Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista de Cirurgia e Traumatologia Buco-maxilo-facial
versão On-line ISSN 1808-5210
Rev. cir. traumatol. buco-maxilo-fac. vol.10 no.2 Camaragibe Abr./Jun. 2010
ARTIGO ORIGINAL
Prevalence and risk factors for the development of recurrent aphthous stomatitis
Prevalência e fatores de risco para o desenvolvimento de estomatite aftosa recorrente
Leonardo M LI; Diogo M DI; Arnaldo F C JrII; Fabíola B AIII; Verônica M S RII; Luiz Gutenberg T M C JrIII; Bruno S SilvaIV
IDental Surgeon, graduated at Faculty of Dentistry – University of Pernambuco – Brazil
IIAssociate Professor – Department of Dental Public Health – University of Pernambuco - Brazil
IIIPhD Student in Dental Public Health – Faculty of Dentistry – University of Pernambuco - Brazil
IVUndergraduate Dental Student - Faculty of Dentistry – University of Pernambuco - Brazil
ABSTRACT
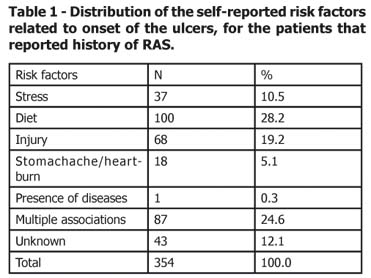
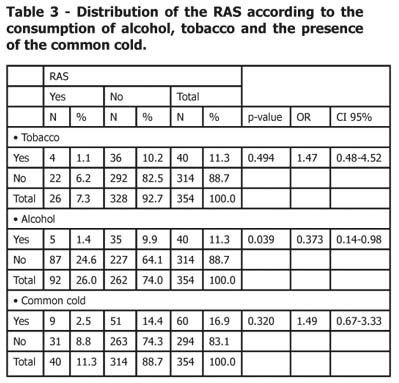
The aim of this study was to determine the self-reported, clinical prevalence and risk factors for the development of recurrent aphthous stomatitis. This is a cross-sectional study carried out with a calculated sample of 450 individuals selected from the individuals awaiting treatment at the Dental Clinic of the University of Pernambuco. All patients were interviewed and an oral examination was conducted. Information on risk factors was assessed during an interview by means of a specific questionnaire. Statistical analysis included descriptive and inferential analyses, and associations between categorical variables were tested using the X2 statistic. A high (78.67%) prevalence of recurrent aphthous stomatitis was found, mainly among women, although the clinical prevalence was 5.9%. Among the risk factors, diet was the most frequently mentioned (28.2%) by patients, followed by injuries and stress (19.2% and 10.5%, respectively). No significant association was found between recurrent aphthous stomatitis and the common cold. Tobacco use was not associated with the development of recurrent aphthous stomatitis (p>0.05). Statistical significance was observed between alcohol consumption and aphthous stomatitis (p<0.039). It was concluded that the prevalence of recurrent aphthous stomatitis is high and the most common risk factors are diet, trauma and stress.
KeyWords: Aphthous Stomatitis. Mouth Ulcers. Risk Factors. Prevalence.
RESUMO
O objetivo deste estudo foi o de determinar a prevalência clínica e autorelatada da estomatite aftosa recorrente e seus fatores de risco. Este é um estudo transversal, realizado com uma amostra calculada de 450 indivíduos, selecionados entre os indivíduos à espera de tratamento na Clínica Odontológica da Universidade de Pernambuco. Todos os pacientes foram entrevistados, e realizado um exame intrabucal. Informações sobre fatores de risco foram avaliadas durante uma entrevista por meio de um questionário específico. A análise estatística descritiva e inferencial incluiu análises de associações entre variáveis categóricas, utilizando o Qui-quadrado. Uma elevada (78,67%) prevalência autorelatada de estomatite aftosa recorrente foi obtida, principalmente entre as mulheres, embora a prevalência clínica tenha sido de 5,9%. Dentre os fatores de risco, a alimentação foi o mais citado (28,2%) pelos pacientes, seguido de traumas e stress (19,2% e 10,5%, respectivamente). Não foi encontrada associação significativa entre a estomatite aftosa recorrente e a presença do resfriado comum. Consumo de tabaco não foi associado com o desenvolvimento da estomatite aftosa recorrente (p> 0,05). A significância estatística foi observada entre o consumo de álcool e estomatite aftosa (p <0,039). Pode-se concluir que a prevalência de estomatite aftosa recorrente é elevada e os fatores de risco mais comuns são dieta, trauma e estresse.
