Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.2 Porto Alegre Abr./Jun. 2012
ORIGINAL / ORIGINAL
Radiopacity of resin cements: in vitro study
Radiopacidade de cimentos resinosos: estudo in vitro
Luana Osório FERNANDES I; Patricia Fernandes CASSIMIRO-SILVA I; Mirella Emerenciano MASSA I; Ricardo Ferreira PEDROSA I; Silvana Maria Orestes CARDOSO I
I Universidade Federal de Pernambuco, Faculdade de Odontologia. Av. Prof. Moraes Rego, 1235, Cidade Universitária, 50670-901, Recife, PE, Brasil
ABSTRACT
Objective
To evaluate the radiopacity of seven different resin cements, noting whether they are in accordance with the requirements of ANSI/ADA no. 27/1993 and ISO no. 4049/2000, comparing the conventional radiographic system with digital (phosphor plate).
Methods
For each material, five samples were prepared that were irradiated and tested in both systems; the optical density of the cement and each step-wedge of the penetrometer were measured. From the resulting values, the equivalent for each mm of aluminum material was obtained.
Results
We found the lowest values in AllCem-FGM, Joinville, Brazil (2.06 and 4.63 Eq mmAl), and the highest values in the Fill Magic Dual Cement- Vigodent, Rio de Janeiro, Brazil (4.03 and 9.20 mmAl eq). Through the F-test (ANOVA) with two factors, a significant difference was confirmed between the two system types (p <0.05) and between cements (p <0.05). On the other hand, the interaction between type of system and cement was not significant (p> 0.05). Through the Tukey test, a significant difference was found between the cement Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil) and each of the other cements: AllCem (FGM, Joinville, Brazil), Cement Post (Angelus, Londrina, Brazil), RelyX Unicem (3M ESPE, St. Paul, MN, USA), SET (SDI, Victoria, Australia), regardless of the system.
Conclusion
All cements fell within the standards, where the AllCem (FGM, Joinville, Brazil) had the lowest value of radiopacity and Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil) the highest, irrespective of the type of system.
Indexing terms: Densitometry. Dental digital radiography. Resin cements.
RESUMO
Objetivo
Avaliar a radiopacidade de sete cimentos resinosos diferentes, observando se os mesmos encontram-se de acordo com as normas da ANSI / ADA n. 27/1993 e ISO n. 4049/2000, comparando-se o sistema radiográfico convencional com o digital (placa de fósforo).
Métodos
Para cada material confeccionaram-se cinco amostras, que foram irradiadas, e analisadas em ambos os sistemas, mediram-se a densidade óptica dos cimentos e de cada degrau do penetrômetro. A partir dos valores encontrados obteve-se o equivalente em milímetros de alumínio para cada material.
Resultados
Constatou-se menores valores no AllCem-FGM, Joinville, Brasil (2,06 e 4,63 Eq mmAl), e maiores no Fill Magic Dual Cement-Vigodent, Rio de Janeiro, Brasil (4,03 e 9,20 Eq mmAl) . Através do teste F (ANOVA) com dois fatores se comprovou diferença significativa entre os dois tipos de sistema (p < 0,05) e entre os cimentos (p < 0,05). Por outro lado, a interação do tipo de sistema e cimento não se mostrou significativa (p > 0,05). Através do teste de Tukey se evidenciou diferença significativa entre o cimento Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brasil) com cada um dos cimentos: AllCem (FGM, Joinville, Brasil), Cement Post (Angelus, Londrina, Brasil), RelyX Unicem (3M ESPE, Saint Paul, EUA), seT (SDI, Victória, Austrália), independente do tipo de sistema.
Conclusão
Todos os cimentos estavam dentro das normas, onde o AllCem (FGM, Joinville, Brasil) apresentou menores valores de radiopacidade e o Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brasil) os maiores, independente do tipo de sistema.
Termos de indexação: Densitometria. Radiografia dentária digital. Cimentos de resina.
