Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista de Cirurgia e Traumatologia Buco-maxilo-facial
versão On-line ISSN 1808-5210
Rev. cir. traumatol. buco-maxilo-fac. vol.13 no.2 Camaragibe Abr./Jun. 2013
Teeth in the line of mandibular fractures: epidemiology, management and complications
Dentes em linhas de fraturas mandibulares: epidemiologia, manejo e complicações
Mariana SchafferI; Nelson Luis Barbosa RebellatoII; Luis augusto PasseriIII; Bruno Tochetto PrimoIV; Rafaela Scariot de MoraesV
I Senior Resident, Division of Oral and Maxillofacial Surgery, Curitiba Dental School, State University of Paraná, Curitiba, Paraná, Brazil
II Professor, Division of Oral and Maxillofacial Surgery, Curitiba Dental School, State University of Paraná, Curitiba, Paraná, Brazil
III Professor, Division of Oral and Maxillofacial Surgery, Piracicaba Dental School and Division of Plastic Surgery, School of Medical Sciences, State University of Campinas - Unicamp, São Paulo, Brazil
IV Resident of Oral and Maxillofacial Surgery, Federal University of Paraná, Curitiba, PR, Brazil
V Professor of the Resident of Oral and Maxillofacial Surgery, Federal University of Paraná, Curitiba, PR, Brazil
RESUMO
Objetivo: avaliar a incidência, as regiões mais afetadas, o manejo bem como as complicações encontradas em dentes envolvidos em linhas de fraturas mandibulares. Métodos: Os dados foram coletados a partir de prontuários de pacientes tratados com fraturas mandibulares. Foram incluídas informações como dados demográficos, localização da fratura, presença de dentes na linha de fratura e complicações. Resultados: a amostra apresentou um total de 310 linhas de fratura, e destas 144 tinham dentes envolvidos. a região mais afetada foi o ângulo, seguido da parassínfise, pelo corpo, pelo processo alveolar e pela sínfise. Observaram-se 196 dentes nas linhas de fraturas, 60 dos quais tinham sido retirados. Complicações pós-operatórias ocorreram em 8,6% da amostra. Dos casos que apresentaram complicações, pacientes sem dentes envolvidos na linha de fratura corresponderam a 43,75%, e os pacientes com dentes envolvidos na linha de fratura foram de 56,25%. Quando o dente foi removido, 8,47% dos pacientes apresentaram complicações, e, quando o dente foi mantido, 2,85%. Conclusão: este estudo demonstrou que a presença de dentes da linha de fratura não é um fator limitante para o tratamento. As complicações são mais frequentemente relacionadas com o método de tratamento escolhido do que para o envolvimento de dentes na linha de fratura.
Descritores: Fraturas Mandibulares; Dente não Vital; Complicações.
ABSTRACT
Purpose: To examine the incidence, the regions most affected, the management as well as the complications found in teeth involved in the line of mandibular fractures. Methods: Data were collected from patients records treated of mandibular fractures. It was included information such as demographic data, fracture location, presence of teeth in the line of fracture, treatment and complications. Results: The sample has presented a total of 310 lines of fracture, from these, 144 had teeth involved. The most affected area was the angle, followed by the parasymphysis, body, alveolar process and symphysis. There were 196 "fracture line" teeth, 60 of which had been removed. Postoperative complications occurred in 8.6% of the sample. From the cases that presented complications, patients without teeth involved in the fracture line ranged 43.75% and patients with teeth involved in the fracture line reached 56.25%. When the tooth was removed 8.47% of the patients presented complications and when the tooth was retained 2.85%. Conclusion: This study demonstrated that the presence of teeth in the line of fracture is not a limiting factor for the treatment. The complications are more frequently related to the chosen method of treatment than to the involvement of teeth in the line of fracture.
Keywords: mandibular fracture, jaw fracture, complications, tooth nonvitality.
INTRODUCTION
The mandible is the area of the face with major incidence of fracture. Its prominence and position in the skeletal face predispose to frequent traumas. Some studies1 have demonstrated that it is really common to observe teeth in the line of fractures. Others authors2 mentioned that the presence of the teeth can be one of the determinant factor of the fracture location.
The management of teeth in the line of fracture had changed within the past years. In the past, it was thought that teeth in the line of fractures should be immediately removed3.
