Serviços Personalizados
Artigo
Links relacionados
Compartilhar
Revista Odonto Ciência (Online)
versão On-line ISSN 1980-6523
Rev. odonto ciênc. (Online) vol.25 no.3 Porto Alegre Jul./Set. 2010
CASE REPORT
Orthodontic treatment of a midline diastema related to mesiodens and thumb-sucking habit
Tratamento ortodôntico de um diastema mediano relacionado a mesiodens e hábito de sucção digital
André Wilson MachadoI,II; Aldrieli Regina AmbrosioII; Sergei Godeiro F. Rabelo CaldasII; Luiz Gonzaga Gandini JúniorII
IGraduate Program in Orthodontics, Dental School, Federal University of Bahia, Salvador, BA, Brazil
IIDepartment of Pediatric Dentistry, Araraquara Dental School, UNESP, Araraquara, SP, Brazil
ABSTRACT
PURPOSE: Midline diastema due to simultaneous interplay of mesiodens and thumb-sucking habit is a very uncommon situation and can represent negative impact on esthetics and function. The purpose of this article is to describe a case report of a 9 year-old boy with a 9-mm midline diastema and an anterior open bite treated with an interceptive orthodontic approach.
CASE DESCRIPTION: After orthodontic diagnosis, treatment undertaken was the surgical removal of the mesiodens and the use of a palatal crib therapy in order to discontinue the thumb habit. Then, orthodontic brackets were bonded on maxillary central incisors and the diastema closed allowing the spontaneous irruption of the maxillary laterals incisors. When acceptable levels of overbite and overjet were achieved and the habit was controlled, the orthodontic treatment was discontinued.
CONCLUSION: To assure good results in managing pathological midline diastemas the diagnosis and treatment should be performed as early as possible.
Key words: Diastema; interceptive orthodontics; malocclusion
RESUMO
OBJETIVO: A associação de mesiodens com hábito de sucção digital como fatores etiológicos de diastemas medianos é uma situação clínica incomum e, quando presente, provoca um comprometimento estético e funcional. O objetivo desse trabalho é descrever o caso clínico de um paciente, aos 9 anos de idade, com mordida aberta anterior e um diastema mediano de 9 mm.
DESCRIÇÃO DO CASO: Após o diagnóstico ortodôntico, a conduta terapêutica foi a exodontia do mesiodens e instalação de uma grade palatina fixa para controle do hábito de sucção digital. Em seguida, bráquetes ortodônticos foram colados nos incisivos centrais superiores e o diastema foi fechado possibilitando a irrupção espontânea dos incisivos laterais. Quando adequados níveis de trespasse vertical e horizontal entre os incisivos foi alcançado e o hábito removido, o tratamento foi finalizado.
CONCLUSÃO: É importante ressaltar que com o objetivo de alcançar resultados estéticos e funcionais satisfatórios, minimizando sequelas ao desenvolvimento da oclusão deve-se realizar o diagnóstico precoce e intervenção imediata dos diastemas medianos patológicos.
Palavras-chave: Diastema; Ortodontia Interceptora; má oclusão
Introduction
During dental development the presence of a midline diastema and a supernumerary in the maxillary arch could be deleterious from the esthetic and functional views. Although the literature associates those problems as etiological factors to midline diastema, the presence of both situations in the same patient is very uncommon (1).
Supernumerary teeth are teeth in excess of the normal number (2). When located in the maxillary central incisor region a supernumerary tooth is called mesiodens and its prevalence has been estimated to be 0.15 to 2.2% of the population with a preference of male (3). Mesiodens is usually found to be impacted but also fully or ectopic erupted (3,4).
It is strongly advised that the diagnosis of mesiodens should be made as early as possible due to its associating with disturbances in tooth eruption such as delayed eruption of the permanent incisors, crowding or interference with the alignment of the maxillary incisors, dental impaction, resorption of adjacent tooth, development of dentigerous cist and one of the most common sequel, a midline diastema (2-4).
This last condition should be proper investigated since midline diastema larger than 2 mm in the mixed dentition should be fully investigated due to its relation to some disturbances in tooth eruption. In those situations, the main causes of midline diastemas are not only mesiodens but also congenitally missing teeth, peg-shaped lateral incisors, labial frenum, ethnic and racial characteristics, certain pathologic conditions and thumb-sucking habit (5).
Literature brings different approaches to solve mesiodens, midline diastemas and anterior open bite. Ultimately, options are the mesiodens removal, the orthodontic space closure of the diastema and the use of physical and psychological techniques to correct the cause of the thumb habit. It should be stated that the ultimate goal is to reestablish the normal dental development.
Since there is a lack of information in the literature regarding patients with midline diastemas associated to mesiodens, it is necessary to report clinical cases in order to facilitate the knowledge of this issue (6-8).
