Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.1 Porto Alegre Jan./Mar. 2012
ORIGINAL / ORIGINAL
COX-2 selective nonsteroidal anti-inflammatory drugs and pain control after periodontal surgeries: a pilot study
Anti-inflamatórios não esteroidais COX-2 seletivos e o controle da dor após cirurgias periodontais: estudo piloto
João Paulo STEFFENS I; Fábio André SANTOS I; Gibson Luiz PILATTI I
I Universidade Estadual de Ponta Grossa, Programa de Pós-Graduação em Odontologia. Av. Carlos Cavalcanti, 4748, 84030-900, Ponta Grossa, PR, Brasil
ABSTRACT
Objective
The purpose of this pilot study was to evaluate the effectiveness of two COX-2 selective non-steroidal anti-inflammatory drugs on pain control after open flap debridement.
Methods
For this parallel, double-blind, placebo-controlled randomized clinical trial, 18 open flap debridement procedures were performed in patients from the Department of Periodontology of Universidade Estadual de Ponta Grossa with periodontal disease after nonsurgical treatment in at least one sextant. The patients were randomly allocated to one of the following groups and medicated one hour before surgery: G1- 200 mg celecoxib (n=6); G2- 90 mg etoricoxib (n=6); G3- placebo (n=6). Pain intensity was then assessed by the visual analogue scale and 101-point numerical rating scale within 8 hours of surgery.
Results
Pain intensity in G2 was significantly lower than in G3 1 and 3 hours after surgery.
Conclusion
The use of a preemptive single-dose of 90 mg etoricoxib proved to be effective for initial pain control after open flap debridement. NCT00970112.
Indexing terms: Anti-inflammatory agents, non-steroidal. Pain, postoperative. Surgery oral.
RESUMO
Objetivo
Avaliar a eficácia de dois anti-inflamatórios não esteroidais COX-2 seletivos no controle da dor após cirurgia a retalho para raspagem e alisamento radicular.
Métodos
Neste ensaio clínico randomizado, paralelo, duplo-cego, placebo-controlado, foram realizadas 18 cirurgias para raspagem e alisamento radicular em pacientes que se apresentassem à clínica de Periodontia da Universidade Estadual de Ponta Grossa com doença periodontal após terapia periodontal básica em pelo menos um sextante. Os pacientes foram aleatoriamente alocados em um dos seguintes grupos, recebendo a medicação uma hora antes de cada procedimento: G1 - celecoxibe 200 mg (n=6); G2 - etoricoxibe 90 mg (n=6); G3 - placebo (n=6). A intensidade da dor foi avaliada através de escala visual analógica e escala numérica de 101 pontos durante 8 horas após a cirurgia.
Resultados
A intensidade de dor pós-operatória no grupo G2 foi estatisticamente inferior ao grupo G3 nos períodos de 1 e 3 horas pós-operatórias.
Conclusão
O uso do etoricoxibe 90 mg em dose única pré-operatória mostrou-se efetivo no controle inicial da dor após cirurgias periodontais para raspagem e alisamento radicular. NCT00970112.
Termos de indexação: Antiinflamatórios não esteróides. Dor pós-operatória. Cirurgia bucal.
INTRODUCTION
Pain and discomfort after surgical or nonsurgical periodontal therapy are common. Scaling and root planing is one of the most common periodontal procedures in clinical practice but there may be pain after the procedure1. Most patients (77%) experience pain after scaling and root planing and the mean duration of moderate to intense pain is 6.1 hours1-2. Periodontal surgery also causes pain and discomfort, often more intense than those stemming from scaling and root planing3. Comparing different periodontal therapies, 79% of the patients report pain after open flap debridement, 89% after gingivectomy and 93% after osseous resection. The factors that can influence postoperative pain include age, therapeutic modality, region, surgery duration and extension, and psychometric analysis values3.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are useful for preventing and relieving pain. They act by inhibiting the enzyme cyclooxygenase (COX), which promotes the release of prostaglandins, prostacyclins and thromboxanes, and activates phagocytes, which, in turn, promote the release of proinflammatory cytokines in response to tissue trauma. These chemical mediators promote a state of hyperalgesia by sensitizing nociceptors, resulting in pain4. At least two COX isoforms have been identified: COX-1 is predominantly constitutive and expressed in different tissues, such as the stomach, intestine, kidneys and platelets. It has a protective role in the gastrointestinal tract; COX-2 responds to tissue trauma and produces prostaglandins involved in the inflammatory response and pain mediation5.