Although recent studies, support the vision that noninfected teeth in the line of fracture can be preserved4. The maintenance of these teeth can favor the treatment in some cases; therefore they contribute for the stability of the fracture. Its removal can be harmful, once that can diminish the contact between fragments, cause additional trauma to the region, increase the risk of contamination of the fracture through the empty alveolus, convert a closed fracture into an open fracture and cause the loss of the bony bunch in the zone of tension.
Each case must be evaluated individually, for maintaining or not the teeth in the fracture line, depending on the clinical and radiographic findings 4. A great variety of opinions has been observed when relating to management, prognostic of these teeth and method of treatment.
This study aimed at to carry through a survey epidemiologist of the patients with mandibular fractures treated in the Department of Oral and Maxillofacial Surgery, of the XV Hospital Ltda., Curitiba, Brazil, in a period of 18 years to evaluate the frequency of teeth in the line of fractures, the area that they were found, the management and the complications associated.
METHODS
Patients treated in the Department of Oral and Maxillofacial Surgery of the XV Hospital Ltda., Curitiba, Brazil who had presented mandibular fractures, in the period between February - 1986 and October - 2004, had completed records and a minimum postoperative follow-up care of six months, were included in this study.
It was examined the following variables: age, sex, etiology of the fractures, fracture location (angle, parasymphysis, body, alveolar process, symphysis), tooth presence in the line of fracture, management with these teeth, method of treatment and associated complications.
The criteria used for the management of teeth in the line of mandibular fractures, was based on the guidelines published by Shetty and Freymiller 4 which indicates: (1) Intact teeth in the fracture line should be left in situ if they shown no evidence of severe loosening or inflammatory change; (2) Impacted molars, especially complete bony impactions, should be left in place to provide a larger repositioning surface. Exceptions are partially erupted molars with pericoronitis or those associated with follicular cyst; (3) Teeth that prevent reduction of fractures should be removed; (4) Teeth with crown fractures may be retained provided that emergency endodontic therapy is carried out. All teeth with fractured roots must be removed; (5) Teeth with exposed root apices, or where the fracture line follows the root surface from the apical region to the gingival margin, tend to develop pulpal or periodontal complications which may adversely affect healing. These should be carefully monitored; (6) Teeth that appear nonvital at the time of injury should be retained; (7) Treatment should be performed as early as possible; (8) Primary extraction is recommended when extensive damage to the periodontium and supporting alveolus has occurred.
RESULTS
During the studied period, 203 patients with mandibular fractures have been treated in the department, of these, 17 patients without complete records or postoperative follow-up care for at least six months were eliminated from the study.
The 186 patients consisted of 50 (26,89%) females and 136 (73,11%) males. They had an average age of 26,7 years with a range from one to 78 years.
It was identified 310 fractures in the 186 treated patients, of those, 85 (45, 69%) had a single fracture, 78 (41,93%) had two lines of fractures and 23 (12,36%) had three lines of fractures.
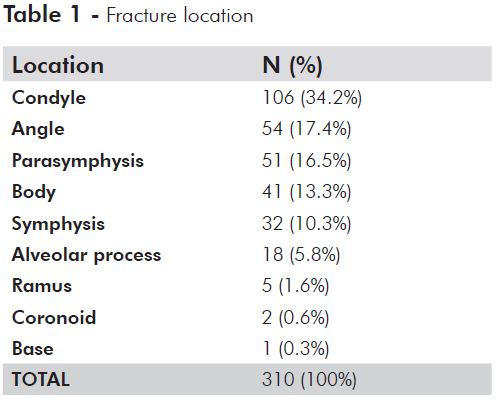
Fracture location is distributed in TABLE 1. In the 186 analyzed patients, 67 (35,83%) had not presented tooth in the line of fracture, and 119 (64,17%) patients had teeth involved in at least one of the lines of fracture. Of a total of 310 lines of fracture, 166 (53,54%) lines were not involved with teeth and 144 (46,45%) presented teeth.
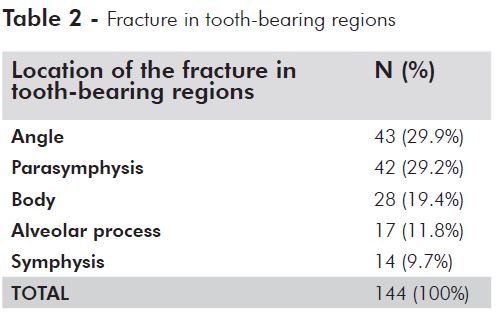
The 144 lines of fracture in tooth-bearing regions are distributed in TABLE 2.
