Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.1 Porto Alegre Jan./Mar. 2012
ORIGINAL / ORIGINAL
Retrospective four year analysis in 199 bone grafts of the alveolar ridge
Análise retrospectiva de quatro anos em 199 enxertos autógenos do rebordo alveolar
Rafael ORTEGA-LOPES I; Valdir Cabral ANDRADE I; Cláudio Ferreira NÓIA I; Castelo Pedro Vemba CIDADE I; Henrique Duque de Miranda CHAVES NETTO I; Renato MAZZONETTO I
I Universidade Estadual de Campinas, Faculdade de Odontologia, Serviço de Cirurgia e Traumatologia Buco-Maxilo-Faciais. Av. Limeira, 901, Caixa postal 52, 13414-018, Piracicaba, SP, Brasil
ABSTRACT
Objective
To evaluate the factors that lead to complications in autogenous bone grafting.
Methods
Review of clinical records of the patients that were candidates for rehabilitation, between May 2004 and December 2008. With regard to the donor area, of the 199 reconstructions, 175 were autogenous bone graft procedures and 210 donor areas were acted upon.
Results
A total of 48 procedures (24.12%) were grafts using particulate bone while sinus lift grafts were performed on 28 patients (14.07%). Osteogenesis distraction and inferior alveolar nerve lateralization were performed in five (2.51%) and three (1.51%) procedures respectively. Eleven autogenous bone grafts were lost, of which 90.9% were onlay block.
Conclusion
The use of autogenous bone grafting in atrophic alveolar ridge reconstruction is a highly successful treatment, and the sinus lift procedure is the most predictable form of treatment.
Indexing terms: Bone transplantation. Dental implant. Postoperative complications.
RESUMO
Objetivo
Avaliar os fatores que levam às complicações em enxertia óssea autógena.
Métodos
A amostra foi composta pela revisão de prontuários clínicos de pacientes candidatos à reabilitação no período entre maio de 2004 e dezembro de 2008. Em relação à área doadora, das 199 reconstruções, 175 foram procedimentos de enxerto de osso autógeno, sendo abordadas 210 áreas doadoras.
Resultados
Os enxertos com osso particulado totalizaram 48 procedimentos (24,12%). O levantamento de seio maxilar foi realizado em 28 pacientes (14,07%). Já a distração osteogênica e lateralização do nervo alveolar inferior foi realizada em cinco (2,51%) e três (1,51%) procedimentos respectivamente. Foi registrada a falha de 11 enxertos com osso autógeno. Dos enxertos perdidos, 90,9% deles foram os de bloco tipo onlay.
Conclusão
A utilização de enxertos ósseos autógenos nas reconstruções de rebordos alveolares que apresentam atrofia é um tratamento com alto índice de sucesso, destacando-se a cirurgia de levantamento de soalho de seio maxilar como a modalidade mais previsível de reconstrução óssea.
Termos de indexação: Transplante ósseo. Implante dentário. Complicações pós-operatórias.
INTRODUCTION
At the present time, dentistry has at its disposal a variety of techniques for treating atrophic alveolar ridges that are unable to take implants. Amongst the most common reconstructive procedures are bone grafts, which are recommended for horizontal and/or vertical defects of the alveolar ridge, either in block form or in particulate form1-4.
In addition to enabling bone volume augmentation, grafts make it feasible to place the implant, at a subsequent point in time, in the ideal, three dimensional location, enabling the future prosthetic load to be inserted along its own axis, thereby providing longevity for the proposed rehabilitation. To this end, the autogenous graft has, up to now, been regarded as the "gold standard" in these types of rehabilitation as it presents specific properties such as osteogenesis, even with the disadvantage of the need of a donor area to achieve it.
There are certain factors, however, that may compromise the success of bone grafts. These include: systemic diseases, tobacco usage, patients who use substances noxious to health (alcohol, drugs), the inexperience of the surgeon, lack of postoperative care by the patients, to name but a few5-7.
