Serviços Personalizados
Artigo
Links relacionados
Compartilhar
IJD. International Journal of Dentistry
versão On-line ISSN 1806-146X
IJD, Int. j. dent. vol.9 no.3 Recife Jul./Set. 2010
CASE REPORT RELATO DE CASO
Nasopalatine duct cyst: a case report within 3 years follow-up
Cisto do ducto nasopalatino: relato de caso clínico com 3 anos de acompanhamento
Nicolau Conte NetoI; Alliny Souza BastosII; João Frank de Oliveira DantasIII; Waldner Ricardo Souza de CarvalhoIV; Cleverton Roberto de AndradeV; Eduardo Hochuli VieiraVI
IPhd student in Implantodonty, UNESP - Univ. Estadual Paulista, School of Dentistry, Department of Diagnosis and Surgery, Araraquara - SP/Brazil
IIPhd student in Periodontology, UNESP - Univ. Estadual Paulista, School of Dentistry, Department of Diagnosis and Surgery, Araraquara - SP/Brazil
IIIPhd student in Stomatology, UFPB -Univ. Federal da Paraíba, School of Dentistry, Department of Diagnosis and Surgery, Joao Pessoa - PB/Brazil
IVResident in Oral and Maxillofacial Surgery, UNESP - Univ. Estadual Paulista, School of Dentistry, Department of Diagnosis and Surgery, Araraquara - SP/Brazil
VAssistant Professor of Oral and Maxillofacial Surgery, UNESP - Univ. Estadual Paulista, School of Dentistry, Department of Diagnosis and Surgery, Araraquara - SP/Brazil
VIAssistant Professor of Oral Pathology UNESP - Univ. Estadual Paulista, School of Dentistry, Department of Physiology and Pathology, Araraquara - SP/Brazil
ABSTRACT
The nasopalatine duct cyst (NPDC) is considered to be the most common non-odontogenic cyst in the mouth. These cysts are usually asymptomatic; however they can result in swelling, pain and drainage. The radio logical analysis can reveal a round, oval or heart shaped well-demarcated image, which can be confounding with inflammatory lesions. The aim of this paper is report a clinical case of NPDC in a patient of 33 years old, occurring near a periapical inflammatory lesion. During clinical examination, it was not possible to detect swelling of the anterior palate and patient didn't complain painful symptoms. Surgical treatment, enucleation, was performed under local anesthesia and there was no post operative complications. Histological results showed the presence of a cuboidal and respiratory mucosa associated with vessels, nerves and inflammatory cells. The patient's 3 years follow-up was uneventful with subsequent bone regeneration and no sign of the lesion recurrence.
Keywords: Bone Regeneration; Respiratory Mucosa; Mouth
RESUMO
O cisto do ducto nasopalatino (CDNP) é considerado o cisto não odontogênico mais comum na cavidade bucal. Estes cistos são geralmente assintomáticos, entretanto podem resultar em edema, dor ou drenagem. A análise radiológica pode demonstrar uma imagem bem definida de forma redonda, oval ou em formato de coração, podendo ser confundindo ocasionalmente com lesões inflamatórias. O objetivo deste artigo é relatar um caso clínico de CDNP em uma paciente de 33 anos, ocorrendo nas proximidades de uma lesão inflamatória. Durante o exame clínico não havia edema na região anterior do palato, bem como sintomatologia dolorosa. O tratamento cirúrgico, enucleação, foi realizado sob anestesia local, sem a presença de complicações pós-operatórias. A análise histológica revelou a presença de epitélio cuboidal e respiratório associado com vasos, nervos e células inflamatórias. O pós-operatório de três anos procedeu-se sem complicações com regeneração óssea da loja cirúrgica sem sinais de recidiva.
Palavras-chave: Epitélio respiratório; Regeneração óssea; Cavidade bucal
INTRODUCTION
The nasopalatine duct cyst, first described by Meyer1 in 1914, is classified as the most common non-odontogenic cyst in the oral cavity2,3, originated from epithelial remnants of the nasopalatine duct4,5, in association with trigger events such as trauma, infection and spontaneous proliferation6. In most of the cases these cysts are asymptomatic6-8, thus detected during oral cavity routine examination8, especially after radiologic analysis that shows a well-demarcated radiolucency located in the midline of the maxilla that can be round, oval or heart shaped6. To avoid an incorrect management it important differentiates these cysts from a wide incisive foramen and inflammatory cystic lesions. The aim of this paper is report a case of nasopalatine duct cyst occurring near an inflammatory lesion that was detected after routine clinical and radiographic examination.