Descritores: Estomatite Aftosa/epidemiologia. Úlceras Orais. Mucosa Bucal/patologia.
INTRODUCTION
The recurrent aphthous stomatitis (RAS) is one of the most frequent lesions in oral mucosa. The prevalence among differing populations has been documented as 5-66%1-5 with a high prevalence among women6 and it is especially common in North America1,3.
These lesions appear as a single lesion or in groups, in the non-keratinized areas as lips, tongue, buccal mucosa and soft palate7. They are usually painful, shallow round ulcers with an erythematous halo covered by a yellowish-gray fibromembranous layer2.
Many suggestions have been proposed but the etiology of recurrent aphthous stomatitis is still controversial8 and its occurrence is related to a range of factors9, so an effective therapy is still lacking. It is suggested that stress with its presumed effects on the immune system, constitutes one of the major causative agents of RAS10. The aetiopathogenesis of RAS appears to be a complex interaction of genetic, nutritional and hematologic factors11,12. Much has now been clarified about the mechanisms involved, and interesting new associations such as the involvement of a T cell mediated immunologic reaction have emerged13.
In view of this, this study was carried out in order to investigate the prevalence and risk factors related to the development of recurrent aphthous stomatitis.
MATERIALS AND METHODS
A cross-sectional survey was carried out with a sample of patients from the Dental Clinic of the Faculty of Dentistry of University of Pernambuco - Brazil. To calculate the sample size, a pilot study was performed with 100 patients in order to achieve the self-related prevalence of recurrent aphthous stomatitis. Using a 95% confidence interval, a standard error of 5% and an acquired prevalence of RAS of 75%, a sample of 450 patients was required. The patients were randomly chosen from the outpatient clinic patients.
All individuals underwent an interview in which they had to answer specific questions about RAS in their daily lives. The key questions from the questionnaire were gathered from the patient questionnaire and physical evaluation forms of the dental record (patient health and dental history) used at the dental clinic of University of Pernambuco. Furthermore, an oral examination was performed in all interviewed patients in order to observe the clinical prevalence of RAS lesions. Patients were asked about a family history of RAS and their dietary habits. Differences in prevalence and clinical manifestations were identified according to gender, age, stress, oral injuries, tobacco consumption, presence of common cold symptoms and use of medications at the time of the study.
The statistical analysis included descriptive and inferential analyses at a 5% significance level. Associations between categorical variables were tested using chi-square. Data were analyzed using SPSS version 11.0 software (SPSS Inc., Chicago, USA).
This research was approved by the Committee of Ethics in Research of the University of Pernambuco and all the subjects signed an informed consent form immediately before the interview.
RESULTS
The sample comprised 450 individuals, of whom 68.7% were females and 31.3% males. Ages ranged from 18 to 76 years, with the majority of the subjects (59.3%) in the 21 to 40 year-old group. A significant difference was found between age and the episodes of RAS (p=0.037) but not for gender (p=0.263).
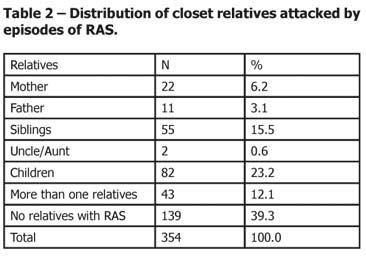
A high self-reported prevalence (78.6%) of RAS was observed, especially among the women (53.3%), however, 5.9% of the patients had the lesion at the time of the interview (clinical prevalence). Among all patients, 5.1% had a close relative who also presented RAS and a statistical significance was found between the presence of the RAS and family history of bouts (p=0.018).
