Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista de Cirurgia e Traumatologia Buco-maxilo-facial
versão On-line ISSN 1808-5210
Rev. cir. traumatol. buco-maxilo-fac. vol.14 no.2 Camaragibe Abr./Jun. 2014
Atypical Typical Avulsion Zygomatic Bone Fracture
Fratura Avulsiva Atípica de Zigona
Caroline Comis GiongoI; Fernando GiovanellaI; Marcos Antonio TorrianiII
I DDS, Esp
II DDS, MSc, PhDIII Acadêmica do curso de Odontologia da Faculdade de Odontologia da Universidade de Passo Fundo, Passo Fundo, RS, Brasil.
ABSTRACT
Avulsion injuries of facial bones are rare, as well as accounts regarding the management of these lesions. This study describes a facial trauma that resulted from a bull gore, which caused the avulsion of the zygomatic bone, which was left hanging by only a small pedicle. The case study involved a 36 year old male leukoderma patient who sought the Maxillo-Facial Surgery and Trauma Department at the Emergency Unit in Pelotas-RS (Brazil). Clinical examination showed extensive laceration of the face in the middle third area on the left side, with the avulsion of the zygomatic body, causing the displacement of the eyeball towards the maxillary sinus. Treatment included bone and eyeball repositioning, zygoma fixation and suture, yielding good aesthetic and functional results. The peculiarity of the etiology and the particular features of the trauma are highlighted.
Descpriptors: Zygomatic bone; Facial trauma; Zygomatic complex fractures.
RESUMO
Lesões avulsivas dos ossos faciais são raras, assim como descrições quanto ao manejo dessas injúrias. Este estudo descreve um traumatismo facial decorrente de uma chifrada de um boi, que ocasionou a avulsão do osso zigomático, restando preso apenas por um pequeno pedículo. Trata-se de um paciente gênero masculino, 36 anos, leucoderma, que procurou o serviço de Cirurgia e Traumatologia Buco-Maxilo-Facial do Hospital de Pronto-Socorro da cidade de Pelotas-RS (Brasil). Ao exame clínico observava-se extensa laceração na face, em área de terço médio, lado esquerdo, com avulsão do corpo do zigoma, determinando o deslocamento do globo ocular em direção ao seio maxilar. O tratamento constou de reposicionamento ósseo e do globo ocular, fixação do zigoma e sutura, obtendo-se um bom resultado estético e funcional. Destaca-se a peculiaridade da etiologia e características únicas deste trauma.
Descritores: Osso zigomático; Trauma facial; Fraturas do complexo zigomático.
INTRODUCTION
Avulsion lesions of facial bones are quite rare, and result mainly from high-powered mechanisms in which the major force vector is tangentially directed to the cranium, often causing the resulting bone segment to become a free non-vascularized graft.1
Only two similar cases have been found in literature. Yokoo et al.1 reported the case of a 26 year old male patient who suffered avulsion of the zygomatic bone following a car crash in 2002. The avulsed zygoma had an intact 51 periosteum and, after wash with amikacin sulfate and dimethylsulfoxide, was kept at -80º C for 40 days. Such procedure was adopted due to subarachnoid hemorrhage and temporal bone fracture, insofar as these traumas required treatment priority. After the neurosurgical staff had been released, the zygomatic bone was reimplanted through the laceration scar and fixated by means of plates and screws in its anatomical position. After 6 months the bone graft incorporation was considered satisfactory and after a four-year period a discrete resorption was observed.
The second case of zygoma avulsion was reported by Colin-Duran et al.2 60 upon referring to a 42 year old male patient who was victim of a car accident which resulted in severe traumatic brain injury and extensive laceration of the cheek. The bone had been stripped of its periosteum due to the frictional forces of the accident, and was kept in saline in the freezer. The zygoma was repositioned 36 h after the trauma, and fixated by means of plates and screws in the infraorbital rim, the frontozygomatic suture and the zygomatic arch. An excellent bone graft volume was observed in the immediate postoperative and three-month follow-up by computerized tomography (CT) scan. However, another 24 month follow-up scan revealed significant zygomatic bone resorption.
Because these events are so rare, treatment should be planned quickly, which may be difficult due to the unprecedented condition, sometimes demanding a breach of protocol. Associated to this, there are material difficulties that imply the adoption of solutions which are not always the ideal ones.