CASE REPORT
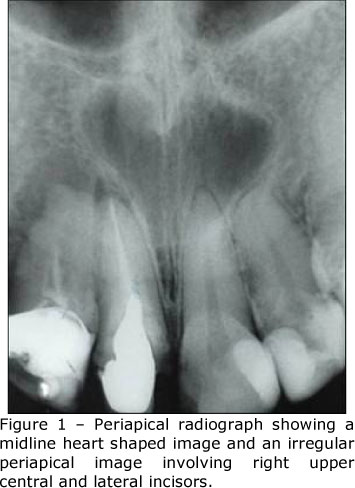
A 33-year-old caucasian woman was referred to evaluate a midline cystic lesion of the premaxilla detected during a routine clinical and radiographic exam. The patient's dental history revealed that she went through endodontic treatment of right maxillary central and lateral incisors, however without any information about the reason and the time that this treatment happened. Before the endodontic retreatment, the first periapical radiographic, revealed a well-demarcated unilocular heart shape radiolucent involving maxillary central incisors and left lateral incisor with 6 mm in diameter, surrounded by a sclerotic line with a intact lamina dura of maxillary incisors, an exception of the right lateral incisor, that also showed a apical irregular radiolucency apparently isolated from the other image (Figure 1). After five months, she was submitted to a retreatment of the same teeth for prosthetic reasons and to treat a periapical lesion.
After six months of this retreatment, it could be seen on a second periapical radiograph the same heart-shape image previously seen, however the second image had disappeared (figure 2). A maxillary occlusal radiograph showed an enlarged incisive foramen and although an improvement of the periapical lesion was noticed, the radiolucency in the midline of the upper jaw was still present and for this reason she was referred to the Department of Oral and Maxillofacial Surgery of Araraquara School of Dentistry, São Paulo State University (UNESP) Brazil.

During anamnesis the patient did not relate swelling, pain, loco-regional paresthesia or drainage in the oral cavity, associated to the lesion. Extra-oral examination did not reveal any facial asymmetries or palpable lymph node on ganglionar chain. Clinical examination of the oral cavity revealed good oral hygiene and normal aspect of the mucosa, without any swelling in soft tissue or fistulas. Her maxillary incisors had no mobility associated, were non-tender to percussion and without periodontal pockets. Left upper central and lateral incisors responded to vitality testing.
Based on clinical and radiographic evidences, a diagnosis hypothesis of nasopalatine duct cyst associated with a inflammatory periapical lesion was made. In this way, the patient underwent surgery for enucleation of the cyst under local anesthesia. At operation, a palatal mucoperiosteal flap was raised. During the surgery it was noted that the lesion was not associated with any teeth and it was firmly attached to the contents of the nasopalatine canal (Figure 3). Following appropriate bone removal the cyst was carefully enucleated and sent to histological analyses. The flap was repositioned with interrupted resorbable sutures.

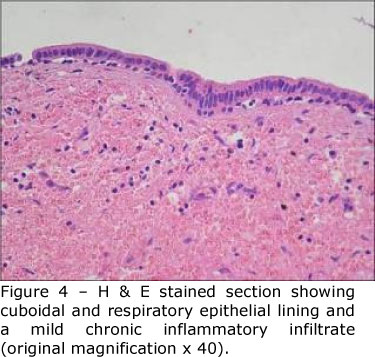
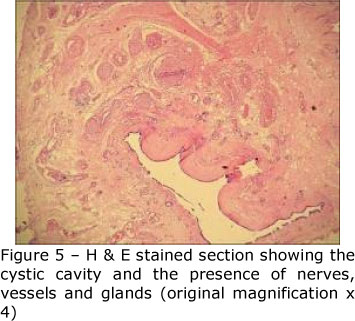
Histological evaluation revealed a cyst cavity lined by cuboidal and respiratory epithelium sustained by dense connective tissue (Figure 4) associated with nerves, arteries, salivary glands and chronic inflammatory cells (figure 5). These findings confirmed the provisional diagnosis of NPDC. The postoperative period was uneventful, followed by satisfactory healing. Three years after surgery, complete bone formation of the cyst cavity was evident on radiographic follow-up, without signals of recurrence (Figure 6).