Regarding to the frequency of the episodes of RAS, the majority (63%) rarely had them, about 15% said they had one every 15 days, another 15% answered every month and only 7% of the individuals said that the episodes were weekly. Most of the subjects (96.6%) reported that the ulcer heals after 7 to 14 days, 2.5% after 15 to 30 days and only 0.8% said it took from 4 to 6 weeks to heal. In addition, 85% of the respondents had pain during the episode.
The most frequent sites of the RAS, according to the patients were in multiple sites (46.6%), jugal mucosa (33.9%), labial mucosa (9.3%), tongue (8,5%) and soft palate (1.7%).
Around 33% of the individuals mentioned that food was responsible for making the aphthous ulcers worse. Among the aliments, citric fruits (71.9%) and spicy foods (7.8%) were the most commonly mentioned and a statistical significance was found between the intake of acid foods and the emergence of the lesion (P<0.001).
Table 1 shows the distribution of risk factors related to the onset of the ulcers, for the patients that reported history of RAS.
It was observed that 61% (215) of the patients with a history of RAS reported a familiar history of RAS. From Table 2 it can be seen that children (23.2%), followed by siblings (15.5%), were the closes relatives attacked by episodes of aphthae.
The distribution of the RAS according to the consumption of alcohol, tobacco and the presence of the common cold is shown in Table 3.
DISCUSSION
Evidence from previous studies shows that the recurrent aphthous stomatitis is a common lesion in the oral cavity14, with a high prevalence in females6, and may arise in response to several factors such as immunological, genetic and dietary factors, injuries, stress, allergic disorders and hormonal disturbances15-18.
In relation to the female predisposition to RAS, some authors have suggested that this association is related to hormonal rates18, which accounts for the coincidence of the appearance of the ulcers with puberty in young women19 and also leads to a decrease in its incidence during pregnancy, thus relating the episodes of RAS to progesterone levels16. Nevertheless, the results of this study, despite confirming the high prevalence of aphthae in females, did not confirm the hypothesis of the existence of a relation between this pathological condition and gender, thereby corroborating the findings of Ship3 and the ones reported by Chattopadhyay, Chatterjee8, who also demonstrated that there was no relation between RAS and gender. Moreover, these authors observed that the prevalence was higher in males, which was different from this study. Rivera-Hidalgo et al.2 and Shulman et al20 also found a higher prevalence among males, although without statistical significance.
Nowadays, the most widely accepted theory is the one that relates the episodes to immunological changes, so the development of ulcers is though to be related to a defective response of the immune system, which reacts nonspecifically to unknown antigens, but this response also could be related to the presence of microorganisms21,22. Various microorganisms have been tested, but none have been unequivocally incriminated in RAS. In this study, the existence of the common cold was used to test this theory, but no significant relationship was found for the development of aphthous ulcers.
Regarding to risk factors, diet was the one most frequently reported by the individuals and, among the aliments, citric fruits and spicy foods were mentioned as responsible for the episodes, highlighting the fact that acid foods were statistically significant for the development of the lesions, corroborating the report by21, thereby reinforcing the concern raised by other authors, who have found that the presence of allergies or sensibility to foods or tissue irritation from certain substances in these foods are closely related to the occurrence of RAS23. Patients allergic to a variety of foods, especially those containing pigment and preservatives, diminish the frequency of the episodes from 25 to 75% in the event of complete elimination of these substances from the diet23.
Injury was the second factor mentioned as being responsible for the development of aphthae. From a review of the literature7,18, injuries caused by anesthetic injection, sharp foods, brushing and/or dental treatment may trigger the aphthae. However, according to Barrons24, edentulous patients are not susceptible to RAS due to prosthetic injuries, probably because of the greater keratinization of the alveolar ridge that restricts the wound to the underlaying tissue.
A number of studies have shown that there is a familiar trend in the development of recurrent aphthous stomatitis24 and the correlation is also greater in identical twins17, demonstrating the existence of a genetic influence in the episodes. Moreover, according to these authors, around 50% of first degree relatives develop RAS, corroborating the findings of this study, where it was observed that children, as well as siblings and mothers, also had aphthae.