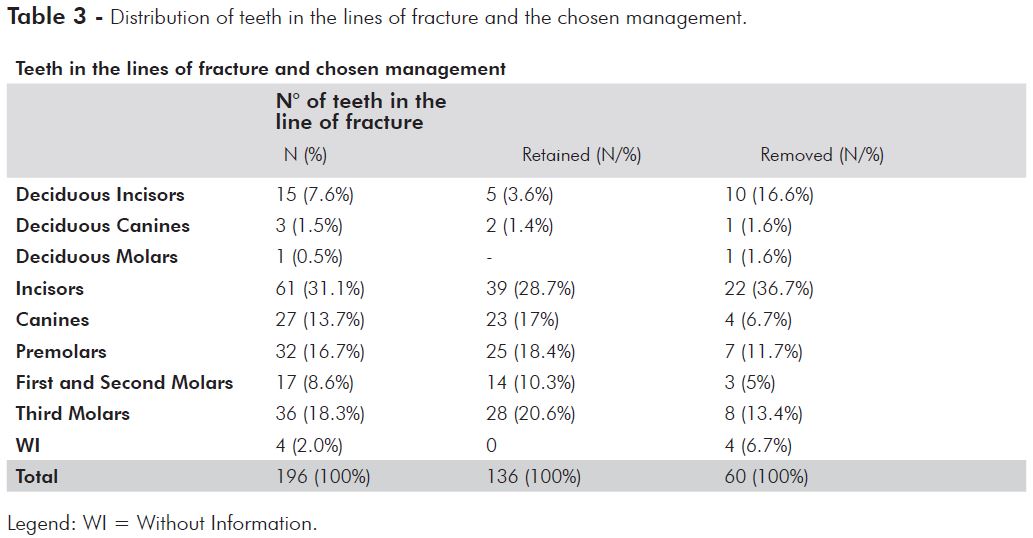
There were 196 teeth in lines of fracture. The central incisors (61 teeth – 31.1%) and the third molars (36 teeth – 18.3%) had been the teeth with the most prevalence,, the other teeth observed, as well as the chosen management, are distributed in TABLE 3.
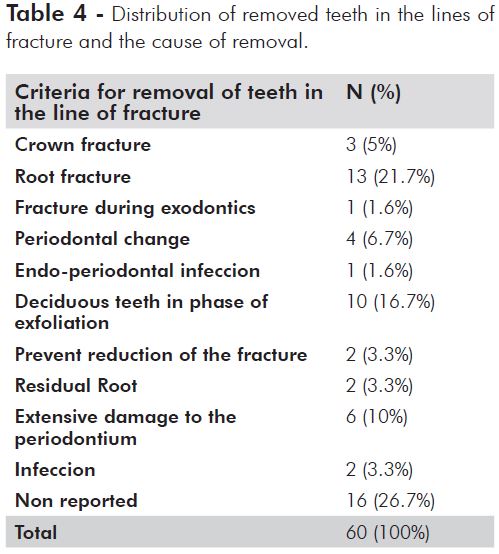
In concern of teeth in line of fractures, 136 (69.4%) had been retained and 60 had been removed (30,6%), the number of extracted teeth related to its cause is distributed in TABLE 4.
As for the adopted method of treatment, 189 fractures had been treated surgically. The rigid internal fixation with miniplates and screws was the most used method (85 fractures). Osteosyntheses with transosseous wires and maxillomandibular fixation was applied in 81 fractures. Other 23 fractures had been reduced surgically, however without any type of internal fixation, only applying maxillomandibular fixation.
The conservative treatment was used in 121 fractures, in which, 119 had been treated with maxillomandibular fixation and only two cases with proservation and soft diet, due to age and general conditions of the patients.