INTRODUCTION
Dental cement is defined as a moldable substance that promotes the bonding of juxtaposed surfaces, as well as functioning as a thermal, electrical and chemical insulator1. These dental materials promote the retention of the prosthetic item on the tooth remnant, the sealing of the tooth/restoration interface, the mechanical support for the restorative material, the sealing of the dentinal tubules and also adequate esthetic results2.They are used to cement indirect composite resin restorations, ceramic inlays and onlays, ceramic crowns and fixed, partial prostheses to cavity preparations and abutment teeth3-4.
Radiopacity is one of the principal prerequisites of these dental cements, since it is by means of radiographs that the clinician is able to conclude his/her diagnosis in terms of the presence of recurring caries, detect gaps and excess restorative material, mainly in areas where it is difficult to gain access5-6.
Today, one of the leading cementation materials available in the marketplace is still the cement popularly known as zinc phosphate1. However, despite its good radiopacity, evidenced by Attar et al.6 as the most radiopaque cement found in her study, certain undesirable properties such as its solubility in the oral environment1 prompted the search for a cementation material containing the ideal characteristics. This quest has been intense in recent years and lately the tendency has been toward the adhesive technology of resin-based cements, as they have the big advantage of adhesion, not only to the dental structure, but also to metal alloys, composite resins and porcelain and they are practically insoluble7. With the advent of these cements, therefore, it has been possible to circumvent the problems with bonding resistance and wear and tear8. However, despite these scientific advances in dentistry, there has still not been a great deal of research4-6,9-11 addressing the radiopacity of these cementing agents.
At the present time, the clinician has at his/ her disposal two radiographic systems available in the marketplace: conventional and digital. The digital radiation detection system has emerged as an alternative to dental radiographic film, since this furnishes an analogue image that is unalterable, while the digital image may be altered according to requirements, as well as providing a reduction in the radiation dose, as it is more sensitive. There are two main types currently being used: the coupled charge device and the phosphor plate12.
The coupled charge device is actually a rather thick but essentially small sensor, connected by cable directly to the computer and, after exposure to x-rays, it will provide an almost instantaneous image on the screen12. The phosphor-plate system used in the present study looks, on the outside, like a conventional periapical film, with a similar area and thickness, but it does not have a cable connected to a computer. With this type of sensor, the digital image that is formed is obtained through exposure to x-rays, read by a specific type of scanner where the information resulting from the interaction of receiver and image reader is subsequently converted into machine language and thus the digital radiographic image is created12-13.
The aim of the present study was to ascertain the degree of radiopacity of some resin-based cements used in Dentistry, checking if they are in agreement with ISO standard 4049/2000 (International Organization for Standardization)14 and ANSI/ADA specification no. 27/1993 (American National Standard / American Dental Association Specification)15 for radiopacity, as well as to check if there is any difference in relation to the radiopacity of the cements used in conventional radiography and digital radiography.
METHODS
Preparation of the specimens
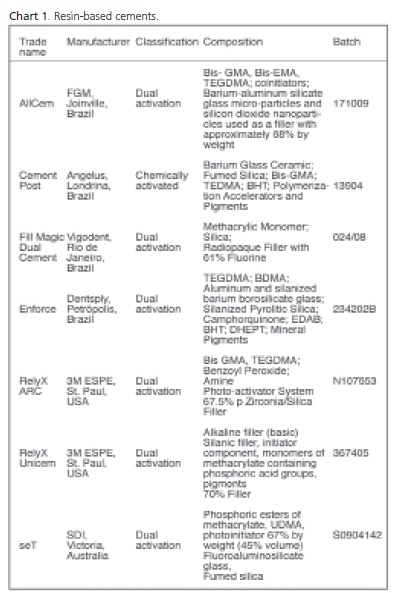
A total of seven resin-based cements were used: AllCem (FGM, Joinville, Brazil), Cement Post (Ângelus, Londrina, Brazil), Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil), Enforce (Dentsply, Petrópolis, Brazil), RelyX ARC (3M ESPE, St. Paul, USA), RelyX Unicem (3M ESPE, St. Paul, USA) and seT (SDI, Victoria, Australia) as shown in Chart 1.