The objective of this study is to evaluate the factors that lead to complications with autogenous bone grafts, through a sample of patients treated at the Advanced Training School of the Association of Dental Surgeons of Campinas (ACDC - Campinas), over a period of 4 years.
METHODS
For the data collection and the preparation of the study, the clinical records were examined of patients who were candidates for dental rehabilitation through the insertion of osseo-integrated dental implants, between May 2004 and December 2008, through the Advanced Surgery Training Course at the ACDC in Campinas, in the state of Sao Paulo.
The collection of data, related to the procedures carried out, was based on clinical prognoses in which, for each patient appointment or return visit, the professional in charge made notes on the patient's record, describing the types of treatment performed and the prognosis of the patient as a result of treatment, the patients being monitored for an average period of 12 months. Thus it was possible to obtain the modes of treatment to which the patient was subjected and the intra-operative and post-operative outcomes, such as accidents, complications, action taken to resolve these intercurrences, the success, or lack thereoft, of the treatment employed. A total of 186 patients were selected who underwent some form of reconstructive procedure with autogenous bone. Data were collected in respect of the surgical technique used, the donor area and potential complications.
Excluded from the sample were clinical records with insufficient data or data not properly completed, which gave rise to doubts over the details of the surgical procedure carried out or the clinical prognosis of the patient in question. This study was conducted after approval by the Ethics in Research Committee at the Faculty of Dentistry at the Campinas State University (UNICAMP), filed as case no. CEP 078/2008, and it observes the ethical principles contained in the Helsinki declaration (2000).
Data collection was carried out concurrently by two examiners with each medical record having its data analyzed and interpreted simultaneously by both.
RESULTS
Out of the 199 reconstructive procedures performed, 171 took place at the surgical stage preceding the insertion of the dental implant (pre-treatment), 23 during the insertion of the implants and 5 after the loss of implants.
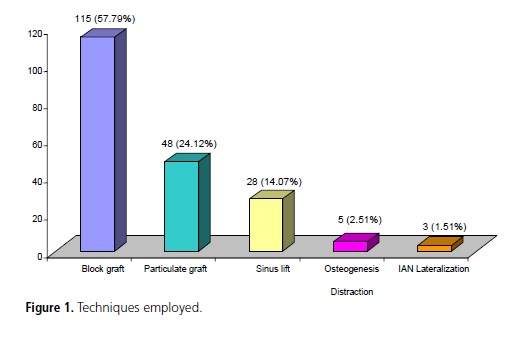
The distribution of reconstructive procedures performed was classified according to the technique employed. The onlay block graft was the procedure most frequently employed, in 115 procedures (57.79%) with autogenous bone where three of these cases were mixed with 0.5 cc of heterogeneous bone (demineralized bone graft of bovine origin - Genox Org®, Baumer, Mogi Mirim, Brazil). In total, there were 48 grafting procedures (24.12%) using particulate bone, of which 36 cases used only autogenous bone, twelve cases were joined with 0.2 cc of heterogeneous bone (demineralized bone graft of bovine origin - Genox Org®, Baumer, Mogi Mirim, Brazil). Maxillary sinus lifts were performed on 28 patients (14.07%) with autogenous bone and in one case it was joined with 0.2 cc of heterogeneous bone (demineralized bone graft of bovine origin - Genox Org®, Baumer, Mogi Mirim, Brazil). As for osteogenesis distraction and lateralization of the inferior alveolar nerve, this was performed in 5 (2.51%) and 3 (1.51%) procedures respectively, without the need for any type of bone graft (Figure 1).
As regards the donor area for the acquisition of autogenous graft, for the 199 reconstructions, 210 donor areas were acted upon. The mandibular symphisis region was used in 70 cases (33.33%); maxillary tuberosity in 54 cases and 8 bilateral cases making a total of 62 (29.52%). As for the mandibular branch, this was applied in 67 cases plus 4 bilateral cases, totaling 71 (33.81%), while the iliac crest was used in 6 cases (2.86%) and the tibia in 1 case (0.48%). No cases of the use of calvaria were recorded (Figure 2).
