Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista de Cirurgia e Traumatologia Buco-maxilo-facial
versão On-line ISSN 1808-5210
Rev. cir. traumatol. buco-maxilo-fac. vol.14 no.4 Camaragibe Out./Dez. 2014
Carcinoma in situ in a patient with erythroleukoplakia: challenges in the diagnosis and in the therapeutic choice
Short title: Carcinoma in situ in erythroleukoplakia
Willian Pecin JacomacciI; Liogi Iwaki FilhoII; Lilian Cristina Vessoni IwakiII; Mariliani Chicarelli da SilvaII; Neli PielarisiII; Vanessa Cristina VeltriniII; Rafael de Oliveira LazarinIII; Elen de Souza TolentinoIV
I Undergraduate Student at Maringá State University, Maringá-PR, Brazil.
II DDS, MA, PhD, Associate Professor, Department of Dentistry, Maringá State University, Maringá-PR, Brazil.
III DDS, MA applicant in Dentistry at Maringá State University, Maringá-PR, Brazil.
IV DDS, MA, PhD, Assistant Professor, Department of Dentistry, Maringá State University, Maringá-PR, Brazil.
ABSTRACT
A 41-year-old Caucasian male smoker presented a red and white plaque on the left jugal mucosa suggestive of oral erythroleukoplakia (OEL). Biopsy followed by microscopic examination revealed carcinoma in situ. Since OEL is considered a precancerous lesion with a high malignant transformation potential, the present case set out to discuss the challenges in diagnosing the condition and choosing the most appropriate treatment. The discussion deals with issues such as whether there is a limit for choosing either a radical or a more conservative approach to treatment and the importance of using a procedure that allows a microscopic examination of the entire lesion. Carcinoma in situ associated with OEL made the treatment planning even more complex in the present case. In order to avoid a mutilating approach, multiple excisions with safety margins were performed, and the patient was instructed not to smoke. A strict 12-month follow-up shows no signs of recurrence of the OEL.
Descriptors: Erythroplasia; Leukoplakia; Primary Treatment.
INTRODUCTION
Oral erythroleukoplakia (OEL), sometimes likened to speckled or nodular leukoplakia, is a red and white plaque with a relatively high risk of malignant transformation.1 Tobacco and alcohol are major risk factors associated with its malignant potential.2,3
OEL shows a higher malignant transformation potential than homogeneous leukoplakia,2-4 which can be partially demonstrated by histological and immunohistochemical examinations and cohort studies. The malignant transformation rate of OEL ranges from 18% to 47%, whereas it is around 1-7% for homogenous thick oral leukoplakia (OL), and 4-15% for granular or verruciform OL.5 Histologically, OEL lesions are characterized by epithelial changes of hyperkeratosis, hyperplasia, atrophy, a certain degree of epithelial dysplasia, carcinoma in situ, or superficially invasive carcinoma. In addition, OEL lesions have higher mitotic and apoptotic indices than homogeneous and nodular OL lesions6.
The management of potentially malignant disorders can be challenging. Clinical treatment consists of the elimination of risk factors,7 follow-up,8 use of retinoids,9 vitamins A, C, E, ketorolac, celecoxib, green tea, fenretinide, lycopene,10 and photodynamic therapy.5,11-14 Surgical treatment consists of lesion removal, cryosurgery, and laser ablation.15
The aims of this study were (1) to report the clinical and histological details of OEL on the jugal mucosa, and (2) to review the literature regarding OEL's demographic, clinical, and histological features, as well as its prognosis and treatment.
CASE REPORT
A 41-year-old Caucasian male smoker attended the Oral Medicine Clinic of the State University of Maringá, Brazil, reporting an asymptomatic lesion on the left side of the jugal mucosa of unknown time of development. Intraoral examination showed a red plaque near the premolar region and a white nodular plaque around the molar region (Fig. 1).
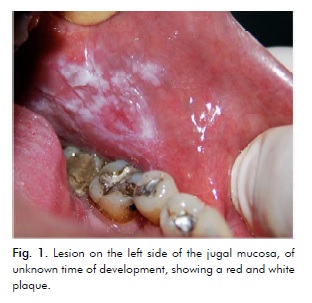
The presumptive diagnosis was either OEL or squamous cell carcinoma. Biopsy samples were collected from the more posterior white nodular region and from the more anterior red region.