For the experiment, 10 specimens were prepared of each material and then 5 were selected which exhibited, in radiographic terms, the most uniform surfaces. To this end, and with the aim of standardizing the samples, a brass mold was used composed of two threaded parts, with a hole in the center with a diameter of 10 mm and depth of 2 mm, in conformity with ANSI/ADA standard no. 2715, and encircling walls at an angle of approximately 8º (to facilitate the removal of the samples after photopolymerization). Allied to this, a device made of aluminum was used to help with the removal of the samples from the mold, which had been lined in advance using Vaseline.
The materials were handled and inserted in accordance with the manufacturer’s standards, and slowly in order to avoid the formation of blisters on the material. After filling the mold with the cement, this was leveled with the aid of a polyester strip and 10 mm glass plate previously coated with Vaseline. The materials were then photopolymerized in the mould by means of the cordless LED curing light equipment Radii (SDI, Victoria, Australia), which is composed of blue LEDs that emit light at a maximum intensity of 1500 mw/cm2, as verified by a radiometer.
The duration of the photopolymerization was that recommended by the manufacturers. After photopolymerization, the mold was opened and a second photopolymerization was carried out on the opposite side. Sanding discs (TDV, Santa Catarina, Brazil) with the finest granulations were used to remove the excess and to give a finish. After all the samples were prepared, and with the aim of checking the standardization, the thicknesses were calibrated using a Starrett digital precision pachymeter (Itu, Brazil).
X-Ray Apparatus
Radiographs were taken using Dabi Atlante apparatus (Ribeirão Preto, Brazil) of the type Spectro 70 X Class I type B, with 70 kVp and 8 mA, a total filtering equivalent to 2.71 mm of aluminum. The exposure time was 0.6 seconds, by means of prior selection, via trial and error with the aim of producing images with contrast levels similar to those obtained in the clinic, both for conventional film and for the phosphor-plate sensor. The accuracy, precision and reproducibility of the X-ray apparatus were previously evaluated using an RMI 242 (Gammex, Middleton, USA) belonging to the Metrology Laboratory of the Nuclear Energy Department at the Federal University of Pernambuco.
EXPOSURE OF SAMPLES TO X-RAYS
Conventional film
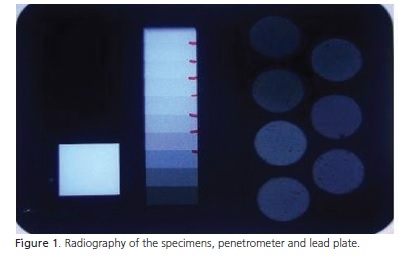
Insight occlusal film (Eastman Kodak, New York, USA) with E/F sensitivity - (24 to 96 R*) was used for the radiography of the specimens, an aluminum penetrometer and a lead sample. The penetrometer is a 99.5% pure aluminum device comprising 10 step-wedges which vary in thickness every 2 millimeters, used to check the quantity of ionization and the reduction in the salts of silver in films.
In each of the 5 conventional occlusal films, a group of 7 specimens was created, one for each resinbased cement, the penetrometer and the lead sample (Figure 1). Each group and film was duly placed on a polystyrene support arranged on a fixed table, from which the focus film distance (FFD) of 40 cm was measured, as recommended by ISO 4049, with the aim of obtaining a large area of exposure to the x-rays, but without causing any discrepancies therein.
Digital system
The same groupings of cement, aluminum penetrometer and lead plate exposed using the conventional system, were irradiated for the digital system using two phosphor-plate sensors arranged side by side to be equivalent to the size of the occlusal film used previously. Once again, each group and film was duly placed on a polystyrene support laid out on a fixed table, from which a focus-film distance of 40 cm was measured.