An inverse relationship between tobacco use and the appearance of RAS has been observed in the literature17 and smoking was found to be a protective factor21, although this association was not found in this study. Chattopadhyay, Chatterjee8 observed that individuals who had never smoked had a greater risk of RAS then the ones who smoked more than10 cigarettes per day. The findings of Ussher et al.26 demonstrated that there was a significant increase in reports of mouth ulcers relative to baseline following both one week and two weeks of smoking abstinence. According to the evidence17, the contact of harmful substances present in cigarettes with the oral mucosa leads to the production of parakeratin, which makes the mucosa thicker and, consequently more resistant. On the other hand, among the subjects with RAS at the time of the interview, a significant relationship was observed between alcohol consumption and patients with RAS at the time of the study (p=0.039; OR= 0.373), demonstrating that it was a protective factor, probably because of the same abovementioned factors for the individuals using tobacco. It is important to mention that the decision to use the patients with the lesion at the time of the interview was based on the statement that the lesion could be confounded with other lesions similar to RAS, so the clinical diagnosis by a trained examiner could diminish this bias, which could lead to a lower number of false negatives or positives. In addition, the lack of significance between the RAS and smoking should be well explored because this sample had a small number of smokers which might have masked some association.
With regard to the prevalence of RAS, it is important to highlight the fact that the self-reported prevalence of RAS found in this study was higher than the clinical prevalence which was near to the prevalence reported in other studies. This difference is probably due to cross-sectional design which might underestimate the real prevalence of the lesion because recurrent diseases may not be present at the time of the study27, thereby confirming the possible that the actual prevalence of RAS is greater than reported rates because of its recurrent nature3.
As showed, this disease has a multifaceted pattern. In view of this, considering its high prevalence and the fact that treatment is limited to a reduction of pain and discomfort, it is worth pointing out the need for further studies in this area in order to elucidate this cause-effect relationship to ensuring a specific treatment for those subjects, because the cross-sectional design lacks sufficient power for this. Furthermore, the findings from this study point to the importance of a thorough history taking with the aim of identifying the patient's main risk factors and informing him or her about how to control RAS through preventive measures.
Based on these results it was concluded that the prevalence of recurrent aphthous stomatitis is high and the most self-reported risk factors are diet, injuries and stress.
REFERENCES
1 Scully C, Shotts R. Mouth ulcers and other causes of orofacial soreness and pain. Student BMJ. 2000; 8: 411-4. [ Links ]
2 Rivera-Hidalgo F, Shulman JD, Beach MM. The association of tobacco and other factors with recurrent aphthous stomatitis in an US adult population. Oral Diseases. 2004; 10 (6): 335-45. [ Links ]
3 Ship JA. Recurrent aphthous stomatitis. An update. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 81(2): 141-7. [ Links ]
4 Femiano F, Lanza A, Buonaiuto C, Gombos F, Nunziata M, Cuccurullo L, et al. Guidelines for Diagnosis and Management of Aphthous Stomatitis. Pediatr Infect Dis J. 2007; 26(8): 728–32. [ Links ]
5 Scully C, Porter SR. Recurrent aphthous stomatitis: current concepts of etiology, pathogenesis and management. J Oral Pathol Med.1989;18(1):21-7. [ Links ]