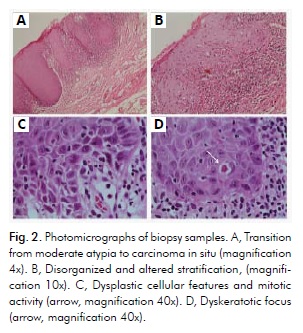
Histopathological examination using haematoxylin and eosin staining revealed hyperkeratosis and atrophy, with focal carcinoma in situ in the more anterior red region, compatible with carcinoma in situ in OEL. The examination also revealed hyperkeratosis with moderate dysplasia in the more posterior white region, compatible with a diagnosis of OL. The stratified squamous epithelium covering the mucosa exhibited varying degrees of orthoandparakeratosis, with rhomboid crest cells showing hyperchromatism and pleomorphism in approximately half of the epithelial thickness. However, a smaller area showed more evident dysplastic features throughout the epithelium, but with no signs of an infiltrative pattern (Fig. 2A). The features consisted of disorganized and altered stratification, drop projections alternating with atrophy (Fig. 2A and 2B), an unusual nucleocytoplasmic ratio, hyperchromatism, pleomorphism, loss of intercellular adhesion with infrequent mitotic figures (Fig. 2C), and dyskeratotic foci (Fig. 2D). The connective tissue underlying these areas showed more intense inflammatory changes.
The clinical and microscopic features were consistent with a diagnosis of OEL associated with a focal carcinoma in situ. At this stage, the patient was given a thorough explanation on his treatment options: (1) he could be referred to a neck and head surgeon, who would probably use an invasive approach, whether or not associated with radiotherapy; (2) he could undergo outpatient treatment at the Oral Medicine Clinic with a more conservative approach that would preserve both esthetic and functional aspects. The patient chose the second option and signed the appropriate Informed Consent Form (Appendix A).
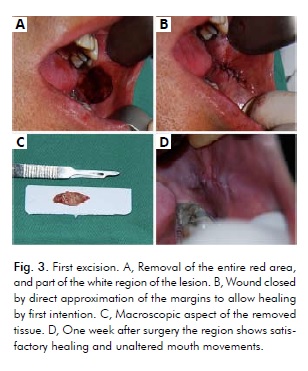
Owing to the extensive size of the lesion and the fact that a single large excision could restrict mouth movements, surgical procedures consisted of three multiple excisions using a scalpel, performed within a 2-month period, with a 30-day interval between each procedure. Due to the presence of carcinoma in situ in the red region, the first procedure consisted of its entire excision, as well as part of the white area of the lesion, using a 5-mm security margin (Fig. 4). In addition, the patient was instructed to stop smoking.
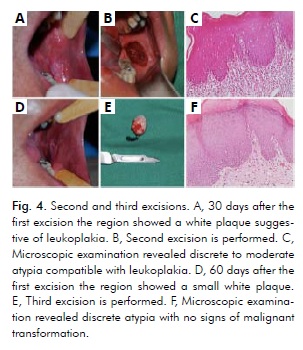
The clinical examination one month after the first excision showed a white plaque suggestive of leukoplakia (Fig. 4A). The second excision was then performed (Fig. 4B), and microscopic examination revealed discrete to moderate atypia (Fig. 4C). Intraoral examination two months after the first excision showed a small white plaque even more posteriorly located than before (Fig. 4D). Next, the third excision was performed (Fig. 4E), which revealed discrete atypia (Fig. 4F). Both the second and third excisions were performed in the more posterior molar region using the same 5-mm security margin. The tissues of these two excisions were compatible with leukoplakia with no signs of malignant transformation (Fig. 4C, Fig. 4F).
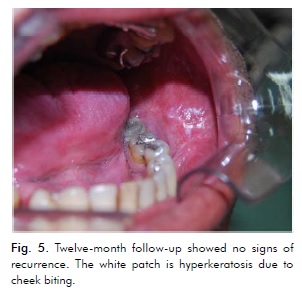
The patient stopped smoking and is under strict follow-up, having been seen weekly during the first three months, monthly up to one year, and every three months after that. No signs of recurrence were observed 15 days after the third and final excision, confirmed at the 12-month follow-up appointment (Fig. 5).