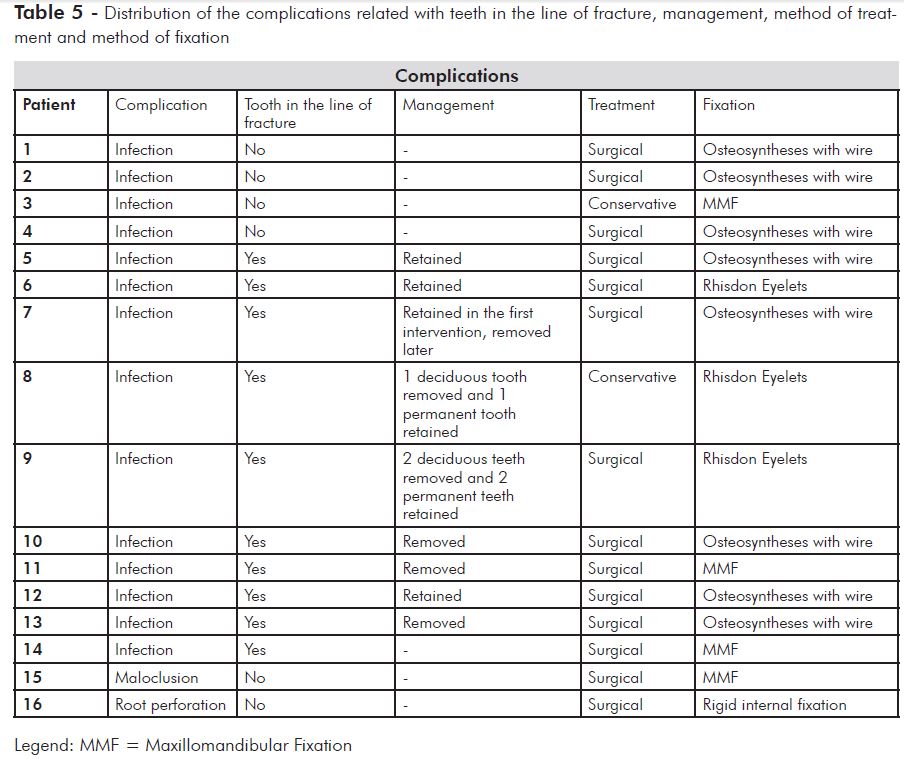
Complications had been found in 16 patients (8,6%), infection was the most found and affected 14 patients. Moreover there was a malocclusion case and a radicular perforation case during the fixation of the fracture, in which later was necessary endodontic procedures.
Relating the method of treatment used in patients with postoperative complications, it was noticed that 14 patients had been treated surgically (eight patients treated with osteosyntheses with wire, two with eyelets, two with maxillomandibular fixation, one with cerclage and one with rigid internal fixation with miniplates) and two patients with conservative procedures.
In the 14 patients with infection, five did not present tooth associated with the line of fracture and others nine presented teeth in the line of fracture. In three cases the teeth had been removed during the first intervention. In two cases of patients with deciduous and permanent teeth associated with the line of fracture, the deciduous teeth had been removed and the permanent ones retained. Four patients had retained the tooth in the line of fracture, from which only one needed to be removed for complete resolution of the infection.
It is important to point out that 110 patients with teeth in the line of fracture had not presented any kind of complication. Table 5 is a summary of fixationthese situations.
DISCUSSION
Considerable controversy still exists as to whether impacted or partially erupted mandibular teeth associated with fractures of the mandibular should be removed at the time of fracture reduction. Some studies5,6 demonstrate the distribution of the location and the number of lines in mandibular fracture and present among them a slight variation in the predominance of these elements. This study demonstrated that the most common was the occurrence of one line of fracture per mandible, the most affected regions were the condyle, angle and parasymphysis. It seems to be sufficiently evident that the anatomical conformation, its prominence in the face, the action of the inserted musculature in each region and mainly the mass of the objects, intensity, speed and direction of the forces that collided to the mandible during the traumas, are responsible for the type and the location of the fracture. The condyle was the most affected area, which differs from studies carried through for James5 and Sinn 6 who had observed a higher incidence rate in the angle region.
In this study it was identified 144 lines of fracture in tooth-bearing regions, 46.45%, a value close to the incidence observed by Neal et al.1, who reported that 50% of the fractures had teeth involved in the line. Fuselier et al.7, noted that patients with third molar (M3) present had a 2.1 times greater chance of an angle fracture than did patients without and there was a statistically significant variation in the risk for an angle fracture depending on M3 position. In the study of Ma'aita and Alwrikat A8, in the 426 patients with an M3, 127 (29.8%) had angle fractures. Of the 189 patients without an M3, 25 (13.2%) had angle fractures.