OBTAINING THE RADIOGRAPHIC IMAGE
Conventional film
The films were processed for 2 to 3 hours after exposure to the x-rays. The developing was carried out manually in a darkroom using the temperature/time method measured using the immersion thermometer belonging to the Metrology Laboratory of the Nuclear Energy Department at the Federal University of Pernambuco. The developer and fixer used were from Kodak Dental (New York, USA). After processing, they were dried in a warm air dryer.
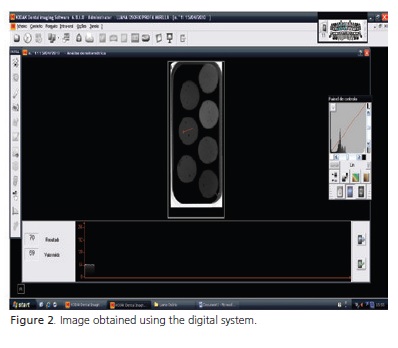
Digital system (phosphor plate)
The sensors were removed from the protective covers and located in a specific place inside the Kodak CR7400 scanner (New York, USA) for reading by laser. One image was generated for each sensor using the program known as Kodak Dental Imaging Software 6.8.6.0. (Figure 2).
MEASURING OPTICAL DENSITY
Conventional film
The radiographs were evaluated for optical density using an MRA 07-443 photodensitometer belonging to the Nuclear Physics Department at the Federal University of Pernambuco, calibrated on the basis of manufacturer specifications. Firstly, a reading was taken of the basedensity plus fog, which would simply be the reading of the radiographic density of the lead plate. Then the measurement was obtained of the optical densities of the specimens and penetrometer. The optical density of the penetrometer is obtained from just one reading of each step-wedge. As far as the specimens were concerned, five readings were performed in random locations on each body and the results were expressed in the form of the arithmetic mean. From the resulting values the basedensity plus fog value is subtracted from the optical density thereby obtaining the net optical density, the aim of which was to establish the aluminum equivalence, in millimeters, of the materials being studied.
Digital system
To create the digital radiographic image, a detector was used which converts all information into electronic signals called bits. A bit (binary digit) is the smallest unit used in computers and has a numeric value of either 0 or 1. A group of 8 bits forms a byte and one byte can contain 256 different values representing the numbers from 0 to 255.
After receiving the information of the upcoming image, the computer usually stores it in analog form and then the signals undergo analog to digital conversion. The digital scanning of the image leads to a number of figures arranged in a matrix of X Y coordinates where each dot corresponds to one pixel, which may assume a variety of shades of gray. The larger the matrix the greater the number of pixels and consequently the better the image resolution.
The histogram tool is used to determine the mean of the gray scale which goes from a value of 0 (black) to 255 (white), of the region of the radiographs containing the samples. In order to read them, a line is traced in the most uniform area of the image of the specimen and penetrometer (Figure 2). This line passes through areas of different densities and the software automatically obtains a mean for these values. These means are equivalent to the shades of gray. Unlike the density measurements of conventional film, digital film registers the darkest areas with the lowest values, a fact which leads us to invert the optical density values obtained in the digital system, transforming them into black via the following equation:
Inverse of gray = 255 – grayscale value
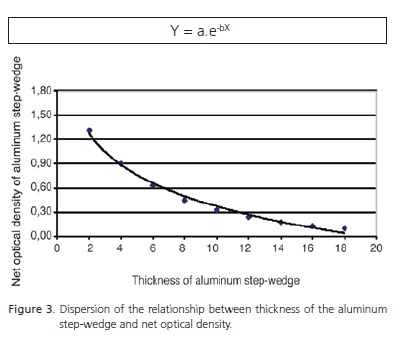
Aluminum equivalence in millimeters
In order to obtain aluminum equivalence in millimeters, a net optical density (or inverse of gray) graph was generated versus the Step-wedge of aluminum in millimeters of the penetrometer for each radiographic film (image), where Y equals the net optical density (or inverse of gray), X equals the value of aluminum equivalence in millimeters and a and b are the regression parameters generated for each curve (Figure 3). An equation is obtained from each graph which is used to find the aluminum equivalence of the cement, in millimeters. For this, the net optical density (or inverse of gray) of the aluminum is replaced by that of the cements on the same radiographic film (image).