DISCUSSION
OEL is considered a non-homogeneous leukoplakia with mixed white and red plaques and has a high risk of malignant transformation.2-4 The red or erythroplakia areas seem to be more likely to undergo dysplastic changes than the white hyperkeratotic ones,7 as found in the present case, the most atypical cells being observed in the red region. Yen et al. (2008)16 found that betel quid and cigarette use resulted in a 42.2% risk of developing leukoplakia and a 95.0% one of developing OEL after 20 years of follow-up. The patient in the present case had smoked approximately ten cigarettes per day for 20 years and the initial biopsy revealed carcinoma in situ associated with OEL.
Because the treatment modalities for OEL are variable, choosing the appropriate therapy can be challenging. Taking into consideration its stage of development and its high malignant potential, one might wonder whether treatment should be either conservative or invasive. In order to verify the most used modalities of treatment, we reviewed the literature on this issue. The sources were Medline and Lilacs databases, the texts must have been written in English, and the searching terms were oral AND nonhomogeneous OR no homogeneous AND leukoplakia OR erythroleukoplakia. Non-homogeneous leukoplakia was used, since many authors consider it a synonym for erythroleukoplakia. Eight studies on the treatment of OEL were found,5,7,14,16-19 published between 1987 and 2010. Of the total 226 cases, 211 were treated by means of a clinical approach (photodynamic therapy and clinical follow-up), and 15 were treated with surgical excision (Table 1).
As for the clinical approach, photodynamic therapy (PDT) is used in the treatment of potentially malignant disorders because it is non-invasive, is well tolerated by patients, can be used repeatedly with no cumulative side effects, and results in little scar formation. 5,11,13,14 However, this technique showed variable success, inconsistent follow-up results, and recurrence.17 Indeed, recurrence of the disease using PDT may vary between 21%5 and 29%14.
A double-blind placebo-controlled study [Sankaranarayanan et al (1997)]17 found that vitamin A and beta-carotene, both used alone, showed better results on homogeneous leukoplakias and smaller lesions. Thus, the use of either vitamin A or betacarotene was questionable in the present case, due to the size of the lesion and the associated carcinoma in situ.
The traditional treatment for OEL consists is its complete excision,15,21,22 particularly for lesions with severe dysplasia.21,22 Complete excision allows histological analysis of the entire lesion, which may reveal alterations undiagnosed in the preoperative biopsy.8 Moreover, to the best of our knowledge, long-term studies have yet to demonstrate whether or not recurrence occurs after non-surgical treatment.20,23 Two out of the eight studies reviewed used surgical excision to treat OEL,8,19 with recurrence rates varying from 10.1%19 to 20%8.
The present study opted for a surgical approach as the biopsy had revealed an initial malignant transformation. In addition, multiple excisions associated with security margins were chosen because of the large size of the lesion, for a large wound could limit mouth movements and complicate postoperative recovery. This option also allowed supplementary microscopic examinations, which revealed different degrees of atypia, which guided the treatment. Particular care was taken during surgical procedures not to cover the opening of the parotid duct in order to prevent glandular atrophy and avoid further complications such as mucocele or reduction of the salivary flow. The wound was closed by direct approximation of the margins, allowing healing by first intention, and no significant reduction of mouth opening.
Vedtofte et al (1987)8 state that the mucosal defect caused by excisions can be repaired by second intention or closed using other techniques, such as direct approximation of the wound margins, transposition by a local mucosal flap, free mucosal graft, and free split skin transplant. As far as we know, there is no study using alloplastic grafts on potentially malignant lesions whose treatment can cause large defects. Although transplants can be used to recover broad surgical sites, as advocated by several authors,8,24 they may be infected by Candida sp, undergo postoperative contraction, deformities, and mask early signs of recurrence8.