As regards complications arising from treatment, 10 procedures presented complications such as dehiscence of the gingival tissue, graft exposure, exposure of graft fixation material (mesh and titanium screws) and infections in the receptor region.
The failure of 11 (5.53%) grafts with autogenous bone was recorded out of a total of 199 patients over the course of the 12-month tracking period. Of those grafts lost, 90.9% were of the onlay block type and only one was a maxillary sinus lift. No risk factors such as tobacco usage or other systemic alterations were found in any of the patients who lost grafts.

DISCUSSION
For the insertion of osseo-integrated implants, it is necessary for there to be bone tissue in sufficient quantity and quality, since this will be the main factor in the support and survival of this type of rehabilitation. The lack of volume in the height and thickness of the alveolar ridge could adversely affect the correct insertion of the implant1. Without the necessary augmentation in the alveolar ridge, the esthetic outcome could be adversely impacted, as well as the position of the implant in relation to the prosthetic to be installed8.
Clinical findings have shown a reduced implant success rate when the maxillary bone is inadequate in terms of both volume and density. However, rehabilitation using inlay and onlay bone grafting techniques promotes an implant survival rate close to those obtained in nonreconstructed jawbones7.
As far as the origin of the graft is concerned, different maxillary reconstruction options are available for use such as autogenous bone, homogeneous bone and alloplastic materials for subsequent placement of implants, however, despite the fact that it still generates controversy and discussion, it is accepted that the best results are obtained using autogenous bone9. In the present study, the success rate percentage was 94.48%, which is roughly similar to the results found in the literature4,10-11. In a study with 129 grafts using autogenous bone, the authors reported a success rate of 96.9%, concluding that this mode of grafting in pre-dental implant therapy has a high degree of predictability11.
Misch & Misch.12, Buyukkurt et al.13 and Dik et al.14 demonstrated the aspects to be observed in relation to the autogenous bone graft from the mandibular symphisis area, concluding that this technique offers advantages in the repair of severe alveolar defects prior to implant insertion surgery, easy access to the donor area, an increase in the quantity of donor bone when compared with other intraoral areas and improved bone density in the receptor region, and is thus regarded as a viable alternative for reconstructing alveolar ridges and inserting implants. Andersson15, however, states that, despite the viability of using mandibular symphisis in alveolar reconstructions, the mandibular branch should be considered as the first option of choice, as this offers a lower potential for paresthesia, and consequently better acceptance on the part of the patients. In this study, the percentages of use of mandibular branch and mandibular symphisis are very similar (33.81% and 33.33%, respectively).
A number of factors may affect the success of these grafts leading to loss, such as systemic diseases, patients who smoke, patients who use substances noxious to health (alcohol, drugs), inexperience of the surgeon and lack of post-surgical care5-7. These are the main indicators of failure in this type of surgery16-17, however it should be stressed that in our study there was a graft failure rate of 5.53% but, notwithstanding this, none of these patients presented adverse health conditions or any relevant medical fact; they were all classified as healthy.
The success of bone grafting treatments is related to the predictability of procedures based on the chronology and on the cellular mechanisms involved in the physiopathology of bone repair10. Complications in these treatments usually appear in the first few months after the bone graft or present bone reabsorption after the insertion of the implant, not managing to gain adequate grip on the bone for prosthetic rehabilitation11. This could be the reason why reconstructive procedures do not have a significant impact on late loss of dental implants. In the present study, the most common complications were dehiscence of the gingival tissue, graft exposure, exposure of graft fixation material (mesh and titanium screws) and infections in the receptor region, and all of these complications occurred before insertion of the dental implants.
CONCLUSION
According to the results of this retrospective analysis and based on the literature reviewed, it can be concluded that the use of autogenous bone grafts in the reconstruction of atrophic alveolar ridges is a treatment with a high rate of success, attaining 94.47% in the present study. Donor regions such as mandibular branch and symphisis may be used in treatments such as maxillary sinus lifts and onlay and inlay type grafts, provided that these offer bone in sufficient quantity for the proposed graft. In this study, the success rate for the technique of lifting the maxillary sinus floor was 96.43%, which suggests that this form of treatment is the most predictable in terms of bone reconstruction.
