Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.1 Porto Alegre Jan./Mar. 2012
ORIGINAL / ORIGINAL
Transverse measurements of the jaws of patients with a predominance of nose and mouth breathing in children between 6 and 14 years of age
Medidas transversais dos maxilares de pacientes com predominância de respiração nasal e bucal em crianças de 6 a 14 anosI
José Márcio Lenzi de OLIVEIRA II; Erica Silva CARVALHO II; André Luiz Tannus DUTRA III; Ana Cristina Barreto BEZERRA IV; Orlando Ayrton de TOLEDO IV
I Artigo elaborado a partir da tese de JML OLIVEIRA, intitulada "Medidas transversais maxilares e de componentes orgânicos da saliva em pacientes com predominância de respiração bucal e nasal na faixa etária de 6 a 14 anos". Universidade de Brasília; 2011
II Universidade Paulista - Brasília, Faculdade de Odontologia. Setor Gráfico Asa Sul, quadra 913, s/n., Conjunto B, 70390-130, Brasília, DF, Brasil
III Universidade do Estado do Amazonas. Manaus, AM, Brasil
IV Universidade de Brasília, Faculdade de Odontologia. Brasília, DF, Brasil
ABSTRACT
Objective
To determine and study the occurrence of possible growth and development anomalies of the craniofacial complex in patients aged between 6 and 14, diagnosed with predominantly mouth and nose breathing patterns, and without having received prior dental treatment.
Methods
We performed transverse jaw measurements on 103 patients between 6 and 14 years of age, registered for orthodontic treatment in the Military Hospital in the Brasilia area. Divided into two groups: Group 1, patients with predominance of nose breathing and Group 2, patients with predominance of mouth breathing.
Results
There were no statistically significant differences between the upper and lower intercanine or upper intermolar distances, between groups 1 and 2. A smaller statistically significant difference was observed in group 2 when evaluating the lower intermolar distance.
Conclusion
The group of mouth breathers showed statistically lower values in the lower jaw, thus suggesting a contraction in the posterior arch of patients diagnosed with this breathing pattern.
Indexing terms: Child. Dental arch. Mouth breathing.
RESUMO
Objetivo
Verificar e estudar a ocorrência de possíveis anomalias de crescimento e desenvolvimento do complexo craniofacial, de pacientes diagnosticados com o padrão de respiração predominante bucal e nasal, na faixa etária de 6 a 14 anos de idade, sem tratamento ortodôntico prévio.
Métodos
Foram realizadas as medidas transversais maxilares em 103 pacientes na faixa etária dos 6 a 14 anos de idade, inscritos para tratamento ortodôntico no Hospital Militar de Área de Brasília. Divididos em dois grupos: 1 pacientes com predominância de respiração nasal e 2 pacientes com predominância de respiração bucal.
Resultados
Não foram observadas diferenças estatisticamente significativas entre as distâncias inter-caninos superior e inferior, inter-molares superior, entre os grupos 1 e 2. Foi observada diferença estatisticamente significativa menor no grupo 2 quando avaliada a distância inter-molar inferior.
Conclusão
O grupo de pacientes respiradores bucais apresentou valores estatisticamente menores na arcada inferior, sugerindo desta forma uma contração posterior na arcada dos pacientes diagnosticados com este padrão de respiração.
Termos de indexação: Criança. Arcada dental. Respiração bucal.
INTRODUCTION
The act of breathing exerts a heavy influence on the stomatognathic system. When discussing respiratory function and its effects on the growth of the craniofacial complex, one of the main issues is the distinction between mouth and nose breathing. It should be stressed that there are various levels of combinations of respiratory capacity. Accordingly, the majority of patients may be considered to be mouth/nose breathers at diverse levels, and just a minority of them should be considered as purely mouth breathers1-2.
Where breathing occurs only by mouth, the stimulation of facial growth and development through the action of the musculature may occur unsatisfactorily. This happens mainly when the child is experiencing periods of growth spurts as this favors the disharmonious growth and development of the facial structure3.
This disharmony in growth and development is normally caused by problems with general health, the relationship of the organic structures, relationship with the dentofacial morphology or by environmental influences. Obstructive diseases of the upper airways come under general health problems and environmental influences4.
As far as breathing through the mouth is concerned, there is little activity by the respiratory muscles and the nerve terminations of the nasal cavities are not called into action. Air gets to the lungs via a mechanically shorter and easier path, with the occurrence of atrophy of nasal cavity development, which has an effect on the development of the upper jaw, causing atresia5-6.
