Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista Odonto Ciência (Online)
versão On-line ISSN 1980-6523
Rev. odonto ciênc. (Online) vol.25 no.3 Porto Alegre Jul./Set. 2010
ORIGINAL ARTICLE
Clinicopathological and demographic characteristics of ameloblastomas in a population from Bahia, Brazil
Características clinicopatológicas e demográficas de ameloblastomas em uma população da Bahia, Brasil
Francisco de Assis Caldas Pereira; Leonardo de Araújo Melo; Clarissa Araújo Silva Gurgel; Maria Cristina Teixeira Cangussu; Roberto Almeida de Azevedo; Jean Nunes dos Santos
Dental School, Federal University of Bahia, Salvador, BA, Brazil
ABSTRACT
PURPOSE: The present study aimed to review a series of ameloblastoma cases by observing their clinicopathological and demographic characteristics. The data in this study were compared to previous studies.
METHODS: Seventy ameloblastoma cases were obtained from the archive of the Surgical Pathology Service of the Dental School of the Federal University of Bahia and were analyzed with regards to age, gender, clinical manifestation, radiographic aspect, anatomical distribution and histological subtype. These data were submitted to statistical analysis.
RESULTS: Of the 70 cases, 35 (50%) occurred in males and 35 (50%) in females. Young adults were most affected by tumors. Fifty-six (80%) of all tumor cases occurred in the jaw. The main histological subtype seen was unicystic ameloblastoma, which occurred in 35 cases. The majority of the tumors [n=57 (81.4%)] were treated with radical surgery. The differences in clinical aspects and anatomical distribution were shown to be statistically significant (P<0.001).
CONCLUSION: The clinical-epidemiological profile of the patients in the present study is similar to that in other populations, with unicystic ameloblastoma being the most common histological subtype seen.
Key words: Ameloblastoma; jaw; odontogenic tumors
RESUMO
OBJETIVO: O presente estudo se propôs a revisar uma série de casos de ameloblastomas, observando-se as suas características clinicopatológicas e demográficas. Adicionalmente, os dados foram comparados com estudos prévios.
METODOLOGIA: Setenta casos de ameloblastomas foram recuperados dos arquivos do serviço de Patologia Cirúrgica da Faculdade de Odontologia da Universidade Federal da Bahia e analisados quanto a idade, sexo, manifestação clínica, aspecto radiográfico, distribuição anatômica e subtipo histológico. Esses dados foram submetidos à análise estatística.
RESULTADOS: Dos 70 casos, 35 (50%) acometeram o sexo masculino e 35 (50%) o sexo feminino. Os adultos jovens foram os mais afetados pelos tumores. A mandíbula foi o sítio preferencial, correspondendo a 56 casos (80%) do total dos tumores analisados. O principal subtipo histológico encontrado foi o ameloblastoma unicístico, que acorreu em 35 casos. A maioria dos tumores [n=57 (81,4%)] foi tratada cirurgicamente de forma radical. Dados em relação ao aspecto clínico e distribuição anatômica apresentaram-se estatisticamente significantes (P<0,001).
CONCLUSÃO: O perfil clínico- epidemiológico dos pacientes do presente estudo é similar ao de outras populações, sendo que o ameloblastoma unicístico é o subtipo histológico mais comum em nossa população.
Palavras-chave: Ameloblastoma; mandíbula; tumores odontogênicos
Introduction
Odontogenic tumors are lesions derived from epithelial and/or ectomesenchymal components of developing teeth or associated structures. These tumors represent only 1% of all jaw tumors (1-3). Among odontogenic tumors, ameloblastomas and odontomas are the more prevalent pathological patterns (3-7). Ameloblastoma is a benign epithelial tumor with no ectomesenchymal component; it has aspects of aggressiveness and local invasion but is also asymptomatic and slow-growing (8-12).
Radiographically, ameloblastomas present as multilocular and unilocular radiolucent lesions surrounded by a radiopaque border (10,13), located primarily in the posterior mandibular segment (2,7-9,12-14). Histologically, ameloblastoma can be subdivided in four types: solid, unicystic, peripheral and desmoplastic. In relation to cellular pattern and organization, ameloblastoma can be classified into five subtypes: follicular, plexiform, acanthomatous, granular ameloblastomas cells and basal cells ameloblastomas (11-15). These subtypes can occur in isolation or in combination (15,16).
The present study aimed to analyze a series of ameloblastoma cases diagnosed in a Diagnosis and Treatment Center in Oral and Maxillofacial Pathologies, as well as perform a demographic study of these lesions. In addition, we compared the data obtained in this study with that of previous studies.