Laser and cryotherapy can be used alone or associated with traditional surgical methods for the treatment of OEL. Cantarelli Morosolli et al. (2006)7 report a successful case of the disease treated with excision and carbon dioxide laser radiation. Cohort studies found that laser surgery plays an important role in the diagnosis and treatment of the potentially malignant lesions.10,18,25,26 The use of cryosurgery, though reported in the literature,9 share with laser ablation the major disadvantage of not providing the entire lesion for histological examination.27,28 In addition, cryotherapy causes considerable postoperative pain and swelling, and potentially malignant lesions are rarely completely destroyed.10
Vedtofte et al. (1987)8 found that premalignant lesions treated by surgical excision showed a general recurrence rate of 20%, often diagnosed within the first post-operative year. Most OEL recurrences were found in the areas adjacent to the previously treated lesion. The recurrence of erythroplakia and verrucous leukoplakia was 40% and 55.6%, respectively. Leukoplakia showed no recurrence. Two cases of OEL transformed into carcinoma, as well as one case of verrucous leukoplakia. Recurrences of potentially malignant lesions were often adjacent to the excised lesion, possibly because the 3-5 mm-security margin did not remove the entire pathologically changed tissue. The authors consider surgical excision a satisfactory treatment for potentially malignant lesions and emphasize the importance of using a technique that allows histological examination of the entire lesion.
Difficulties in determining the exact margin of a lesion are particularly frequent for erythroplakia or OEL,8 which may account for the high recurrence rate of these lesions. In order to avoid leaving pathological tissues at the surgical site and minimize the risk of recurrence, the present study opted for multiple excisions. Mouth movements are normal and there are no signs of recurrence. In addition, the risk of recurrence and malignant transformation is reduced with the elimination of risk factors, such as tobacco and alcohol cessation. The patient was instructed to stop smoking, and did stop cigarette use, being currently under strict follow-up.
In the present case report, a conservative modality of surgical treatment of OEL was proposed. Although still a surgical procedure, it is minimally invasive compared to traditional approaches used by both head and neck surgeons and oncologists. Their typical approach consists of more radical and extensive excisions that usually result in mutilation and impairment of both aesthetic appearance and function. The decision on whether to adopt a radical or a more conservative approach is a difficult one to make, as research thus far has not established a single protocol for handling such cases. The choice of treatment of cases like the present one requires a careful assessment of individual circumstances, taking into account the degree of cellular atypia, the location of and access to the lesion, as well as its size. We believe that, in principle, these lesions should not be treated as malignancies, thus enabling us to avoid the routine protocol of large resections and adjuvant therapies, such as radiotherapy. In addition, we believe that one has to keep in mind that carcinoma in situ is not invasive. Its surgical removal, along with the cessation of risk factors, such as tobacco, as well as constant monitoring can translate into successful treatment. Furthermore, multiple surgeries allowed multiple microscopic investigations, which afforded the patient a more reassuring prospect and the assurance that there were no malignant cells in the region.
REFERÊNCIAS
1. Küffer R, Lombardi T. Premalignant lesions of the oral mucosa. A discussion about the place of oral intraepithelial neoplasia (OIN). Oral Oncol. 2002;38:125-30. [ Links ]
2. Van der Waal I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol. 2009;45:317-23.
3. Van der Waal I. Potentially malignant disorders of the oral and oropharyngeal mucosa; present concepts of management. Oral Oncol. 2010;46423-5.
4. Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36:575-80.
5. Yu CH, Lin HP, Chen HM, Yang H, Wang YP, Chiang CP. Comparison of clinical outcomes of oral erythroleukoplakia treated with photodynamic therapy using either light-emitting diode or laser light. Lasers Surg Med. 2009;41:628- 33.
6. Kövesi G, Szende B. Changes in apoptosis and mitotic index, p53 and Ki67 expression in various types of oral leukoplakia. Oncology. 2003;65:331-6.
7. Cantarelli Morosolli AR, Schubert MM, Niccoli- Filho W. Surgical treatment of erythroleukoplakia in lower lip with carbon dioxide laser radiation. Lasers Med Sci. 2006;21:181-4.
8. Vedtofte P, Holmstrup P, Hjørting-Hansen E, Pindborg JJ. Surgical treatment of premalignant lesions of the oral mucosa. Int J Oral Maxillofac Surg. 1987;16:656-64.
9. Kleier C, Werkmeister R, Joos U. [Zinc and vitamin A deficiency in diseases of the mouth mucosa]. Mund Kiefer Gesichtschir. 199;2:320-5.
10. Thomson P. Oral Precancer – Diagnosis and Management of Potentially Malignant Disorders. Hoboken: Wiley-Blackwell: 2012; p. 107-136.
11. Dolmans DE, Fukumura D, Jain RK. Photodynamic therapy for cancer. Nat Rev Cancer. 2003;3:380-7.
12. Lee MR, Ryman W. Erythroplasia of Queyrat treated with topical methyl aminolevulinate photodynamic therapy. Australas J Dermatol. 2005;46:196-8.