In addition, the mouth breather may present various signs and symptoms such as: predominantly vertical craniofacial growth, increased angle of the jaw, long face, ogival or inclined palate, narrow facial dimensions, hypo-development of the upper jawbones, narrow or inclined nostrils, microrhinia with a smaller space in the nasal cavity, deviated septum, class II malocclusion, increased overjet, crossbite or open bite, protrusion of the upper incisors3,7.
As for nose breathing, this has an impact on the performance of the functions of sucking, chewing, swallowing and speaking, and is of fundamental importance to the development of the craniofacial complex. The ion-charged air, as it forces a passageway through the nasal cavities, stimulates the medial and lateral surfaces of each nostril and causes the airy spaces in the bones to grow. Specific responses are generated such as: the three dimensional development of the nasal cavities and the size of the paranasal or pneumatic cavities5-6.
The human body exhibits variations in the speed of growth due to the diversity of organ morphology, however it is an orderly process which possesses moments of greater intensity. These are divided into three big growth spurts in the craniofacial complex. The first happens on average at three years of age and it is here that the principal increases in antero-posterior growth of the upper and lower jaws occur8.
In the stage that precedes the eruption of the incisors, at around five years of age, the second growth spurt occurs, this one assuming greater proportions in terms of upper and lower jaw laterality. This process is extremely important for compensation to occur between the size of the bone base and the teeth8-9.
Craniofacial growth occurs through alternating processes of bone apposition and reabsorption, in which the nasal and orbital floors and the palate move downwards in parallel. The segments of the mouth move outwards and downwards, while the upper jaws move downwards and forwards. Accordingly, the upper dental arch grows wider naturally. The growth in width is mainly represented by the activity in the median palatine suture10.
The parameters of this transverse growth of the upper jaw may be obtained via intercanine and intermolar measurement. The intercanine distance is the measurement between the lingual surface of the canines at the level of the cervical region or from cuspid to cuspid. This space increases gradually in the mandibular arch as a result of the distal movement of the deciduous canines, occupying the primate spaces. This growth is on average 1.12 mm between the ages of 5 and 18, measured cervically from the lingual surface, increasing to 2.45 mm when measured from cuspid to cuspid. In the maxillary arch, this increase is a little higher and may be 1.76 mm in maxillary intercanine distance when measured cervically and 4.39 mm when measured from cuspid to cuspid10.
The third and biggest growth spurt occurs during puberty, in which the greatest increases in speed are observed, particularly in the antero-posterior direction of the upper and lower jaw8-9.
The study of these growth spurts and the development of the craniofacial complex has increasingly caught the attention of professionals working on the treatment of young people in the phases of prepuberty and puberty. A number of aspects, such as mouth/nose breathing or simply mouth breathing in this phase still produce some controversy and confusion as regards the influence of these factors on tendencies for facial growth and development in patients. Despite this discussion, there are authors who have already established associations between growth anomalies and the development of the upper jaw in mouth breathers, quoting the atresia of the upper dental arch and certain malocclusions as frequent features of the mouth breather5.
Amongst the manifold causes of malocclusion, mouth breathing is ostensibly the most potent, persistent and varied in results, causing asymmetrical development of the muscles, the bones of the nose and the upper and lower jaws. The instability in functions exerted by the lips, cheeks and tongue is supposedly a frequent feature of this dysfunction. It was found that the effects of mouth breathing always manifested themselves in the facial features: noses are small, short, with lack of nostril development, cheeks are pale and sunken, mouth constantly open with a short upper lip. Moreover, it was found that the lower jaw appeared retruded and underdeveloped, being shorter probably due to the unstable pressure of the musculature, and being predominantly related to class II, division 1 malocclusion4,11.
The action of the musculature, both inside and outside of the mouth, is considered to be an abnormal phenomenon during mouth breathing. The upper teeth are deprived of support from the tongue on the palatine surface, allowing the mouth musculature to operate on the outside, causing a contraction of the dental arch and the palate. This effect is particularly noticeable during the mixed dentition stage.
Despite the fact that many professionals associate mouth breathing as being the result of nasal obstruction, leading to a long face syndrome with dentofacial anomalies, there is nothing in the literature which bears out this assertion. There is in fact a complex interaction between hereditariness and environmental factors which interfere with the genetic pattern of predetermined growth12.