DISCUSSION
The nasopalatine duct cyst is considered the most common non-odontogenic cyst in the oral cavity2,3. Although its etiology remains unknown, some factors are implicated as trigger agents especially trauma, infection and spontaneous proliferation5. In the present report no history of trauma was related, as well as periodontal pockets were not found in maxillary incisors, but there was a pathologic process in the adjacent teeth that might have disseminated to the nasopalatine duct, as has been reported5, however during the surgery no anatomical relation with the roots of the anterior teeth was found. Although it can not be affirmed for sure with regard to any specific etiological factor for the present occurrence of this cyst, spontaneous proliferation may be implicated in this case report.
NPCD has been reported in patients ranging from 7 to 72 years of age7,8, however, the peak incidence is between 5050 years of age5,8, being rare in young patients9. This is in agreement with the present report, as the patients age was 33. Most studies show a higher incidence of NPDC among males8,10 with male/female ratio of 3:19, differing from this case report. Otherwise, Francoli et al. (2009) have not found any gender prevalence. Although among the literature researched for this paper there was no tendency for a female prevalence, this woman's case report might be considered as an eventual case, as it is not a large case series. Concerning the incidence among races, it's difficult: to ascertain any preponderance, while some authors reported high incidence in blacks11,12 others also reported the same rates in the white population6,10.
The NPDC is frequently detected after a routine clinical and radiographic examination, due the lack of any marked clinical symptom8. In this way cysts are usually reported to be asymptomatic6-8, which is consistent with our findings. However, in other cases it can be also present swelling in the anterior palate7,8,13, drainage5 and pain13 and which is generally associated with secondary infections or pressure exerted on the nasopalatine nerves14.
Radiographic evaluation demonstrate a well-defined radiolucency often located in the midline of the maxilla6,8. Even though roots may diverge, the lamina dura of incisors remains intact15. All these findings are consistent with the present report. Concerning the shape of radiolucency Francoli et al. (2009) found most cases as rounded or oval images. The heart-shape radiolucency, that occurs due the superimposition of the nasal spine7,13 and which was found in this report, has a less frequent appearance6. Diameters ranging from 10 to 40 mm have been reported6,8,13.
The diagnosis of NPDC is made primarily from clinical and radiographical observations, but can be confirmed by histopathological analysis6, specially by the presence of nerves and blood vessel found in this report that are considered by Abrams et al. (1963) to be the most important differentiation criterion of NPDC from cysts of other origins. A relevant aspect to consider is the differential diagnosis between NPDC from normal, but wide, incisive canal and a periapical lesion. Even though a variation between 6 to 8 mm in the incisive canal has been found to be normal in this report it can be observed a radiolucency with 10mm of diameter, besides the normal foramen generally don't show a well-defined cortical border in its superior and inferior aspects and do not appears as a heart shape, as seen in this report.
Testing the pulp vitality of the involved teeth and lamina dura analysis are very important aids in having correct diagnosis, especially to differentiate odontogenic periapical lesions from NPCD, as in the nasopalatine duct cyst last one the lamina dura will be intact15 and the pulps usually vital6. However, in large size the cyst can expand and devitalize the pulp of these teeth6,13. In the present case there was initially two apparently distinct lesions, one related to the right maxillary lateral incisor and other one between the roots of upper central incisors. Although there is no information regarding the first endodontic treatment, it seems that the retreatment once done was related to both images, because according to the dental practitioner who referred the patient, the radiolucency still persisted even after the endodontic retreatment, characterizing a possible misdiagnosis.
Multiple different epithelial lining in distinct proportions have been reported in NPDC, where only one6 or more than one epithelial type10 can be found. The last one is in agreement with this case report that had both cuboidal and respiratory lining epithelium. However this specifically combination is not frequently found according Swanson et al. (1991). Squamous epithelium alone or associated with other epithelial type has been reported as the most common lining2,6. Although Bodin et al. (1986) did not find any relation to the vertical position of the cyst, it is generally accepted that the type of epithelium can be influenced by the proximity of nasal cavity6, as well by the presence of metaplastic transformation15,16.
Most authors stated the necessity of surgery as soon as possible, even in patients that have asymptomatic lesions6,15, in order to minimize the risk of complications, including root resorption, teeth displacement and bone perforation, especially if the cyst reaches a large size7. Other arguments towards surgical treatment are the excellent outcomes that have been reported after surgical removal6,17, preventing chronic trauma by dentures6 and the possibility of malignant transformation18. In the present case report, surgical removal of the cyst was the treatment chosen for most of the reasons previously reported.
In this case it was opted for enucleation of the lesion, as it is the technique usually recommended6,19, but marsupialization can be an option for larger cysts17, especially when a persistent fistula is a concern15. The recurrence is low after surgery6 and patients usually exhibit bone regeneration of the cyst cavity6,17 which is consistent with our findings.