Methods
After approval by the Institutional Ethics Committee (Protocol 36/08), 70 ameloblastoma cases were obtained from the Surgical Pathology Laboratory archive of the Dental School of the Federal University of Bahia, Salvador, Brazil, between January 2001 and July 2009. Data with regard to age, gender, clinical manifestation, radiographic aspect, anatomical distribution and histological subtype were analyzed. The histopathological diagnosis was reviewed and classified by an experienced oral pathologist (J.N.S.)based on World Health Organization classification from 2005 (OMS). Regarding tumor location, maxillary cases were considered unique, independent of their anterior or posterior position. Mandible cases were divided into anterior (symphysis and parasymphysis), posterior (corpus and ramus) and hemimandible (in cases with very extensive lesions in the anterior-posterior direction).
Statistical analysis was conducted on the distribution of absolute and relative frequencies of variables of interest. In addition, the difference in disease occurrence was tested by the chi-square test assuming a significance level of 5%.
Results
During a period of 8 years, a total of 3,070 biopsies were sent to the Surgical Pathology laboratory. Of these, 70 had a confirmed diagnosis of ameloblastoma, representing 2.2% of total cases.
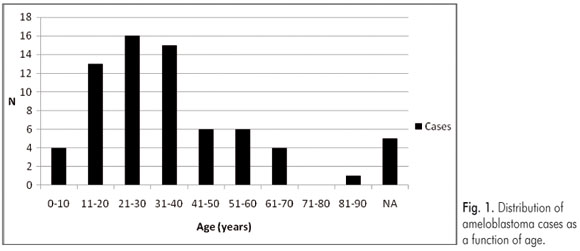
Of the 70 cases, 35 (50%) were in males and 35 (50%) were in females, making a male/female ratio of 1:1. Young adults in their second, third and fourth decades of life were most affected by the tumors. The patient age varied from 3 to 82 years, with an average of 31 years of age at the time of diagnosis.
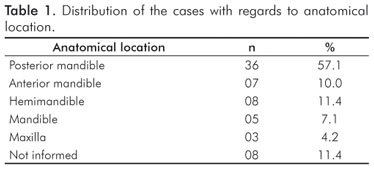
The anatomical sites of all the intraosseous tumors are presented in Table 1. In general, the mandible was the most common site, corresponding to 56 cases (80.0%) of all analyzed tumors. Of these cases, the posterior region was affected more often than the anterior segment and the hemimandible. (P<0.001). Some lesions that involved the mandible did not have their exact location recorded, thus it was not possible to evaluate the antero-posterior extension of these tumors. The maxilla was less affected, with the mandible to maxilla ratio being 18.6:1.
The main clinical feature of tumors was a swelling of the affected region (n=40; 57.1%). This was statistically significant in relation to less frequent signs and symptoms such as pain (n=7; 10%), ulcers (n=1; 1.4%), dental mobility (n=4; 5.7%), root reabsorption (n=2; 2.8%) and fistula (n=1; 1.4%) (P<0.001).
In the large majority of cases (n=38; 54.2%), the radiographic aspects were not recorded in the clinical records. In 15 cases (21.4%), a multilocular radiolucent appearance was observed and two cases had a soap bubble or honeycomb-like appearance. Unilocular radiolucent lesions were observed in 17 cases (24.2%).
Unicystic ameloblastoma was the most commonly histological subtype seen. Data related to patients' ages and genders are presented in Table 2. The mandible was the most commonly affected location, with 31 cases (88.5%), while only one lesion (2.85%) was observed in the maxilla. Of the 17 cases where the radiographic aspect was indicated, 14 (82.3%) corresponded to unilocular lesions, whereas 3 (17.6%) had a multilocular appearance.
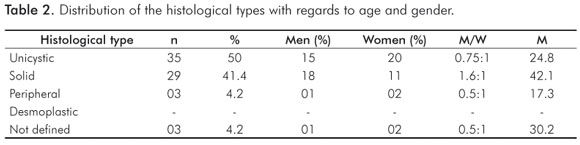
Solid ameloblastoma was the second most commonly diagnosed histological type. Table 2 presents the relation of this tumor type with the patients' ages and genders. This variant presented greater predilection for the mandible, with 22 lesions diagnosed in this site (31.4%), whereas only two cases (2.85%) were observed in the maxilla. In relation to the radiographic aspect, all ten lesions where the radiographic aspect was recorded were multilocular. Of the 22 solid ameloblastoma cases where the histological organization of the lesion was known, 14 were follicular (63.6%), 3 were plexiform (15%) and 5 cases were judged to be both follicular and plexiform (22.7%).