Other professionals share the hypothesis that, if nose breathing is aggravated for any reason, a compensating mechanism of the whole facial structure would kick in. This would result in defined morphological alterations to the middle and lower regions of the face, though not sufficient to modify the predetermined genetic factors of each individual11,13.
Mouth breathers cannot be considered as suffering from one specific type of malocclusion. However, the discovery of a smaller intermolar distance in mouth breathers could suggest a tendency for the evolution of contraction of the maxillary arch and the subsequent introduction of posterior crossbite14.
Analysis of the intermolar distance amongst individuals in two distinct groups, the former involving predominantly mouth breathers and the latter predominantly nose breathers, showed that, in terms of the dimensions of the palate, there is a smaller statistically significant distance in mouth breathers. As for the intercanine distances, however, there was no significant difference between the groups. These findings suggest a tendency towards maxillary narrowing in a more posterior position as a result of the altered breathing pattern14.
As regards associations between facial types (dolichofacial, mesofacial and brachyfacial) and breathing patterns (mouth and nose) a correlation was found between the brachyfacial type and the nose breathing pattern. In associations between breathing patterns (mouth and nose) and cephalometric variables, the variable of facial depth was found to be significant15.
Obstruction of the upper airways due to hypertrophy of the adenoids, palatine tonsils or both (environmental factors) may result in serious cardiorespiratory complications. However, the prejudicial effect of adenoid growth on craniofacial growth is unclear. Nevertheless, patients suffering from persistent nose obstruction, the presence of infection or allergy and adenoid hypertrophy, should have them removed5,16.
Mouth breathers present with greater vertical displacement of the lower jaw than nose breathers and nasal obstruction produces changes in masticatory muscle activity as well as modification in lingual pressure and position. The lower jaw exhibits a posterior and rotational displacement in an attempt to maintain the intake of air as compensation for the nasal obstruction, when in a seated position17.
Processes of allergic rhinitis promote edema and cause obstruction of the Eustachian tube, giving a blocked ear sensation. During the day, the Eustachian tube remains open as a result of chewing, swallowing and yawning. However, at nighttime, only the swallowing of saliva keeps the tube open. The dryness of saliva presented by mouth breathers does not allow this to take place and patients begin to grind their teeth in an attempt to keep the Eustachian tube open and in many situations, they develop the habit of bruxism18.
In view of the findings related above, the aim of this study was to check and study the occurrence of possible anomalies with the growth and development of the craniofacial complex in patients, in the 6 to 14 age range, diagnosed with a breathing pattern which is predominantly oral or predominantly nasal.
METHODS
This study was previously evaluated and approved by the Ethics in Research Committee at the Military Hospital (HFA), under reference number 005/2007 CEP/ HFA.
A total of 310 individuals, awaiting dental treatment, were referred for the initial examination. Internal and external clinical examination of the mouth was performed using specific clinical instruments, in the preventive dentistry consulting rooms at the Military Hospital in Brasília (HMAB), between April and June 2010.
After clinical examination, a record card was completed containing information supplied by the parents/guardians. The data on the record card identified behaviors, signs and signals that might give clues as to the predominant breathing mode. The first item, tonsillitis and/or sinusitis, was specific as to the individual's general health, with the aim of analyzing breathing mode, whether predominantly via mouth or otherwise, and the probable etiology. Questions were put as to sleep, snoring, nighttime drooling, difficulty in breathing through the nose or dry mouth on waking up, all signals of partial or total nasal obstruction for part or all of the day.
Of the total of 310 individuals awaiting treatment for malocclusions in the Military Hospital in Brasilia, 220 of them, irrespective of race or gender, were considered to be suitable for participation in the study, since they came back with the consent of the parents/guardians, along with the free and informed consent form, as well as complying with the following criteria: a) sufferers of Angle's class I, II or III malocclusion; b) children in the mixed/permanent stage of dentition; c) absence of dental caries lesions; d) absence of dental anomalies of shape, number, structure or eruption; e) no premature tooth loss; f) absence of prior dental treatment; g) absence of non-nutritive sucking habits.
Of the total number of participants in the study, 60 were diagnosed as predominantly mouth breathing and 160 predominantly nose breathing. The initial diagnosis was carried out by the project‘s author, through the use of the protocol extolled by Willer et al.19. The patients were observed on different days using instructional films to evaluate the characteristics compatible with breathing pattern. In stage two, the diagnosis was confirmed in multidisciplinary fashion by the professional staff at the Military Hospital in Brasilia (speech therapists and ear, nose and throat specialists).