In the 1990's, NSAIDs that specifically inhibited COX-2 were introduced in the market to minimize gastrointestinal adverse effects associated with common NSAIDs. These drugs were especially beneficial to patients at risk of gastrointestinal bleeding or with a history of peptic ulcer6. Furthermore, these COX-2 selective NSAIDs, generically called coxibs, did not inhibit platelet aggregation like other NSAIDs did, allowing them to be used preoperatively to prevent nociceptor sensitization without increasing the risk of intraoperative bleeding7. Another advantage of coxibs was their long-lasting effect, so patients do not have to take them as frequently8.
Celecoxib was the first COX-2 selective drug to be approved by the United States Food and Drugs Administration (FDA). It is indicated for the treatment of rheumatoid arthritis, osteoarthritis, acute pain and dysmenorrhea in adults9. This medication has a COX-2 to COX-1 specificity ratio of 30, elimination half-life of approximately 12 hours and a number needed to treat (NNT) of 4.2 for a dosage of 200mg (that is, for every 4.2 patients that use the drug, 1 has at least 50% of the pain relieved during 4 to 6 hours)8,10.
Etoricoxib is a second-generation coxib. This medication is indicated for acute pain in some countries. Its chronic use has not yet been approved by the FDA9. In Brazil, it is sold in dosages of 60 and 90mg. This drug is more than 10 times more specific for the enzyme COX-2 than celecoxib, has twice the elimination half-life and a 120mg dose has an NNT in dentistry of only 1.68,11.
The objective of this pilot study was to compare how well preemptive analgesia with celecoxib and etoricoxib prevented and controlled pain after open flap debridement.
METHODS
Study design
Eighteen patients from the Department of Periodontology of the State University of Ponta Grossa with indication of open flap debridement between August 2008 and July 2009 participated in this randomized, double-blind, parallel-group, pilot study. The inclusion criteria were: patients of both genders, aged 18 to 55 years, diagnosed with chronic, moderate to severe generalized periodontitis in at least one sextant with clinical signs of the disease (bleeding upon probing and/ or suppuration) and a probing depth of 5 mm or more after nonsurgical periodontal treatment. Patients with a history of systemic diseases such as diabetes mellitus, uncontrolled hypertension, gastric ulcer, kidney or liver failure, pregnancy, nursing, allergic to any of the study drugs, chronic users of painkillers or anti-inflammatory drugs, and/or patients at risk of infectious endocarditis were excluded from the study. The nature of the study was explained previously to each patient and those who agreed to participate signed a free and informed consent form. The study was approved by the local Research Ethics Committee under protocol number 051/2008 and followed the ethical principles set forth by the Declaration of Helsinki (2000) and pertinent Brazilian laws.
Each patient was randomly assigned by lot to receive preemptive oral medication one hour before the procedure, as follows: Group (G) 1- celecoxib 200 mg (Celebra, Pfizer, São Paulo, Brazil); G2 - etoricoxib 90 mg (Arcoxia, Merck Sharp & Dohme, Campinas, Brazil); and G3 - placebo. A second researcher (GLP) was assigned to medicate the volunteers because of the double-blind nature of the study. Hence, the drug taken by the patient was unknown to the patient and surgeon.
Surgical technique
The patients were anesthetized with 2% mepivacaine with norepinephrine at 1:100,000. The anesthetic technique depended on the affected region. An intrasulcular incision was done to reflect the vestibular and lingual mucoperiosteal flap, exposing the crestal bone. The root surfaces were instrumented with Gracey and McCall curettes (according to the operated region) and ultrasound (10P ultrasonic tip, Jet-Sonic Plus, Gnatus, Ribeirão Preto, Brazil) until a smooth surface free from accretions (plaque and calculus) was obtained by visual inspection and confirmed by probing by an expert (GLP). A simple, circumferential suture was done with a 4.0 silk suture (Shalon Suturas, São Luis de Montes Belos, Brazil). All surgeries were performed by an expert periodontist (JPS).
Postoperative recommendations
A blister pack of four 750mg-tablets of paracetamol (additional painkiller) was given to each patient after surgery. They were advised to take the drug only if necessary, at six-hour intervals if the pain persisted and to take down, in the assessment form, the time each tablet was taken. Instructions for filling out the assessment forms were also given to the patients after surgery. The patients were also prescribed 15ml of 0.12% chlorhexidine gluconate (PerioGard, Colgate-Palmolive, São Bernardo do Campo, Brazil) to rinse the oral cavity gently for 1 minute at 12-hour intervals starting the day after surgery until the stitches were removed, 7 days after surgery.
Pain assessment
Postoperative pain intensity was recorded in an assessment form given to each patient after the surgery. This assessment was done hourly for the 8 hours that followed. Two postoperative pain assessment methods were used: the visual analogue scale (VAS), consisting of a 10-cm line and both ends closed by vertical lines which correspond to no pain and maximum pain, and the 101-point numerical rating scale (NRS-101), consisting of asking the patient to give a score to his/her pain ranging from 0 (no pain) to 100 (maximum pain).