The peripheral variant was the least frequent subtype. However, its location was reported in only two cases with this lesion, one in the oral mucosal region corresponding to the posterior mandibular area and one in the anterior gingival region of the maxilla (see Table 2).
The majority of the tumors (n=57; 81.4%) were treated with a radical form of surgery, including ample bone resection with a safety margin of healthy bone of about 1 cm. Only 13 (18.5%) young patients (< 19 years) with unicystic ameloblastomas were treated conservatively with enucleation or curettage.
Discussion
Despite the increasing literature about odontological tumors, specifically ameloblastoma, little is known about the clinicopathological aspects and frequency of these tumors in Brazil. The prevalence of ameloblastomas varies from 11.7% to 80.3% in relation to other odontological tumors in different populations (2-5,8,17). This bias can be explained by the fact that the relative incidence of ameloblastoma is greater than is reported, due to underreporting of odontomas in many studies, primarily those from Africa and Asia. This occurs because studies from these regions are generally carried out at large hospital centers where ameloblastoma frequency is greater and also due to the lower quantity of odontoma diagnosis because it is an asymptomatic lesion that is primarily diagnosed through routine radiographic examinations (1,7,18).
In accordance with Ledesma-Mountes et al. (12), studies based only on previously published data in the literature do not represent the true prevalence of ameloblastomas and the statistical analyses are difficult to interpret. Thus, studies with information obtained from diagnosis services present better and more trustworthy results. Therefore, we opted to develop a study based on the Surgical Pathology Service archives. However, there were some limitations in regards to underreporting of some data, such as location and radiographic aspect, in the clinical records. Moreover, because this is a cross-sectional study of a retrospective nature, we could not access postoperative and follow-up information.
Table 3 presents a comparative analysis of this study with other works published in the English literature since the year 2000. The relative frequency of ameloblastomas, histological and clinical data are compared.
In general, ameloblastoma does not have a gender preference, with men and women being affected equally, as seen in the present study (9,10,12). However, studies from India and Nigeria revealed a greater occurrence in men (3,5), while studies from Brazil and Kenya indicated a greater prevalence in women (2,17).
In the present study, ameloblastoma occurred more often in the second, third and fourth decades of life, although practically every age range was affected. This is similar to findings from other studies reported in India (3), Brazil (2,17) and Nigeria (5). According to Kim and Jang (14), the frequency of ameloblastoma in young patients (< 19 years) is relatively low, occurring in only 10 to 15% of all reported cases. Our results show a greater frequency, around 25%, for this group of individuals. In addition, our findings were very similar to those observed by Chidzonga et al. (9), who showed that two thirds of the patients affected by ameloblastomas were less than 40 years of age.
There is a consensus in the literature that ameloblastoma more frequently affects the mandible, primarily in its posterior region (2,4,8,9,13,14,17,19,20). This was also observed in the present study, where a statistically significant difference was observed. Some authors state that the lesion site in the mandibular bone is related to the individual's race, with the posterior region more frequently involved in Caucasians and Japanese, while in blacks, especially those of African origin, the anterior/sinfisal bone segment (3,15,21) is a more common disease site. It was not possible to establish such a comparison in the present study.
In accordance with the reports of several authors (8,10,19), the primary clinical manifestation of ameloblastoma is increased slow swelling in the area affected by the tumor. Our results were statistically significant for this variable and are in accordance with previous reports. Moreover, other less frequent symptoms, such as pain, paresthesia, ulceration, and dental mobility, among others, can be present (8,9,15).
The multilocular radiolucency appearance surrounded by a radiopaque border is the most common radiographic appearance of ameloblastoma (15). In a study conducted in Nigeria by Arotiba et al. (19), the authors observed that almost 66% of the cases corresponded to multilocular lesions. Nevertheless, Kim and Jang (14) conducted a study in Korea and reported that almost 60% of cases were composed of unilocular ameloblastomas, while approximately 20% were multilocular. It is difficult to compare data from this study with previous reports, as there was underreporting of the radiographic characteristics in the clinical reports.
In relation to the frequency of the different ameloblastoma histological subtypes, the results of the present study differ from previous reports from Estonia (4), Nigeria (5,19), Zimbabwe (9) and the United States (20), which demonstrated a greater occurrence of the solid tumor variant. Our findings are similar to those from Ledesma-Mountes et al. (12), who observed a greater prevalence of the unicystic subtype, although the difference between the solid and unicystic subtypes were not statistically significant in the present work. Peripheral and desmoplastic ameloblastomas are considered rare (21-23).