Of the 220 preselected subjects, 103 showed up for the examination on the appointed day and, accordingly, formed the sample for the study, in 2 groups, group I comprising 59 children with Angle's class I, II or III malocclusion and predominantly nose breathers, while group II consisted of 44 children who were predominantly mouth breathers.
Producing the plaster models
Using plastic casting trays (Morelli®, Campinas, Brazil), alginate molds were obtained (fast-setting Geltrate®, São Paulo, Brazil) of the dental arches of each child selected for the study, with subsequent plaster pouring (type II model plaster). These plaster replicas were duly numbered, thereby facilitating control and permitting better evaluation of results.
The modeling was carried out in the hospital itself, in the dental consulting room, and always by the author of this study; the children remained seated with the chair back inclined at 90º. The children were instructed to clench normally in maximum intercuspidation so that records of the occlusion in wax could be obtained. All the plaster models were prepared in the Hospital's prosthetics laboratory immediately after molding with the aim of preventing distortions in the material. Only the final finishing was carried out in a specialized laboratory and the models received no form of special treatment prior to analysis.
With the aim of getting the maximum cooperation out of the children and lessen their initial anxiety, as well as to facilitate the explanation about the procedure being performed, the examinations and moldings were always carried out in the presence of the parents/guardians.
Evaluation of results
Intercanine and intermolar measurements were obtained by the same researcher using a millimeter ruler and a pair of compasses at both arches of the study models. As a benchmark, the incisal ridges of the canine teeth and mesio-palatine cuspid of the first permanent molars were used. The objective was to check the growth and development of children who were predominantly mouth breathers and predominantly nose breathers.
The results were compared with the aim of checking and correlating the growth and development pattern of the craniofacial complex of predominantly mouth breathers and predominantly nose breathers.
RESULTS
The statistical analysis of the data was performed using the statistical software application Statistical Package for Social Science - SPSS 17.0. The variable predominantly mouth or predominantly nose breathing was cross-checked against the other variables in order to find significant discrepancies between the means of the two groups. The normality test for the variables was not carried out as the sample contained over thirty subjects. The student's t test was chosen as the variables were continuous. The significance level of the tests was considered to be 5%. On performing the t test, in relation to each variable studied, in the patient groups that were predominantly nose breathing or predominantly mouth breathing, the assumed null hypothesis was that the means were equal and as an alternative hypothesis, that the means were different.
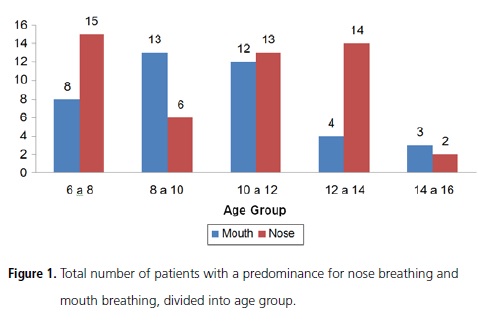
In the sample studied, 27.2% of patients were predominantly mouth breathing (Figure 1).
Intercanine and intermolar distances
In the analysis of the means of the upper and lower intercanine/intermolar transverse measurements, the only measurement which resulted in a mean with a significant difference was the lower intermolar distance.
Looking at the measurement for the upper intercanine distance, a mean value of 31.25 mm was found for the group of mouth breathers and 32.07 mm for the nose breathers (Table 1).
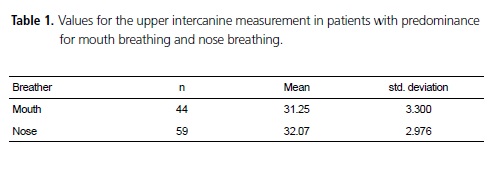
When performing the t test, the calculated value of t was below the tabulated value. It may be concluded that there is no significant difference between the means in the two groups.
Analyzing the measurement of the upper intermolar distance, a mean value of 36.89mm was found for the group of mouth breathers and 37.93mm for the nose breathers (Table 2).
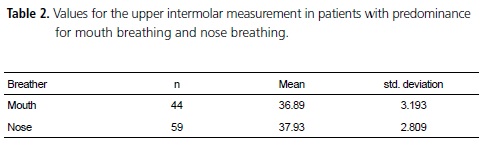
When applying the t test, the calculated value of t was below the tabulated value. It may be concluded that there is no significant difference between the means in the two groups.