The central incisors and the third molars had been the teeth more frequently associated with the lines of fracture, close to the results observed in other studies which also show that the third molars were more frequent1, the difference may be that these studies exclude alveolar fractures from their report.
The incidence of angle fractures is significantly higher in patients with unerupted third molars than in those without. The region of the mandibular angle with an unerupted third molar is an area of lowered resistance to external forces9. Reitzik et al.10 showed that a mandible with unerupted third molars required 40% less force to fracture it than one with fully erupted third molars, and they suggested that the unerupted third molars could weaken the mandible because the tooth occupied more of the osseous space. According to this theory, if the tooth was buried deeper this would increase this risk. To Halmos et al.11 that there is a greater risk of angle fractures when the third molar is present, and a variable risk depending on the position of the third molar. According to Kober et al.12 the resistance of the mandibular angle increases when the third molar is erupted or absent, which causes the force to be transmitted to a more fragile region, the condyle. Patil PM13, suggest that if the mandibular angle is made more resistant to fracture under a traumatic force, such trauma would create a fracture elsewhere, particularly the mandibular condyle.
Teeth in the line of fracture had been removed in 30.10% of the cases. A total of 140 teeth was retained and only in one patient exodontics was necessary in one tooth after the first intervention so that the infectious could be despoiled, therefore, the result of the obtained success was 99.29% of "safe" teeth. Berg and Pape14 in their study had found that 23% of teeth in the lines of fracture had been extracted during the first intervention and only one tooth electively retained needed extraction, which means, 98% had been safe successfully. Wagner et al15 had 37 cases of mandibular angle fractures with teeth in the line of fracture that were treated with an open reduction and found a complication rate of 11.8% in those fractures in which the teeth were retained and 35% when teeth were removed. Rubin et al.16, when comparing open and closed reduction of the mandibular angle fracture associated with an impacted or partially erupted third molar tooth, the incidence of complications in the open reduction group was 25% and in the closed reduction group was 20%. And when comparing extraction of the tooth and retention of the tooth, the complication rate was 19% and 23%, respectively.
It is generally accepted by most surgeons that antibiotic therapy should be administered when teeth are left in the line of fracture because of open nature and contamination of the oral cavity. Penicillin is still considered the drug of choice17.
Kamboozia and Punnia-Moorthy,18 recommend that teeth associated with mandibular fracture should not be removed on a prophylactic basis to reduce the risk of infection of fracture sites just if there is an absolute indication for removal, and when retained they should be followed up clinically and radiographically for at least 1 year with a view to endodontic treatment if indicated. Patients with teeth in the fracture line showing no response on pulp vitality testing should be advised extraction to avoid further complications19. There is an increased risk for postoperative complications when a tooth is present, but the increase is not statistically significant. The incidence of postoperative infection and/or the need for plate removal is not affected by whether the tooth in the fracture is removed20. The socioeconomic status of the patient, nutritional status, oral hygiene, abusive habits, and other factors may all play a role in the outcomes from treatment.
In cases in which the deciduous predecessor was lost at the time of injury, the space for the tooth involved in the fracture should be preserved. Careful attention should also be paid to preventing infection and to avoiding injury to the tissue in the follicles during surgical reduction. Repeated radiographic follow-up after the initial treatment is necessary in the cases in which infection around the tooth bud is observed, the tooth bud is rotated, or a surgical wire or miniplate placed near the tooth bud is confirmed after surgery.
The rate on complications with teeth in the line of fracture is similar to the ones found by James5 in his study, who observed that from the 261 fractures of the mandible associated with teeth, 15 (5,35%) had become infected postoperatively.
In this study, 9 patients (4.83%) with teeth in the fracture line, values lower than those of the Ellis E 3rd20 study when the incidence of infection in patients who had no tooth associated with the angle fracture was 15.8% compared with 19.1% in those who did. For angle fractures associated with a tooth, when the tooth was retained, the incidence of infection was 19.5%. When it was removed, the incidence was 19.0%20. The only complication found in the patients treated surgically with rigid internal fixation was a root perforation, therefore this complication, is related to the deficiency in the surgical technique and not to the stability of the material or the tooth presence in the line of fracture.