This study reports a trauma resulting from a bull gore that caused avulsion of the zygomatic bone, which was left hanging by a small pedicle only. The peculiarity of the etiology and the particular features of the trauma are highlighted.
CASE REPORT
A 36 year old male leukoderma patient sought the Maxillo-Facial Surgery and Trauma Department at the Emergency Unit in Pelotas-RS (Brazil) after suffering an accident in a rodeo, where he had been wounded by a bull gore.
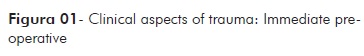
Upon physical examination, edema and periorbital hematoma, subconjunctival ecchymosis, hypoesthesia in the nostril, upper lip and upper anterior teeth, an extensive laceration of the face in the middle third area with the avulsion of the left zygomatic bone – which was hanging by a pedicle only – were found (Figure 1). As there had been avulsion of the zygomatic bone, including the orbital floor, the eyeball was displaced towards the maxillary sinus. Posteroanterior maxillary sinus (Waters' view) and Hirtz axial radiographs were requested so as to complement clinical observations, in which total displacement of the left zygomatic bone was observed, as demonstrated by the patient's clinical condition. At the time of trauma, the emergency unit lacked a CT scan machine.
Once the absence of ophthalmic or neurological injury was evidenced, the patient was immediately referred to the surgery center.
In order to access the frontozygomatic area, a superciliary incision was performed in which a n. 1 steel wire, emerging in the lacerated area and transfixing the frontal process of the zygomatic bone, was introduced. Following, the zygomatic bone was repositioned through traction by the steel wire together with the careful lifting of the eyeball with a Minnesota cheek retractor for the proper accommodation of the orbitalfloor. Then osteosyntheses in the frontozygomatic and zygomaticomaxillary suturesbwere done providing, from a clinical transurgical viewpoint, adequate stability for the fractured structured. Soft tissues had their edges smoothed and sutured.
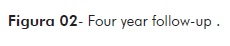
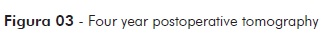
The patient had weekly follow-up for a 4-week period, and after that a monthly followup for a 6-month period. Presently, four years after surgery, he shows good aestheticand functional recovery (Figure 2 and 3) without loss of visual acuity or eye motility.
DISCUSSÃO
Fractures involving the zygomatic complex are one the most common injuries of the maxillofacial complex. Because of its location and projection in the facial skeleton, the zygomatic complex has a significant incidence of injuries, in addition to playing a fundamental role in facial aesthetics.3
There is controversy in literature as to zygomatic bone fracture incidence. Whereas some studies claim that these fractures are the second or third most frequent, with a 17 to 40% average prevalence4. Ferreira et al.5 and Cheema3report these are the most frequent fractures. This shows that the epidemiological results obtained with reference to zygomatic fractures tend to vary according to the geographical area, socioeconomic status, culture, time of year and assistance characteristics.
The etiological peculiarity of the present report (bull-gored victim) is in agreement with that of Sands et al.6 who claimed that the etiology of zygomatic complex fractures is heterogeneous and directly related to individual population characteristics.
Studies where only zygomatic bone fractures were analyzed 125 reveal that their major cause are traffic accidents.3,7,8 This may be due to the fact that young people are able to drive cars and motorcycles at an earlier age, often at high speed; in addition, many of these youngsters are not used to wearing seat belts and local traffic laws and regulations can be less strict in different places.
The age (36) and sex (male) are in agreement with the studies of Motamedi4 and Cheema3, who reported that the highest prevalence of fractures of the zygomatic bone is between 21 and 40 years of age, and that the main victims are males, independently of the studied population.
The method of choice for bone fixation should offer the most direct and simple way for a successful reduction and real fixation, considering the fact the surgeon must restore the patient's normal functions and appearance, or at least bring as close to normal as possible.7,9
This study case reports a rare fracture, insofar as there was virtually the complete avulsion of the zygoma. In spite of displacement severity in this fracture, the positive result obtained was mainly due to the non-comminution of the zygomatic bone, and this is especially true of the orbital floor forming section. This allowed an adequate repositioning of the eyeball, which was displaced towards the maxillary sinus without leaving any sequelae, both in relation to visual acuity and impairment of eye movement or diplopia.