As for the measurement of the lower intercanine distance, a mean value of 25.95 mm was found for the group of mouth breathers and 25.75 mm for the nose breathers (Table 3).
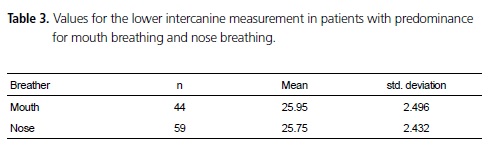
When applying the t test, the calculated value of t was below the tabulated value. It may be concluded that there is no significant difference between the means in the two groups.
Looking at the measurement for the lower intermolar distance, a mean value of 32.8 mm was found for the group of mouth breathers and 34.32 mm for the nose breathers (Table 4).
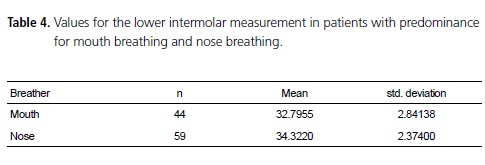
On performing the t test, the calculated value of t was above the tabulated value. It may be concluded that there is a significant difference between the means in the two groups, i.e. in the group of patients that is predominantly nose breathing, the mean is higher.
When cross-referencing the variables of male gender amongst the groups that are predominantly mouth breathing or nose breathing and the female gender amongst the groups that are predominantly mouth breathing or nose breathing, there was no statistically significant difference. On carrying out the t test, the calculated value of t was below the tabulated value. It may be concluded that there is no significant difference between means in the two groups.
DISCUSSION
In this study, the technique chosen for checking the transverse measurements was that of the dental plaster molds, as this is the most simple technique for obtaining upper and lower jaw measurements, demonstrating results similar to those of the photocopying and digitized image technique20. The incisal edges of the lower and upper canine teeth and the mesio palatine cuspids of the primary permanent molars, served as a benchmark for the measuring.
Despite what has been discussed previously, one study carried out with the aim of evaluating transverse measurements in study models returned greater accuracy with the digitizing technique than the others when accurate measurements are required21.
As a result of this study, in spite of the differences found in the upper arch, with the intercanine distance being greater for the group with the nose breathing pattern, this was not statistically significant. As for the lower arch, a greater intercanine distance was observed in the group of patients that was predominantly mouth breathing, though this was not statistically significant.
These findings agree with a study which found no statistically significant differences between the intercanine distance in groups of allergic and nonallergic patients and in groups of nose breathing and mouth breathing children. This would tend to suggest that the breathing mode cannot be linked to the narrowing of the anterior region of the upper jaw14.
In another analysis, a correlation was established between the intercanine and interalar distance, showing evidence of an association between this relationship and another variable, the shape of the arch. This correlation was statistically significant in the cases of square and oval arches22.
Contrary to the intercanine distances, statistically significant differences were demonstrated in respect of the intermolar width in the different breathing pattern groups14. The results found in the present study were comparable with the aforementioned research inasmuch as statistically less significant differences were observed with the intermolar distances of the lower arch in the group of patients showing a predominance for mouth breathing. It was found in this study that the lowest intermolar differences in the upper arch were found in the group of predominantly mouth breathers, however the values found are not statistically relevant. One explanation for the differences in intermolar distance found between the two groups, involves the lack of ventilation in the nasal area which causes the reduction in the transverse development of the upper jaw, indicating a tendency for greater narrowing of the posterior region of the upper jaw, as a result of the breathing pattern14.
This narrowing of the upper arch in mouth breathers suggests a deeper palate in these patients14. The literature is almost unanimous in asserting that patients with obstructive problems present with deeper palates. This finding agrees to that found in the present study.
It was determined that the width of the dental arches in males is greater when compared with females, and that for both sexes, when the mandibular plane angle and anterior base of the skull get bigger, the width of the arch tends to diminish23. It is important to emphasize that the increase in the angle of the mandibular plane is one of the most commonly found cephalometric findings in mouth breathing patients15.
In this study, it was found that the intercanine and intermolar distances of the upper and lower arches in male patients who have a predominance for breathing via the mouth or nose, do not exhibit statistically significant differences. However, when we compare the same distances in the female sex, higher values are found in the predominantly nose breathing group, however they were not considered to be statistically significant. When analyzing the male and female sexes, regardless of breathing pattern, these findings corroborate the findings of the aforementioned author, who reported higher values in the male sex.