6 Motta CS, Gouveia APC, Cherubini K. Epidemiological profile of RAU patients attended at stomatology Service of São Lucas Hospital - PUCRS. Rev Odonto Cienc. 2003; 18(39): 63-7. [ Links ]
7 Bruce AJ, Rogers RS. Acute oral ulcers. Dermatol Clin. 2003; 21(1): 1-15. [ Links ]
8 Chattopadhyay A, Chatterjee S. Risk indicators for recurrent aphthous ulcers among in the US. Community Dent Epidemiol. 2007; 35(2): 152-9. [ Links ]
9 Scully C, Porter S. Oral mucosal disease: Recurrent aphthous stomatitis. Br J Oral Maxillofac Surg. 2008; 46(3):198–206. [ Links ]
10 Albanidou-Farmaki E, Poulopoulos AK, Epivatianos A, Farmakis K, Karamouzis M, Antoniades D. Increased anxiety level and high salivary and serum cortisol concentrations in patients with recurrent aphthous stomatitis. Tohoku J Exp Med. 2008;214(4):291-6. [ Links ]
11 Rogers RS III. Recurrent aphthous stomatitis: clinical characteristics and associated systemic disorders. Semin Cutan Med Surg. 1997;16: 278-83. [ Links ]
12 Saral Y, Coskun BK, Ozturk P, Karatas F, Ayar A. Assessment of salivary and serum antioxidant vitamins and lipid peroxidation in patients with recurrent aphthous ulceration. Tohoku J Exp Med 2005; 305-12. [ Links ]
13Natah SS, Hayrinen-Immonen R, Hietanen J, Patinen P, Malmstrom M, Savilahti E, Konttinen YT. Increased density of lymphocytes bearing gamma/delta T-cell receptors in recurrent aphthous ulceration (RAU). Int J Oral Maxillofac Surg. 2000; 29: 375-80. [ Links ]
14Leao JC, Hodgson T, Scully C, Porter S. Review article: orofacial granulomatosis. Aliment Pharmacol Ther. 2004; 20(10): 1019-27. [ Links ]
15 Rees TD, Binnie WH. Recurrent aphthous stomatitis. Dermatol Clin. 1996; 14(2): 243-56. [ Links ]
16 Scully C, Gorsky M, Lozada-Nur F. The diagnosis and management of recurrent aphthous stomatitis: a consensus approach. J Am Dent Assoc. 2003; 134(2):200-7. [ Links ]
17 Woo SB, Sonis ST. Recurrent aphthous ulcers: a review of diagnosis and treatment. J Am Dent Assoc. 1996; 127(8): 1202-13. [ Links ]
18 Ship JA, Chavez EM, Doerr PA, Henson BS, Sarmadi M. Recurrent aphthous stomatitis. Quintessence Int. 2000 ; 31(2): 95-112. [ Links ]
19 Gonzaga, H FS. Avaliação sistêmica de paciente portador de ulceração aftosa recorrente. Rev Odontol UNESP. 1995; 24(2): 253-62. [ Links ]
20Shulman JD, Beach MM, Rivera-Hidalgo F. The prevalence of oral mucosal lesions in U.S. adults: data from the Third National Health and Nutrition Examination Survey, 1988-1994. J Am Dent Assoc. 2004;135(9):1279-86. [ Links ]
21Petersen MJ, Baughman RA. Recurrent aphthous stomatitis: primary care management. Nurse Pract. 1996; 21(5): 36-47. [ Links ]
22Sugaya NN, Marcucci G. Ulcer: still a mistery. Rev Abo Nac. 1999; 7(2): 73-5. [ Links ]
23Rodu B, Mattingly G. Oral mucosal ulcers: diagnosis and management. J Am Dent Assoc. 1992; 123(10): 83-6. [ Links ]
24Barrons RW. Treatment strategies for recurrent oral aphthous ulcers. Am J Health Syst Pharm. 2001; 58(1): 41-53. [ Links ]
25 Tüzün B, Wolf R, Tuzun Y, Serdaroglu S. Recurrent aphthous stomatitis and smoking. Int J Dermatol. 2000; 39(5): 358-60. [ Links ]
26Ussher M, West R, Steptoe A, McEwen A. Increase in common cold symptoms and mouth ulcers following smoking cessation. Tob Control. 2003; 12(1): 86-8. [ Links ]
27Kleinman DV, Swango PA, Niessen LC. Epidemiologic studies of oral mucosa conditions: methodologic issues. Community Dent Oral Epidemiol. 1991; 19(3):129-40. [ Links ]
 Corresponding Author:
Corresponding Author:
Prof. Dr. Arnaldo de França Caldas Jr
Estrada de Aldeia, Km 13 – Prive Portal de Aldeia. Aldeia
Camaragibe / PE – Brazil - Zip Code: 54783-010
E-mail: caldasjr@alldeia.com.br
Recebido em 10/11/2009
Aprovado em 15/12/2009