CONCLUSION
The nasopalatine duct cyst is considered as the most common non-odontogenic cyst in the oral cavity, usually detected after a routine clinical and radiographic examination, due the lack of any marked clinical symptom. To avoid complications and unnecessary endodontic treatment, diagnosis at an early stage is essential. Besides, in the case presented, the surgical removal represented a predictable treatment option, providing bone formation on the cyst cavity and low recurrence of the lesion.
REFERENCES
1- Meyer AW. A unique paranasal sinus directly above the superior incisors. Journal of Anatomy 1914;48:118-129. [ Links ]
2- Elliott KA, Franzese CB, Pitman KT. Diagnosis and Surgical Management of Nasopalatine Duct Cysts. Laryngoscope 2004;114:1336-1340. [ Links ]
3- Grossmann SM, Machado VC, Xavier GM, Moura MD, Gomez RS, Aguiar MC, Mesquita RA. Demographic profile of odontogenic and selected nonodontogenic cysts in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e35-41. [ Links ]
4- Mermer RW, Rider CA, Cleveland DB. Nasopalatine canal cyst: a rare sequelae of surgical rapid palatal expansion (Letters to the Editor.) Oral Surg Oral Med Oral Pathol Oral Radiol Oral Endod 1995;80:620. [ Links ]
5- Swanson KS, Kaugars GE, Gunsolley JC. Nasopalatine duct cyst: an analysis of 334 cases. J oral Maxillofac Surg 1991;49:268-271. [ Links ]
6- Francolí EJ, Marqués NA, Aytés LB, Escoda CG. Nasopalatine duct cyst: report of 22 cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2008;13:E438-43. [ Links ]
7- Scolozzi P, Martinez A, Richter M, Lombardi T. A nasopalatine duct cyst in a 7-year-old child. Pediatr Dent. 2008;30:530-4. [ Links ]
8- Bachur AM, Santos TCRB, Silveira HM, Pires FR. Cisto do ducto nasopalatino: considerações microscópicas e de diagnostico diferencial. Robrac 2009; 18:58-62. [ Links ]
9- Hegde RJ, Shetty R. Nasopalatine duct cyst. J Indian Soc Pedod Prev Dent 2006;24:S31-2. [ Links ]
10- Vasconcelos RF, Ferreira de Aguiar MC, Castro WH, Cavalcanti de Araújo V, Mesquita RA. Retrospective analysis of 31 cases of nasopalatine duct cyst. Oral Dis 1999;5:325-328. [ Links ]
11-Chamda RA, Shear M. Dimensions of incisive fosse on dry skulls and radiographs. Int J Oral Surg 1980;9:452-457. [ Links ]
12-Nortje CJ, Wood RE. The radiologic features of the nasopalatine duct cyst: an analysis of 46 cases. Dentomaxillofac Radiol 1988;17:129-132. [ Links ]
13-Tanaka S, Iida S, Murakami S, Kishino M, Yamada C, Okura M. Extensive nasopalatine duct cyst causing nasolabial protrusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e46-50. [ Links ]
14-Anneroth G, Hall G, Sturge U. Nasopalatine duct cyst. Int J Oral and Maxillofac Surg 1986;15:572-580. [ Links ]
15-Bodin I, Isacsson G, Julin P. Cysts of the nasopalatine duct. Int J Oral Maxillofac Surg 1986;15:696-699. [ Links ]
16-Abrams AM, Howell F, Bullock WK. Nasopalatine cysts. Oral Surg Oral Med Oral Pathol 1963;16:306-332. [ Links ]
17-Oliveira MTF, Freire DR, Bicalho AA, Santos CRR, Soares JA. Nasopalatine duct cyst: clinical case report. Rev Odontol UNESP. 2009; 38(6): 371-4. [ Links ]
18-Takagi R, Ohashi Y, Suzuki M. Squamous cell carcinoma in the maxilla probably originating from a nasopalatine duct cyst: report of a case. J Oral Maxillofac Surg 1996;54:112-115. [ Links ]
19-Suter VG, Altermatt HJ, Voegelin TC, Bornstein MM. Die nasopalatinale Zyste. Epidemiologie, Diagnostik und Therapie.. Schweiz Monatsschr Zahnmed 2007;117:824-39. [ Links ]
 Correspondent author:
Correspondent author:
Nicolau Conte Neto
e-mail: conteneto@hotmail.com
Recebido em 21/01/2010
Aprovado em 30/04/2010