One survey found there to be a prevalence of mouth breathing of 5.5%. This low index could be related to both the genetic component and climatic issues, since the individuals in the sample came from a region where there was a low prevalence of respiratory diseases24.
Unlike the values reported previously, this survey was carried out in a region with sharp climatic changes inasmuch as a daily thermal range was found with values in excess of 10ºc and relative humidity values below 50%, thereby multiplying the potential for allergenic components. This could be one of the reasons why the prevalence of mouth breathers found in this study was 27.2%, different from that previously quoted, but in conformity with the others already mentioned. This big variance in values relating to the prevalence of mouth breathers in the literature is not just a result of environmental factors, but also relates to the standardization of the samples and principally the difference in terms of the methodology employed for diagnosing the breathing patterns of the populations involved.
Breathing pattern has a strong effect on the stomatognathic system. The diagnosis of respiratory function and its effect on the growth of the craniofacial complex, as well as the distinction between mouth and nose breathing, amount to being important and difficult issues faced every day in the clinic. The classification of individuals into mouth or nose breathers is too simplistic and disguises the existence of a graded scale between totally mouth breathing and totally nose breathing. The majority of individuals probably lie in between these two extremes. One of the limitations of such evaluations is the selection of the sample based on criteria that are more visual than functional, usually based on clinical judgments made by one sole professional25.
This study used the methodology extolled by Willer et al.19 in which the diagnosis protocol for the predominant breathing patterns requires a multidisciplinary formation of professionals from the areas of otolaryngology, speech-language pathology and dentistry, with the aim of reducing the possibility of erroneous diagnosis.
There are many different levels of combinations of nasal and oral respiratory capacity. Thus the majority of patients may be regarded as both mouth and nose breathers at various levels, with only a small minority being diagnosed specifically as mouth breathers1-2.
It is important to stress that the quantification of breathing and its consequences for the craniofacial complex, still lack precision, and the overlapping of various diagnostic methods is still the most effective way for the problem to be identified19.
When the breathing takes place through the nasal airway, it provides favorable conditions for the growth and development of hard and soft tissue2.
In mouth breathers, the vertical displacement of the lower jaw is greater than in nose breathers and nasal obstruction produces alterations in masticatory muscle activity as well as the modification in tongue pressure and position17.
The stimulation of facial growth and development through the action of the musculature could take place inappropriately in the case of mouth breathing, primarily when the child is experiencing periods of growth spurts, since this would promote disharmonious growth and development of the facial structure3.
CONCLUSION
In the group studied, there was a prevalence of 27.2% of patients with a predominance for mouth breathing. No statistically significant differences were found, when comparing males and females, between the groups with a predominance for mouth breathing or for nose breathing.
The group of patients with a breathing pattern that is predominantly by mouth, exhibited lower statistically significance in terms of intermolar distances in the lower arch, when compared to the group of patients with a predominance for nose breathing. Despite the fact that lower values were observed for transverse distances in the group of predominantly mouth breathing patients, this condition cannot be considered in its own right as a determining factor in the narrowing of the dental arches.
Collaborators
JML OLIVEIRA was responsible for patient evaluation, data collection and composition of the article. ES CARVALHO was responsible for the conception of the project structure, bibliographical survey and composition ALT DUTRA was responsible for the conception of the project structure, bibliographical survey, grammatical review and composition of the article. ACB BEZERRA was responsible for the conception of project structure, bibliographical survey, the English language revision and composition of the article. AO TOLEDO provided guidance on the methodology and took part in the statistical analysis, tabulation of results and composition of the article.
REFERENCES
1. Linder AS. Respiratory function in telaton to facial morphology and dentition. Brit J Orthod. 1979.6(2):59-71. [ Links ]
2. Felício CM. Fonoaudiologia aplicada a casos odontológicos. São Paulo: Pancast; 1999.
3. Almeida FL, Silva AM, Serpa EO. Relação entre má oclusão e hábitos em respiradores orais. Rev CEFAC. 2009;11(1):86-93.
4. Hennig TR, Silva AM, Busanello AR, Almeida FL, Berwig LC, Boton LM. Deglutição de respiradores orais e nasais: avaliação clínica fonoaudiológica e eletromiográfica. Rev CEFAC. 2009;11(4):618- 23.
