The varnishes must be applied by a dentist or dental hygienist.
Indications
1. Reduce bacterial activity35.
2. Inhibit demineralization of tooth structure35.
3. Protection of enamel and dentin (Protection of exposed root surfaces and treatment in the hypersensitivity of the cervical areas of tooth structure)35.
Advantages
1. Ease of application22.
2. Patient compliance is assured3,8,29.
3. Children readily accept CHX varnishes21,22.
4. CHX varnishes are highly concentrated in their active content, therefore small amounts of CHX varnish when professionally applied to the teeth is sufficient to reduce high titers of MS for long periods18.
5. The cumulative dose of CHX in the varnish is lower than repeated rinsing with CHX mouthrinse. As a result, the common side effects of tooth staining and loss of taste can be avoided14.
6. The local irritation of the oral mucosa is common in the frequent use of CHX; however avoidance of the varnish application to the soft tissue minimizes irritation to the oral mucosa18.

Disadvantages
1. The cost for CHX varnish is increased compared with other types of CHX delivery systems.
2. Bitter taste9.
3. Some aesthetical discomfort, when anterior teeth are treated with varnish due to temporary peeling of the varnish9.
Toxicity and Ingestion
To date there are no reports of serious side effects with the use of CHX varnish.3 The reduction of these side effects could be most probably attributed to the low frequency of application of the CHX varnish when compared to other methods such as mouthrinses and gels14. Moreover, the possibility for ingestion of the CHX is significantly reduced when used in the form of the varnish14. In individual cases, contact with the mucous membrane may result in short-term, reversible irritation11. Though CHX in the form of mouthrinses and gels causes reversible discoloration of the tooth structure37, the varnish itself acts as a protective layer to prevent the teeth from staining7. Moreover, soreness of the oral mucosa by the use of CHX mouthrinses can be overcome by the use of local varnish application37. Desquamations with the use of the varnish are rare, because both frequency of use and concentration of CHX reaching the oral tissues are very low7.
CONCLUSION
A safe application of high concentrations of CHX in children is possible when its use is in the form of varnishes. Moreover, the CHX remains in the oral cavity over extended periods of time, thus the suppression and stabilization of MS to non-pathogenic levels are clearly observed overtime. The high incidence of caries in children following comprehensive restorative treatment for Early Childhood Caries is being highly reported, so antimicrobial therapy with the use of CHX varnish may be very beneficial for this group of children. In addition, the application of CHX varnish in child orthodontic patients can also be useful for the prevention of dental diseases. This study suggests that more research is urgently needed to determine the optimal preventive regimens, including antimicrobial therapies to prevent and modify the course of oral diseases in children.
REFERENCES
1. Loesche WJ, Walenga A, Loos P. Recovery of Streptococcus mutans and Streptococcus sanguis from a dental explorer after clinical examination of single human teeth. Arch Oral Biol 1973; 18:571-75. [ Links ]
2. Zickert I, Emilson CG, Vrasse B. Effect of caries preventive measures in children highly infected with the bacterium Streptococcus mutans. Arch Oral Biol 1982; 27:861-8. [ Links ]
3. de Soet JJ, Gruythuysen RJ, Bosch JA, van Amerongen WE. The effect of 6-monthly application of 40% chlorhexidine varnish on the microflora and dental caries incidence in a population of children in Surinam. Caries Res 2002; 36(6):449-55. [ Links ]
4. Fardal O, Turnbull RS. A review of the literature on use of chlorhexidine in dentistry. J Amer Dent Assoc 1986; 112:863-9. [ Links ]
5. Emilson CG, Westergren G. Effect of chlorhexidine on the relative proportions of Streptococcus mutans and Streptococcus sanguis in hamster plaque. Scan J Dent Res 1979; 87:288-95. [ Links ]
6. Emilson CG, Fornell J. Effect of tooth brushing with chlorhexidine gel on salivary microflora, oral hygiene, and caries. Scan J Dent Res 1976; 84:308-19. [ Links ]
7. Balanyk TE, Sandham HJ. Development of sustained-release antimicrobial dental varnishes effective against Streptococcus mutans in vitro. J Dent Res 1985; 64:1356-60. [ Links ]
8. Emilson CG. Potential efficacy of chlorhexidine against mutans streptococci and human dental caries. J Dent Res 1994; 73(3):682-91. [ Links ]
9. Schaeken MJ, Schouten MJ, Van Den Kieboom CW, Van Der Hoeven JS. Influence of contact time and concentration of chlorhexidine varnish on mutans streptococci in interproximal dental plaque. Caries Res 1991; 25(4):292-5. [ Links ]
10. Attin R, Tuna A, Attin T, Brunner E, Noack MJ Efficacy of differently concentrated chlorhexidine varnishes in decreasing mutans streptococci and lactobacilli counts. Arch Oral Biol 2003; 48(7):503-9. [ Links ]
11. Schaeken MJ, van der Hoeven JS, Hendriks JC. Effects of varnishes containing chlorhexidine on the human dental plaque flora. J Dent Res 1989; 68(12):1786-9. [ Links ]