The purpose of this article is to show a case report of a 9 year-old boy with a Class II malocclusion with a 9-mm midline diastema and anterior open bite which was treated with a simple orthodontic interceptive approach achieving satisfactory results.
Description of the case
A Brazilian boy, aged 9 years and 7 months, of mixed ethnic background (black and white), was referred to the private office of the first author. His chief complaint was the presence of a large midline diastema. His medical and dental histories were uneventful.
Intraoral examination showed that the patient was in the mixed dentition, with the permanent maxillary central incisors and first molars already erupted. In addition, there was a 9-mm midline diastema associated with an erupted mesiodens. Moreover, there was an anterior open bite associated with thumb-sucking habit and a delay in the maxillary lateral incisors eruption. The molars on the right side were in Class I relationship, whereas in the left side were in Class II leading to a Class II, division 1 malocclusion (Fig. 1).
The treatment plan was designed to accomplish some clinical objectives such as the removal of the mesiodens, the discontinuation f the thumb-sucking habit to correct the open bite and the orthodontic closure of the midline diastema to allow proper eruption of the maxillary lateral incisors.
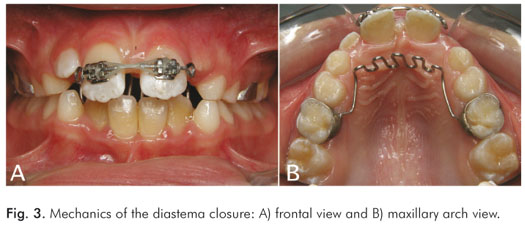
The first step in interception treatment was to proper inform the patient and his parents the need of discontinuing the thumb-sucking habit in order to reestablish the normal dental development. Surgical removal of the mesiodens was then performed, and after 2 months the diastema had spontaneous closed 1.5 mm (Fig. 2). At this stage, a palatal crib was placed to assist in the thumb-sucking habit control and tongue thrusting. Next, orthodontic 0.022" brackets were bonded on the labial surface of the maxillary central incisors, and a passive 0.021×0.025" sectional stainless steel archwire with chain elastics were placed to close the diastema (Fig. 3).
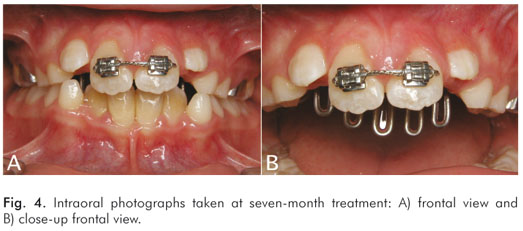
After five months, overjet and overbite were corrected, and diastema was closed leading to a spontaneous eruption of the maxillary lateral incisors (Fig. 4). At this stage, palatal crib was removed as well as the orthodontic brackets, and a palatal bonded retention was placed in the maxillary central incisors to avoid relapse.
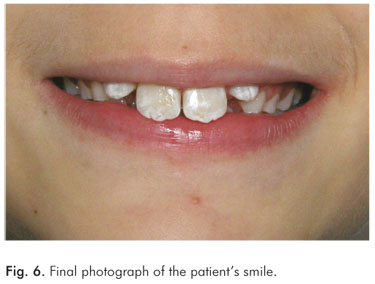
The analysis of the final photographs shows the reestablishment of normal dental development highlighting the efficiency and effectiveness of the treatment (Fig. 5). Furthermore, due to the esthetics improvement of the smile, the patient reported a higher level of self-confidence and was generally happier than in the original situation (Fig. 6).
Discussion
During dental development the interplay of different factors can cause some malocclusion. The case described here involved an interaction of two major factors, a mesiodens and a thumb-sucking habit leading to a 9-mm midline diastema and an anterior open bite.
The early diagnosis of large midline diastemas and erupted mesiodens is more common because they are located in the maxillary anterior region and are easily noticed by parents or general practitioners or pediatric dentists (9). Conversely, the case described here does not corroborate this idea because patient was referred to the orthodontist at the age of 9 years and 7 months, and theoretically the diastema and the mesiodens were present, according to the literature since 7.27 years, the physiological age of maxillary central incisors eruption (10).
Along with this problem since maxillary lateral incisors did not erupt in the dental arch at an expected age, which is 8.2 years (10), it can be characterized as an eruption delay. The reason of this situation was the presence of the mesiodens and diastema, which block the space for the lateral eruption. A simple orthodontic space opening could encourage the spontaneous eruption, which is a more logical and conservative approach (11).
The literature supports the cause/effect relation between the mesiodens and the midline diastema (6-8). The present clinical case shows this association, which was aggravated by the thumb-sucking habit.
Thus, there was a need of closing the diastema related to a mesiodens and a thumb-sucking habit. For the first problem the clinical option was the surgical removal of the mesiodens followed by the orthodontic closure of the remaining space. Interestingly, after the mesiodens removal, there was a 1.5 mm reduction in the diastema, which is probably related to the action of trans-septal fibers maintaining the dental aligning.