5. Castilho JCM, Generoso R, Moraes LC, Moraes MEL. Avaliação radiográfica da altura facial anterior inferior (AFAI) em pacientes com e sem obstrução da nasofaringe. J Bras Ortodon Ortop Facial. 2002;7(38):133-41.
6. Carvalho GD. Respirador bucal: uma visão funcional e clínica da amamentação. Curitiba: Editora Lovise; 2003.
7. Sabatoski CV, Maruo H, Camargo ES, Oliveira JHG. Estudo comparativo de dimensões craniofaciais verticais e horizontais entre crianças respiradoras bucais e nasais. J Bras Ortodon Ortop Facial. 2002;7(39):246-57.
8. Ferreira FV. Ortodontia: diagnóstico e planejamento clínico. 3ª ed. São Paulo: Artes Médicas; 1999.
9. Enlow DH, Hans MG. Noções básicas sobre crescimento facial. São Paulo: Editora Santos; 1998.
10. Araújo MGM. Ortodontia para clínicos. 4ª ed. São Paulo: Editora Santos; 1999.
11. Harvold EP, Tomer BS, Vargervik K. Primate experiments on oral respiration. Am J Orthod. 1981;79(4):359-72.
12. O'Ryan FS, Gallagher DM, LaBanc JP, Epker BN. The relationship between nasorespiratory function and dentofacial morphology. Am J Orthod. 1982;82(5):403-10.
13. Hartgerink DV, Vig PS. Lower anterior face height and lip incompetence do not predict nasal airway obstruction. Angle Orthod. 1989;59(1):17-23.
14. Feres MFN, Enoki C, Sobreira CR, Matsumoto MAN. Dimensões do palato e características oclusais de crianças respiradoras nasais e bucais. Pesq Bras Odontoped Clin Integ. 2009;9(1):25-9.
15. Gouveia SAS, Nahás ACR, Ferreira FAC. Estudo cefalométrico das alterações dos terços médio e inferior da face em pacientes com diferentes padrões respiratórios e faciais. Rev Dent Press Ortodon Ortop Facial. 2009;14(4):92-100.
16. Shimizu IA, Shimizu RH, Souza RS. Estudo morfofuncional do lábio superior de indivíduos respiradores bucais portadores de má-oclusão de classe I. J Bras Ortodon Ortop Facial. 2004;52(9):364-77.
17. Shikata N, Ueda HM, Kato M, Tabe H, Nagaoka K, Nakashima Y, et al. Association between nasal respiratory obstruction and vertical mandibular position. J Oral Rehabil. 2004;31(10):957- 62.
18. Almeida PDV, Bezerra JG, Kreai TB, Barbosa JL, Tanaka O. Estudo das proporções transversais e verticais da face de acordo com modo respiratório. J Bras. Ortodon Ortop Facial. 2006;11(62):206-16.
19. Wieler WJ, Barros AM, Barros LA, Camargo ES, Ignácio AS, Maruo H, et al. A combined protocol to aid diagnosis of breathing mode. Arch Oral Res. 2007;3(2):101-14.
20. Rosseto MC, Palma FM, Ferreira RI, Pinzan A, Vellini-Ferreira F. Comparative study of dental arch width in plaster models, photocopies and digitized images. Braz Oral Res. 2009;23(2):190-5.
21. Paulino V, Paredes V, Gandia JL, Cibrian R. Prediction of arch length based on intercanine width. Eur J Orthod. 2008;30(3):295-98.
22. Rai R. Correlation of nasal width to inter-canine distance in various arch forms. J Indian Prosthodont Soc. 2010;10(2):123- 7.
23. Forster MC, Sunga E, Chung C. Relationship between dental arch width and vertical facial morphology in untreated adults. Eur J Orthod. 2008;30(3):288-94.
24. Berwig LC, Silva AMT. Análise quantitativa do palato duro de respiradores orais: revisão de literatura. Rev Soc Bras Fonoaudiol. 2011;16(4):483-7.
25. Saga A, Maruo H, Tanaka O, Souza PHC. Estudo comparativo da morfologia craniofacial entre respiradores predominante nasais e bucais na maloclusão classe II, divisão 1 de Angle. J Bras Ortodon Facial. 2004;9(54):595-611.
 Correspondence to:
Correspondence to:
JML OLIVEIRA
e-mail: marcio.lenzi@planalto.gov.br
Received on: 29/4/2011
Approved on: 2/8/2011