As to aesthetics, there was also a favorable result, due to fact the laceration occurred coincidentally in the nasolabial fold area, thereby being much less noticeable.
Regarding the method of fixation that was used, plates and screws would have been more appropriate. However, at the time of the accident, the emergency unit did not always have such materials available for immediate use. As an immediate surgical intervention was recommended, the available procedure at the time (osteosynthesis with steel wire) was used, which, though not ideal, helped us follow the principles of a functionally stable fixation: anatomical reduction, the use of a technique that would cause as little trauma as possible, suitable fixation, and early operational results.
The method of treatment used is in agreement with the principles advocated by Kloch & Gilliland7 and Lew9, who claimed that the ideal method of treatment aiming at obtaining both functional and aesthetic satisfactory results with minimal complication depends not only on the type and location of the fracture, but also on the experience and preferences of the surgeon.
In cases of treatment of zygomatic bone avulsion reported by Yokoo et al.1, several factors were mentioned that could optimize results, such as the vascularization of the recipient site, rigid internal fixation, presence of periosteum, and the use of conservation techniques aiming to decrease the metabolic activity of osteoclasts. However, the scarcity of cases prevents more accurate inferences on which the most important or fundamental factors for a successful treatment are. As to the possibility of resorption, Colin-Duran et al.2 suggest that a rich blood supply and stabilization are not enough to avoid it, given the fact that they found extensive bone resorption 24 months after reimplantation. In the case studied, after 2 years, no resorption signs can be observed. The patient has regained good aesthetics and function, with significant sequelae of the trauma he had suffered.
It can be concluded that the synthesis material is a technique facilitator but not the only result determinant.
FINAL CONSIDERATIONS
Surgical treatment of unusual traumas is always challenging, as it demands quick solutions which often do not follow regular protocols. Such being the case, the choice of the best treatment depends on several factors, among which are the kind of trauma, associated lesions, available resources and professional experience.
Thus, although surgeons seek ideal methods of treatment, they need to be prepared to face the hardships that still occur in the professional environment. At times the professional is faced with situations where the lack of resources is a limiting factor to his actions, so that he will have to choose the best treatment available in order to achieve the best possible result for the patient.
DECLARATIONS
Funding: None Competing Interests: None Ethical Approval: Not required Patient Consent: Patient consent obtained.
REFERENCES
1. Yokoo S, Tahara S, Sakurai A, et al.: Replantation of an avulsed zygomatic bone as a freeze-pre served autologous graft: a case report. J Craniomaxillofac Surg. 2003 Apr;31(2):115-9. [ Links ]
2. Colin-Durand J, Parker WL, Crepeau RJ: Repair of an Avulsed Zygoma: Defining Optimal Management. J Oral Maxillofac Surg. 2008 Dec;66(12):2615-6. doi: 10.1016/j.joms.2007.06.67
3. Cheema SA: Zygomatic bone fracture. J Coll Physicians Surg Pak. 2004 Jun;14(6):337-9.
4. Motamedi MH: An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg. 2003 Jan;61(1):61-4.
5. Ferreira P, Marques M, Pinho C, Rodrigues J, Reis J, Amarante J: Mid facial fractures in children and adolescents: a review of 492 cases. Br J Oral Maxillofac Surg. 2004 Dec;42(6):501-5.
6. Sands T, Symington O, Katsikeris N, Brown A: Fractures of the zygomatic complex: a case report and review. J Can Dent Assoc. 1993 Sep;59(9):749-55, 757.
7. Kloch DW, Gilliland R: Internal fixation versus conventional therapy in midface fractures. J Trauma. 1987 Oct;27(10):1136-45.
8. Gomes PP, Passeri LA, Barbosa JRA: A 5-year retrospective study of zygomatic-orbital complex and zygomatic arch fractures in Sao Paulo state, Brazil. J Oral Maxillofac Surg. 2006 Jan;64(1):63-7.
9. Lew D: Midfacial trauma: Diagnosis and treatment. Oral and Maxillofac Surg 1991, 6:1-28.
 Endereço para correspondência:
Endereço para correspondência:
Faculade de Odontologia de Pernambuco - FOP
Av. Gal. Newton Cavalcanti, 1650 - Tabatinga
Camaragibe/PE - CEP: 54753-220