Although the physiological tendency is the spontaneous closure of the midline diastema after the eruption of the maxillary canines (5,6,12), in the case described a orthodontic approach was necessary to allow the eruption of the maxillary lateral incisors. Thus, orthodontic brackets were used achieving a satisfactory result, which is a simple and fast method (6-8). Since the rate of orthodontic diastema closure relapse is found to be 49% (13), a bonded retainer was used in the lingual surface of the maxillary central incisors.
In order to correct the thumb-sucking habit the treatment was based on two strategies. First the patient and his parents were informed about the deleterious effects of the habit and the need of stopping it in order to reestablish the normal dental development. In addition, a palatal crib was used for two reasons: as a reminder therapy and as a barrier to avoid tongue thrusting. The treatment objective was completely achieved in 5 months with the habit discontinued and the open bite closure showing the efficacy and efficiency of the approach undertaken. It is necessary to remember that in order to achieve good results patient compliance is of fundamental importance. The analysis of the esthetics results showed that not only the smile aspect was enhanced but also the patient reported a higher level of self-confidence and was generally happier, which is the ultimate treatment goal even in young patients (14,15).
In summary, although a simultaneous midline diastema and a mesiodens in the same patient is a very uncommon situation, it could be negative in the esthetic and functional views. There is a consensus in the literature towards an early diagnosis and treatment which increases the possibility of good clinical results and the reestablishment of normal dental development.
References
1. Yamaoka M, Furusa K, Yasuda W. Effects of maxillary anterior supernumerary impacted teeth on diastema. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:252. [ Links ]
2. Russel KA, Folwarczna MA. Mesiodens – diagnosis and manage ment of a common supernumerary tooth. J Can Dent Assoc 2003; 69:362-6. [ Links ]
3. Gündüz K, Çelenk P, Zengin Z, Sümer P. Mesiodens: a radiographic study in children. J Oral Sci 2008;50:287-91. [ Links ]
4. Roychoudhury A, Gupta Y, Parkash H. Mesiodens: a retrospective study of fifty teeth. J Indian Soc Pedo Prev Dent 2000;18:144-6. [ Links ]
5. Proffit WR, Fields HW. Ortodontia Contemporânea. 3ed. Rio de Janeiro: Guanabara Koogan; 2002. [ Links ]
6. Almeida RR, Garib DG, Almeida-Pedrin RR, Almeida MR, Pinzan A, Junqueira MHZ. Diastema Interincisivos centrais superiores: quando e como intervir? Rev Dental Press Ortodon Ortoped Facial 2004;9:137-56. [ Links ]
7. Tostes MA, Fernandes KP. Dente supranumerário e diastema mediano superior/ Supernumerary tooth and superior median diastema. RGO 1996;44:220-3. [ Links ]
8. Heluy DB, Portella W, Gleiser R. Supranumerário (mesiodente) e sua influência no diastema mediano superior: relato de um caso na F.O.UFRJ. Rev odontopediatr 1993;2:165-70. [ Links ]
9. Uematsu S, Uematsu T, Furusawa K, Degushi T, Kurihara S. Orthodontic treatment of an impacted dilacerated maxillary central incisor combined with surgical exposure and apicoectomy. Angle Orthod 2004;74:132-6. [ Links ]
10. Moyers RE. Ortodontia. 4. ed. Rio de Janeiro: Guanabara Koogan; 1991. [ Links ]
11. Becker A. Early treatment for impacted maxillary incisors. Am J Orthod Dentofac Orthop 2002;121:586-7. [ Links ]
12. Kurol J. Early treatment of tooth-eruption disturbances. Am J Orthod Dentofac Orthop 2002;121:588-91. [ Links ]
13. Shashua D, Artun J. Relapse after orthodontic correction of maxillary median diastema: A follow-up evaluation of consecutive cases. Angle Orthod 1999;69:257-63. [ Links ]
14. Machado AW, Loriato L, Souki B, Junqueira, T. Erupção espontânea de incisivos centrais superiores impactados após a abertura ortodôntica de espaço. Rev Clin Ortodon Dental Press 2007;5: 43-52. [ Links ]
15. Crawford LD. Impacted maxillary central incisor in mixed dentition treatment. Am J Orthod Dentofacial Orthop 1997;112:1-7. [ Links ]
 Correspondence:
Correspondence:
André Wilson Machado
R. Eduardo José dos Santos, 147, salas 810/811
Salvador, BA – Brazil
41940-455
E-mail: andre@andrewmachado.com.br
Received: November 4, 2009
Accepted: April 9, 2010
Conflict of Interest Statement: The authors state that there are no financial and personal conflicts of interest that could have inappropriately influenced their work.