12. Ie YL, Schaeken MJ. Effect of single and repeated application of chlorhexidine varnish on mutans streptococci in plaque from fissures of premolar and molar teeth. Caries Res 1993; 27(4):303-6. [ Links ]
13. Twetman S, Petersson LG. Comparison of the efficacy of three different chlorhexidine preparations in decreasing the levels of Mutans Streptococci in saliva and interdental plaque. Caries Res 1998; 32:113-8. [ Links ]
14. Achong RA, Briskie DM, Hildebrandt GH, Feigal RJ, Loesche WJ. Effect of chlorhexidine varnish mouthguards on the levels of selected oral microorganisms in pediatric patients. Pediatr Dent 1999; 21(3):169-75. [ Links ]
15. Bratthall D, Serinirach R, Rapisuwon S, Kuratana M, Luangjarmekorn V, Luksila K, Chaipanich P. A study into the prevention of fissure caries using an antimicrobial varnish. Int Dent J 1995; 45(4):245-54. [ Links ]
16. Araujjo AM, Naspitz GM, Chelotti A, Cai S. Effect of Cervitec on mutans streptococci in plaque and on caries formation on occlusal fissures of erupting permanent molars. Caries Res 2002; 36(5):373-6. [ Links ]
17. Sandham HJ, Brown J, Phillips HI, Chan KH. A preliminary report of long-term elimination of detectable mutans streptococci in man. J Dent Res 1988; 67(1):9-14. [ Links ]
18. Schaeken MJ, De Haan P. Effects of sustained-release chlorhexidine acetate on the human dental plaque flora. J Dent Res 1989; 68(2):119-23. [ Links ]
19. Lundstrom F, Krasse B. Streptococcus mutans and lactobacilli frequency in orthodontic patients; the effect of chlorhexidine treatments. Eur J Orthod 1987; 9(2):109-16. [ Links ]
20. Eronat C, Alpoz AR Effect of Cervitec varnish on the salivary Streptococcus mutans levels in the patients with fixed orthodontic appliances. J Marmara Univ Dent Fac 1997; 2(4):605-8. [ Links ]
21. Sandham HJ, Nadeau L, Phillips HI. The effect of chlorhexidine varnish treatment on salivary mutans streptococcal levels in child orthodontic patients. J Dent Res 1992; 71(1):32-5. [ Links ]
22. Joharji RM, Adenubi JO. Prevention of pit and fissure caries using an antimicrobial varnish: 9 month clinical evaluation. J Dent 2001; 29(4):247-54. [ Links ]
23. Baca P, Munoz MJ, Bravo M, Junco P, Baca AP. Effectiveness of chlorhexidine-thymol varnish in preventing caries lesions in primary molars. J Dent Child 2004; 71(1):61-5. [ Links ]
24. Fennis- Ie YL, Verdonschot EH, Burgersdijk RCW, Konig KG, Van't Hof MA. Effect of 6-monthly applications of chlorhexidine varnish on incidence of occlusal caries in permanent molars: a 3-year study. J Dent 1998; 26:233-8. [ Links ]
25. Twetman S. Antimicrobials in future caries control? A review with special reference to chlorhexidine treatment. Caries Res 2004; 38(3):223-9. [ Links ]
26. Berkowitz RJ. Causes, treatment, and prevention of Early Childhood Caries: A microbiologic perspective. J Canad Dent Assoc 2003; 69(5):304-7. [ Links ]
27. Berkowitz RJ, Turner J, Hughes C. Microbial characteristics of the human dental caries associated with prolonged bottle-feeding. Arch Oral Biol 1984; 29(11):949-51. [ Links ]
28. Gregory RL, El-Rahman AMA, Avery DR. Effect of restorative treatment on Mutans Streptococci and IgA antibodies. Pediatr Dent 1998; 20(4): 273-7. [ Links ]
29. Gerardu VA, Buijs MJ, ten Cate JM, van Loveren C. The effect of a single application of 40°% chlorhexidine varnish on the numbers of salivary Mutans Streptococci and acidogenicity of dental plaque. Caries Res 2004; 37(5):369-73. [ Links ]
30. Almeida AG, Roseman M, Sheff M, Huntington N, Hughes CV. Future caries susceptibility in children with Early Childhood Caries following treatment under general anaesthesia. Pediatr Dent 2000; 22(4):302-6. [ Links ]
31. Plotzitza B, Kneist S, Berger J, Hetzer G. Efficacy of chlorhexidine varnish applications in the prevention of early childhood caries. Eur J Paediatr Dent 2005; 6(3):149-54. [ Links ]
32. Messer LB. Assessing caries risk in children. Austral Dent Journal 2000; 45(1):10-6. [ Links ]
33. Twetman S, Petersson LG. Effect of different chlorhexidine varnish regimens on Mutans Streptococci levels in interdental plaque and saliva. Caries Res 1997; 31: 189-193. [ Links ]
34. Galganny-Almeida A, Rebouças BR, Neves BN, Rocha CT. The Efficacy of Antimicrobial Therapy in the Future Caries Susceptibility in Children Diagnosed with Early Childhood Caries (ECC). Pediatr Dent 2004;26 (2): 188. [ Links ]
35. Brambilla E, Cagetti MG, Fadini L, Pariset P, Strohmenger L, Twetman S. Chlorhexidine concentration in saliva after topical treatment with an antibacterial dental varnish. Am J Dent 2004; 17:1968. [ Links ]
36. Huizinga ED, Ruben J, Arends J. Effect of an antimicrobial-containing varnish on root demineralisation in situ. Caries Res 1990; 24(2):130-2. [ Links ]
37. Flotra L, Gjermo P, Rolla G, Waerhaug J. Side effects of chlorhexidine mouth washes. Scand J Dent Res 1971; 79: 119-125. [ Links ]
 Correspondent author:
Correspondent author:
Dr. Anna Galganny Almeida
Rua Osvaldo Cruz, 250 Apt. 400
Meireles 60125-250
Fortaleza-CE Brasil
e-mail: annagalmeida@terra.com.br
Telephone: +55 85 9121 2020
Fax: +55 85 3486 6444
Recebido em 05/05/2010
Aceito em 11/06/2010