Statistical treatment
The data from both pain scales were grouped and then analyzed by the Kruskall-Wallis test (with Dunn's post test) for each study period. The significance level was set to 5%.
RESULTS
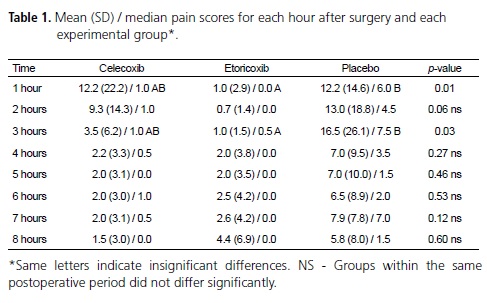
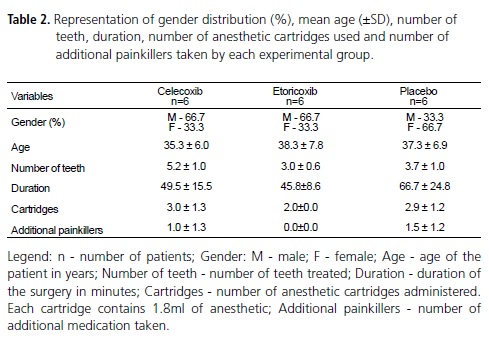
Eighteen patients, 10 males and 8 females, aged 27 to 51 years (37±6.7 years) completed the study. The means, standard deviations and medians of the pain experienced by the groups celecoxib, etoricoxib and placebo are shown in Table 1. Pain intensity felt by groups etoricoxib and placebo differed significantly at 1 and 3 hours after surgery (p<0.05). The distribution of gender, age, number of teeth, duration of surgery, number of anesthetic cartridges and number of painkillers taken after surgery by each patient of each group are shown in Table 2. No adverse effects were reported for any of the medications. The main postoperative complaint was related with dentinal hypersensitivity, treated with desensitizers containing 2% potassium nitrate and 2% sodium fluoride (Dessensibilize KF 2%, FGM, Joinville, Brazil). The patients were also given a topical gel containing 2% sodium fluoride for use twice daily (Flugel, DFL, Rio de Janeiro, Brazil).
DISCUSSION
The present study found that 90mg of etoricoxib is better than placebo for controlling pain 1 and 3 hours after periodontal surgery when used preemptively. A study comparing different dosages of etoricoxib for relieving moderate to intense pain after extraction of third molars found that the minimum clinically effective dosage was 120mg12. However, the Brazilian Health Vigilance Agency (ANVISA) established that this drug could not be sold in Brazil in concentrations higher than 90mg per tablet.
Celecoxib can also be used in doses higher than those used in the present study, increasing its analgesic effect. For example, the NNT of celecoxib 400mg is 2.5, almost half of the NNT of celecoxib 200mg (NNT=4.2)8. However, the main advantage of etoricoxib over celecoxib is the greater elimination half-life of the former, allowing it to be used only once daily, as opposed to twice daily for celecoxib10, facilitating patients' adherence to treatment.
Pharmacological postoperative pain prevention and control have been the target of some literature studies13-14. In this research line, the preoperative use of anti-inflammatory medications is based on an attempt to prevent the inflammation associated with tissue injury, which culminates with nociceptor sensitization, translating into pain. Preoperative medication has been shown to be more efficient than preoperative placebo15 but this protocol has not been proven to be better than postoperative medication16. Evidently, these results should be interpreted with caution, considering the medications that were tested, their pharmacological properties, and the type of surgery.
The use of COX-2 selective NSAIDs is being discussed everywhere because of the increased cardiovascular problems experienced by patients taking them. However, risk increases with dosage and treatment duration10. The dosage and treatment duration used in the present study are safe. The main advantage of using COX-2 selective NSAIDs as preemptive painkillers is that they do not affect bleeding time or platelet aggregation, both mediated by COX-117.
The expectation of pain after open flap debridement can be compared with that after nonsurgical periodontal treatment2-3, which can cause pain of variable degrees of intensity and duration1. Nevertheless, the existence of a statistical difference between the two experimental groups proves that pain is in fact present after this type of surgery, validating the study methodology.
The visual analogue scale and NRS-101 present good agreement and sensitivity for the assessment of acute pain after surgical procedures and both are better than the 4-point verbal rating scale (VRS-4). The NRS- 101 is easier to understand and can be used by patients with poor vision and/or dexterity18.