In the present study, unicystic ameloblastoma was more pre- valent in women, similar to findings from Latin America (12) and the United States (20), where a slightly increased prevalence in females has been reported. According to the OMS (11), this variant does not present a gender bias. Unicystic ameloblastoma tends to occur more frequently during the second and third decades of life, with a lower average age seen for the solid subtype, which more frequently affects the mandible and has a unilocular radiographic appearance (10,11,15,20). Those findings were confirmed in this study. However, some cases of apparently multilolocular radiolucent lesions were also observed for this variant.
Solid ameloblastoma was more common in men, with a male:female ratio of 1.6:1. These findings are in agreement with those found by Ledesma-Mountes et al. (12) and Buchner et al. (20), who also observed greater prevalence in males, despite data from the OMS (11) stating that there is no gender bias for this condition. Solid ameloblastomas had a greater prevalence in the fourth decade of life, with an average age at diagnosis of ~42 years. These data are very close to those found by Ledesma-Mountes et al. (12) and Buchner et al. (20), who recorded an average age of 41.1 and 48 years, respectively. According to data from the OMS (11), the mandible, specifically the posterior region, is the most affected area by both multilocular and unilocular lesions. However, in this study, only multilocular lesions were verified.
Peripheral ameloblastoma is a tumor of varying clinical behavior that occurs in soft tissues associated with the mandible and maxilla. It presents histological characteristics similar to those observed in tumors located in the jaw bones (23). Although it is difficult to establish comparisons because we only found 3 cases, the present study showed only one case among males, in contrast with Buchner, Merrell and Carpenter (23). The average age of patients affected by this condition is significantly greater compared to those who present intraosseous ameloblastomas (1,11,21,23). However, in our study, peripheral ameloblastoma cases were found among younger patients. In addition, Reichart, Philipsen and Sonner (21) also found that the mandible was the most affected bone, in particular the anterior region. However, this cannot be proved in this study.
There are two basic histopathological subtypes of solid ameloblastoma with clinical relevance: the follicular and plexiform patterns (11). The present study is in accordance with the findings by Adebiyi et al. (16), which revealed a greater frequency of the follicular type over the plexiform type for solid ameloblastomas.
In accordance with various authors (24,25), the solid variant is the most aggressive form of ameloblastoma, whereas a relatively less aggressive behavior is associated with the unicystic standard. Thus, the former is commonly managed with radical treatment including extensive bone resection, while the latter is treated in a more conservative manner through enucleation or curettage. In their studies, Carlson and Marx (24) and Pogrel and Montes (25) stated that ameloblastoma should not be treated in a conservative manner because this method is associated with increased reoccurrence rates. In agreement with these authors, the surgery service from our university opts for radical treatment. Only young patients (< 19 years) presenting unicystic tumors are treated conservatively. In agreement with our study, Al-Khateeb and Ababneh (15) agreed that extensive bone resection in a young patient caused a sufficiently negative psychological effect and a deep impact on maxillofacial region growth and function, thus necessitating more conservative therapy for this group of patients.
Conclusions
The clinical epidemiological profile of the patients from the present study is very similar to other populations with regards to gender, age and tumor location, with unicystic ameloblastoma being the most common subtype in our population, in contrast to other reports.
Acknowledgments
We would like to thank all residents from the Surgery and Bucomaxilofacial Traumatology Service of the Federal University of Bahia and the PIBIC/CNPq.