Collaborators
R ORTEGA LOPES was responsible for the conception and composition of the article. VC ANDRADE, CF NÓIA, CPV CIDADE and HDM CHAVES NETTO were responsible for the bibliographical survey and composition of the article. R MAZZONETTO was responsible for orientation and the composition of the article.
REFERENCES
1. Mazzonetto R, Nascimento FFAO, Chaves-Netto HDM. Enxertos ósseos em implantodontia. Nova Odessa: Editora Napoleão; 2011. [ Links ]
2. McAllister BS, Haghighat K. Bone augmentation techniques. J Periodontol. 2007;78(3):377-96.
3. Anner R, Grossmann Y, Anner Y, Levin L. Smoking, diabetes mellitus, periodontitis, and supportive periodontal treatment as factors associated with dental implant survival: a long-term retrospective evaluation of patients followed for up to 10 years. Implant Dent. 2010;(1):57-64.
4. Mazzonetto R. Reconstruções em implantodontia: protocolos clínicos para o sucesso e previsibilidade. Nova Odessa: Editora Napoleão; 2009.
5. Levin L, Herzberg R, Dolev E, Schwartz-Arad D. Smoking and complications of onlay bone grafts and sinus lift operations. Int J Oral Maxillofac Implants. 2004;19(3):369-73.
6. Schwartz-Arad D, Levin L. Multitier technique for bone augmentation using intraoral autogenous bone blocks. Implant Dent. 2007;16(1):5-12.
7. Cohen A, Laviv A, Berman P, Nashef R, Abu-Tair J. Mandibular reconstruction using stereolithographic 3-dimensional printing modeling technology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(5):661-6.
8. Jensen OT, Kuhlke L, Bedard JF, White D. Alveolar segmental sandwich osteotomy for anterior maxillary vertical augmentation prior to implant placement. J Oral Maxillofac Surg. 2006;64(2):290-6.
9. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38(8):613-6.
10. Olate S, de Oliveira GR, Jaimes M, Albergaria Barbosa JR. Recuperación ósea em procedimientos de reconstrución y colocación de Implantes. Int J Morphol. 2007;25(3):649- 57.
11. Levin L, Nitzan D, Schwartz-Arad D. Success of dental implants placed in intraoral block bone grafts. J Periodontol. 2007;78(1):18-21.
12. Misch CM, Misch CE. The repair of localized severe ridge defects for implant placement using mandibular bone grafts. Implant Dent. 1995;4(4):261-7.
13. Buyukkurt MC, Tozoglu S, Yazuz MS, Aras MH. Simulation of sinus floor augmentation with symphysis bone graft using threedimensional computerized tomography. Int J Oral Maxillofac Surg. 2010;39(8):788-92.
14. Dik EA, Ruiter AP, van der Bilt A, Koole R. Effect on the contour of bone and soft tissue one year after harvesting chin bone for alveolar cleft repair. Int J Oral Maxillofac Surg. 2010;39(10):962- 7.
15. Andersson L. Patient self-evaluation of intra-oral bone grafting treatment to the maxillary frontal region. Dent Traumatol. 2008;24(2):164-9.
16. Esposito M, Hirsh J-M, Lekholm U, Thomsen P. Biological factors contributing to failures of ossointegrated oral implants (I). Success criteria and epidemiology. Eur J Sci. 1998;106(1):527- 51.
17. Schawartz-Arad D, Laviv A, Levin L. Failure causes, timing, and cluster behavior: an 8-year study of dental implants. Implant Dent. 2008;17(2):200-7.
 Correspondence to:
Correspondence to:
R Ortega -Lopes
e-mail: rafaellopes@fop.unicamp.br
Received on: 6/8/2010
Final version resubmitted on: 4/2/2011
Approved on: 19/3/2011