13. Chen HM, Yu CH, Tsai T, Hsu YH, Kuo RC, Chiang CP. Topical 5-aminolevulinic acidmediated photo-dynamic therapy for oral verrucous hyperplasia, oral leukoplakia and oral erythroleukoplakia. Photodiagn Photodyn Ther. 2007;4:44–52.
14. Lin HP, Chen HM, Yu CH, Yang H, Wang YP, Chiang CP. Topical photodynamic therapy is very effective for oral verrucous hyperplasia and oral erythroleukoplakia. J Oral Pathol Med. 2010;39:624-30.
15. Reichart PA, Philipsen P. Oral erythroplakia: a review. Oral Oncol. 2005; 41:551–61.
16. Yen AM, Chen SC, Chang SH, Chen TH. The effect of betel quid and cigarette on multistate progression of oral pre-malignancy. J Oral Pathol Med. 2008;37: 417-22.
17. Sankaranarayanan R, Mathew B, Varghese C, Sudhakaran PR, Menon V, Jayadeep A, Nair MK, Mathews C, Mahalingam TR, Balaram P, Nair PP. Chemoprevention of oral leukoplakia with vitamin A and beta carotene: an assessment. Oral Oncol 1997; 33: 231-6.
18. Schoelch ML, Sekandari N, Regezi JA, Silverman S Jr. Laser management of oral leukoplakias: a follow-up study of 70 patients. Laryngoscope 1999; 109: 949-53.
19. Pandey M, Thomas G, Somanathan T, Sankaranarayanan R, Abraham EK, Jacob BJ, Mathew B. Evaluation of surgical excision of nonhomogeneous oral leukoplakia in a screening intervention trial, Kerala, India. Oral Oncol. 2001;37:103-9.
20. Spinola Ribeiro A, Ribeiro Salles P, da Silva TA, Alves Mesquita R. A Review of the nonsurgical treatment of oral leukoplakia. Int J Dent 2010; Article ID 186018, 10 pages, 2010. doi:10.1155/2010/186018.
21. Marley JJ, Cowan CG, Lamey PJ, Linden GJ, Johnson NW, Warnakulasuriya KA. Management of potentially malignant oral mucosal lesions by consultant UK oral and maxillofacial surgeons. Br J Oral Maxillofac Surg. 1996;34:28-36.
22. Marley JJ, Linden GJ, Cowan CG, Lamey PJ, Johnson NW, Warnakulasuriya KAAS, Scully C. A comparison of the management of potentially malignant oral mucosa lesions by oral medicine practitioners and oral and maxillofacial surgeons in the UK. J Oral Pathol Med. 1998;27: 489-95.
23. Lodi G, Sardella A, Bez C, Demarosi F, Carrasi A. Intervations for treatings oral leukoplakia. Cochrane Database Syst Ver. 2006;4:CD001929.
24. Frame JW, Das Gupta AR, Dalton GA, Evans EH. Use of the carbon dioxide laser in the management of premalignant lesions of the oral mucosa. J Laryngol Otol. 1984;98:1251-60.
25. Stocker J, Thomson PJ, Hamadah O. Laser surgery in oral oncology – the Newcastle experience. The Surgeon 2005; Suppl 3: S32-33.
26. Hamadah O, Thomson PJ. Factors affecting carbon dioxide laser treatment for oral precancer: a patient cohort study. Lasers Surg Med 2009; 41: 17-25.
27. Roodenburg JLN. CO2-laserchirurgie van leukoplakie van het mondslijmvlies [dissertation]. Groningen: University of Groningen; 1985. Available at: http://irs.ub.rug.nl/ ppn/852297629 (accessed July 8, 2013).
28. Sako K, Marchetta FC, Hayes RL Cryotherapy of intraoral leukoplakia. Am. J. Surg. 1972:124:482-4.
 Endereço para correspondência:
Endereço para correspondência:
Willian Pecin Jacomacci
Universidade Estadual de Maringá
Av. Mandacarú 1550. CEP 87.083-240
Maringá- PR, Brasil
e-mail: willianpjacomacci@gmail.com
Recebido para publicação: 06/06/2014
Aceito para publicação: 30/06/2014