Some limitations of this pilot study need to be considered. Variables such as anxiety, operated region and surgery time, for example, can influence the perception of postoperative pain, but were not investigated in the preliminary analysis. Furthermore, the small sample may have biased the results. This information must be considered for a better understanding of the study results. The effect of painkillers on postoperative pain does not seem to be relevant in this study, since all patients used the same salt and vasoconstrictor, that is, the pharmacokinetic properties of the local anesthetic were the same for all groups. This fact could affect only the assessment of pain at different times, and this analysis was not considered.
CONCLUSION
Despite the limitations of the present study, the use of 90mg of etoricoxib in a single, preoperative dose proved effective for the initial control of pain following open flap debridement.
Collaborators
JP STEFFENS selected the patients, got their medical histories, performed the surgeries, did the immediate postoperative follow-up and helped to write the manuscript. FA SANTOS randomized the patients, supervised the surgeries, collected the pain assessment forms and helped to write the manuscript. GL PILATTI read and interpreted the data, performed the statistical analysis, supervised the surgeries and helped to write the manuscript.
REFERENCES
1. Pihlstrom BL, Hargreaves KM, Bouwsma OJ, Myers WR, Goodale MB, Doyle MJ. Pain after periodontal scaling and root planing. J Am Dent Assoc. 1999;130(6):801-7. [ Links ]
2. Canakçi CF, Canakçi V. Pain experienced by patients undergoing different periodontal therapies. J Am Dent Assoc. 2007;138(12):1563-73.
3. Matthews DC, McCulloch CA. Evaluating patient perceptions as short-term outcomes of periodontal treatment: a comparison of surgical and non-surgical therapy. J Periodontol. 1993;64(10):990-7.
4. Czock D, Keller F, Rasche FM, Häussler U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet. 2005;44(1):61-98.
5. Jeske AH. COX-2 inhibitors and dental pain control. J Gt Houst Dent Soc. 1999;71(4):39-40.
6. Hawkey CJ, Jones JI. Gastrointestinal safety of COX-2 specific inhibitors. Gastroenterol Clin North Am. 2001;30(4):921-36.
7. Straube S, Derry S, McQuay HJ, Moore RA. Effect of preoperative Cox-II-selective NSAIDs (coxibs) on postoperative outcomes: a systematic review of randomized studies. Acta Anaesthesiol Scand. 2005;49(5):601-13.
8. Derry S, Barden J, McQuay HJ, Moore RA. Single dose oral celecoxib for acute postoperative pain in adults. Cochrane Database Syst Rev. 2008;8(4):CD004233.
9. Khan AA, Dionne RA. The COX-2 inhibitors: new analgesics and anti-inflammatory drugs. Dent Clin North Am. 2002;46(4):679- 90.
10. Shi S, Klotz U. Clinical use and pharmacological properties of selective COX-2 inhibitors. Eur J Clin Pharmacol. 2008;64(3):233- 52.
11. Clarke R, Derry S, Moore RA, McQuay HJ. Single dose oral etoricoxib for acute postoperative pain in adults. Cochrane Database Syst Rev. 2009;15(2):CD004309.
12. Malmstrom K, Sapre A, Coughlin H, Agrawal NGB, Mazenko RS, Fricke JR Jr. Etoricoxib in acute pain associated with dental surgery: A randomized, double-blind, placebo- and active comparator-controlled dose-ranging study. Clin Ther. 2004;26(5):667-79.
13. Rashwan WA. The efficacy of acetaminophen-caffeine compared to ibuprofen in the control of postoperative pain after periodontal surgery: a crossover pilot study. J Periodontol. 2009;80(6):945-52.
14. Steffens JP, Santos FA, Sartori R, Pilatti GL. Preemptive dexamethasone and etoricoxib for pain and discomfort prevention after periodontal surgery: a double-masked, crossover, controlled clinical trial. J Periodontol. 2010;81(8):1153-60.
15. Joshi A, Parara E, Macfarlane TV. A double-blind randomised controlled clinical trial of the effect of preoperative ibuprofen, diclofenac, paracetamol with codeine and placebo tablets for relief of postoperative pain after removal of impacted third molars. Br J Oral Maxillofac Surg. 2004;42(4):299-306.
16. Jung YS, Kim MK, Um YJ, Park HS, Lee EW, Kang JW. The effects on postoperative oral surgery pain by varying NSAID administration times: comparison on effect of preemptive analgesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(5):559-63.
17. Dallob A, Hawkey CJ, Greenberg H, Wight N, De Schepper P, Waldman N, et al. Characterization of etoricoxib, a novel, selective COX-2 inhibitor. J Clin Pharmacol. 2003;43(6):573-85.
18. Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Breivik Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17-24.
 Correspondence to:
Correspondence to:
GL PILATTI
e-mail: gibsonpilatti@gmail.com
Received on: 18/10/2010
Approved on: 3/4/2011