CONCLUSIONS
The study demonstrated that the teeth presence in the line of mandibular fracture is not a limiting factor for the treatment, moreover its presence was not significant statistically in the development of complications. Complications had been more frequently related to the chosen method of treatment than to the teeth presence in the line of fracture. The low rate of complications found in the study, allows concluding that the chosen method of treatments had been efficient.
Conflict of interest
The authors declare that they have no conflict of interest.
Sources of support that require acknowledgment: None.
REFERENCES
1. Neal DC, Wagner WF, Alpert B. Morbidity associated with teeth in the line of mandibular fractures. J Oral Surg 1978; 36:859-862 [ Links ]
2. Amaratunga NA. A comparative study of the clinical aspects of edentulous and dentulous mandibular fractures. J Oral Maxillofac Surg 1988; 46:3-5 [ Links ]
3. Bradley RL. Treatment of fractured mandible. Amer Surg 1965; 31: 289-290 [ Links ]
4. Shetty V, Freymiller E. Teeth in the line of fracture: A review. J Oral Maxillofac Surg 1989; 47:1303-1306 [ Links ]
5. James RB, Fredrickson C, Kent JN. Prospective study of mandibular fractures. J Oral Surg 1981; 39: 275-281 [ Links ]
6. Sinn DP. Mandibular Fractures. Selected Readings In Oral And Maxillofacial Surgery 1991; 5: 1-18. [ Links ]
7. Fuselier JC, Ellis EE 3rd, Dodson TB. Do mandibular third molars alter the risk of angle fracture?. J Oral Maxillofac Surg 2002; 60:514-518 [ Links ]
8. Ma'aita J, Alwrikat A. Is the mandibular third molar a risk factor for mandibular angle fracture?. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89:143-6 [ Links ]
9. Krimmel M, Reinert S. Mandibular fracture after third molar removal. J Oral Maxillofac Surg 2000;58: 1110–1112.
10. Reitzik M, Lownie JF, Cleaton JP, Austin J. Experimental fractures of monkey mandibles. Int J Oral Surg 1978; 7:100–103.
11. Halmos DR, Ellis III E, Dodson TB. Mandibular third molars and angle fractures. J Oral Maxillofac Surg 2004; 62:1076–1081.
12. Kober C, Sader R, Thiele H. Stress analysis of the human mandible in standard trauma situations with numerical simulation (in German). Mund Kiefer Gesichtschir 2001; 5:114–9.
13. Patil PM. Unerupted lower third molars and their influence on fractures of the mandibular angle and condyle. Br J Oral Maxillofac Surg 2011; Jul 15. [ Links ]
14. Berg S, Pape HD. Teeth in the fracture line. Int J Oral Maxillofac Surg 1992 ; 21: 145-146 [ Links ]
15. Wagner WF. Neal DC. Alpert B. Morbidity associated with extraoral open reduction of mandibular fractures. J Oral Surg 1979; 37:97-100. [ Links ]
16. Rubin MM, Koll TJ, Sadoff RS. Morbidity associated with incompletely erupted third molars in the line of mandibular fractures. J Oral Maxillofac Surg 1990; 48:1045-7 [ Links ]
17. Spinnato G, Alberto PL. Teeth in the line of mandibular fractures. Atlas Oral Maxillofac Surg Clin North Am 2009; 17:15-18. [ Links ]
18. Kamboozia AHAH, Punnia-Moorthy A. The fate of teeth in mandibular fracture lines. A clinical and radiographic follow-up study. Int J Oral Maxillofac Surg 1993; 22: 97-101 [ Links ]
19. Samson J, John R, Jayakumar S. Teeth in the line of fracture: to retain or remove? Craniomaxillofac Trauma Reconstr 2010; 3:177-84. [ Links ]
20. Ellis E 3rd. Outcomes of patients with teeth in the line of mandibular angle fractures treated with stable internal fixation. J Oral Maxillofac Surg 2002; 60:863-865. [ Links ]
 Endereço para correspondência:
Endereço para correspondência:
Mariana Schaffer
Mailing address: 95, Joaquim Gonçalves de Barros St., Curitiba, Paraná, Brazil
Postal code: 82600-440
e-mail: marianaschaffer@ig.com.br