References
1. Luo HY, Li TJ. Odontogenic tumors: a study of 1,309 cases in a Chinese population. Oral Oncology 2009;45:706-11. [ Links ]
2. Fernandes AM, Duarte ECB, Pimenta FJGS, Souza LN, Santos VR, Mesquita RA, Aguiar MCF. Odontogenic tumors: a study of 340 cases in a Brazilian population. J Oral Pathol Med 2005;34: 583-7. [ Links ]
3. Sriram G, Shetty RP. Odontogenic tumors: a study of 250 cases in an Indian teaching hospital. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:e14-e21. [ Links ]
4. Tamme T, Soots M, Kulla A, Karu K, Hanstein SM, Sokk A et al. Odontogenic tumors: collaborative retrospective study of 75 cases covering more than 25 years from Estonia. J Craniomaxillofac Surg 2004;32:161-5. [ Links ]
5. Adebiyi KJE, Odukoya O, Taiwo EO: Ectodermal odontogenic tumors: analysis of 197 Nigerian cases. Int J Oral Maxillofac Surg 2004; 33: 766-770. [ Links ]
6. Santos AC, Tarquinio SBC, Rívero ERC, Araújo LMA, Krause CL. Quantitative AgNORs study in ameloblastomas. Rev odonto ciênc 2009;24:10-4 [ Links ]
7. Guerrisi M, Piloni MJ, Keszler A. Odontogenic tumors in children and adolescents. A 15-year retrospective study in Argentina. Med Oral Patol Oral Cir Bucal 2007;12:E 180-5. [ Links ]
8. Olaitan AA, Adeola DS, Adekeye EO. Ameloblastoma: clinical features and management of 315 cases from Kaduna, Nigeria. J Craniomaxillofac Surg 1993;21:351-5. [ Links ]
9. Chidzonga MM, Lopez Perez VM, Portilla Alvarez AL. Ameloblastoma: the Zimbabwean experience over 10 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82:38-41. [ Links ]
10. Lagares DT, Cossió PI, Guisado JMH, Pérez JLG. Ameloblastoma mandibular. Mandibular ameloblastoma. A review of the literature and presentation of six cases. Med Oral Patol Oral Cir Bucal 2005;10:231-8. [ Links ]
11. World Health Organization Classification of Tumours. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005. [ Links ]
12. Ledesma-Montes C, Mosqueda-Taylor A, Carlos-Bregni R, Romero de León E, Palma-Guzmán JM, Paez-Valencia C, Meneses-Garcia A. Ameloblastomas: a regional Latin-American multicentric study. Oral Diseases 2007;13:303-7. [ Links ]
13. Mendenhall WM, Werning JW, Fernandes R, Malyapa RS, Mendenhall NP. Ameloblastoma. Amer J Clin Oncol 2007;30:645-8. [ Links ]
14. Kim SG, Jang HS. Ameloblastoma: A clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:649-53. [ Links ]
15. Al- Khateeb T, Ababneh KT. Ameloblastoma in Young Jordanians: A Review of the Clinicopathologic Features and Treatment of 10 Cases. J Oral Maxillofac Surg 2003;61:13-8. [ Links ]
16. Adebiyi KE, Ugboko VI, Omoniyi- Esan GO, Ndukwe KC, Oginni FO. Clinicopathological analysis of histological variantes of ameloblastoma in a suburban Nigerian population. Head & Face Med 2006;2:42. [ Links ]
17. Santos JN, Pereira Pinto L, Figueredo CRLV, Souza LB. Odontogenic tumors: analysis of 127 cases. Pesqui Odont Bras 2001;15: 308-13. [ Links ]
18. Fregnani ER, Fillipi RZ, Oliveira CRGCM, Vargas PA, Almeida OP. Odontomas and ameloblastomas: variable prevalences around the world? Oral Oncolgy 2002;38:807-8. [ Links ]
19. Arotiba GT, Ladeinde AL, Arotiba JT, Ajike SO, Ugboko VI, Ajayi FA. Ameloblastoma in Nigerian children and adolescents: a review of 79 cases. J Oral Maxillofac Surg 2005;63:747-51. [ Links ]
20. Buchner A, Merrell PW, Carpenter W. Relative frequency of central odontogenic tumors: a study of 1,088 cases from Northern California and comparison to studies from other parts of the world. J Oral Maxillofac Surg 2006;64:1343-52. [ Links ]
21. Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Oral Onco Eur F Cancer 1995;31:86-99. [ Links ]
22. Santos JN, Souza VF, Azevedo RA, Sarmento VA, Souza LB. Caracterização imuno-histoquímica de lesão híbrida de amelo- blastoma desmoplásico e convencional. Rev Bras Otorrinolaringol 2006;72:709-13. [ Links ]
23. Buchner A, Merrell PW, Carpenter WM. Relative frequency of peripheral odontogenic tumors: a study of 45 new cases and comparison with studies from the literature. J Oral Pathol Med 2006;35:385-91. [ Links ]
24. Carlson ER, Marx RE. The Ameloblastoma: Primary, Curative Surgical Management. J Oral Maxillofac Surg 2006;54:484-94. [ Links ]
25. Pogrel MA, Montes DM. Is there a role for enucleation in the management of ameloblastoma? Int J Oral Maxillofac Surg 2009;38:807-12. [ Links ]
 Correspondence:
Correspondence:
Jean Nunes dos Santos
Av. Araújo Pinho, 62, Canela
Salvador, BA – Brazil
40110150
E-mail: jeanunes@ufba.br
Received: December 22, 2009
Accepted: May 23, 2010
Conflict of Interest Statement: The authors state that there are no financial and personal conflicts of interest that could have inappropriately influenced their work.