Statistical analysis
The data were subjected to statistical analysis. The values in equivalence of mmAl were summarized through the usual numerical measures of location (mean and median) and dispersion (minimum value, maximum value, coefficient of variation and standard deviation). To ascertain the effect of the type of material and type of system on equivalence in mmAl, a variance analysis was performed using two classification factors.
Comparisons between pairs of means were carried out using the F-test (ANOVA for two factors) with interaction and Tukey’s multiple comparisons. The margin of error used in the statistical test decision was 5%.
The data were input to an Excel spreadsheet and the program used to obtain the statistical calculations was the Statistical Package for the Social Sciences (SPSS), version 15.
RESULTS
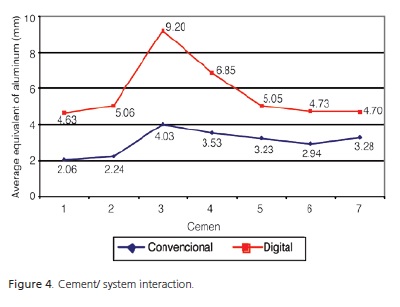
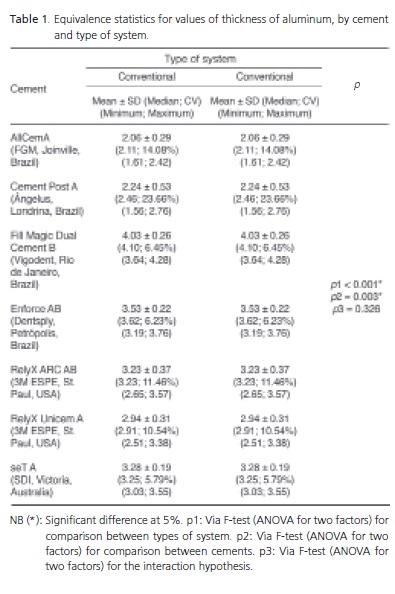
When taking into account the net optical density or the inverse of gray of the cement specimens, in the conventional and digital systems, respectively, it was found that each value had a corresponding value in millimeters of aluminum. Per Table 1, the means of aluminum equivalence of each cement were commensurately higher in the digital system than the conventional one. Moreover, in each type of system, it was noted that the cement Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil) obtained the highest mean for the thickness of aluminum, in millimeters, followed by the cement RelyX ARC (3M ESPE, St. Paul, USA).
By means of the F-test (ANOVA) with two factors, a significant difference is confirmed between the two types of system (p < 0.05) and between cements (p < 0.05) and the interaction between type of system and the cement was seen not to be significant (p > 0.05). Through the Tukey test, a significant difference was found between the cement Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil) with all the other cements: AllCem (FGM, Joinville, Brazil), Cement Post (Ângelus, Londrina, Brazil), RelyX Unicem (3M ESPE, St. Paul, USA), SeT (SDI, Victoria, Australia), irrespective of system type.
Overall, it can be seen from Figure 4 that the lines are roughly parallel, proving that the cements had the same level of radiopacity in both systems and there was no significant difference in terms of cement/system interaction.
DISCUSSION
In order to evaluate the radiopacity of different materials, a device composed of ten aluminum stepwedges is used, each step-wedge having a characteristic thickness and with a purity of as much as 99.5%, known as a penetrometer. The use of this metal is recommended as it has a degree of linear absorption similar to that of dentin16.
In the literature, there is no consensus as to the desirable level of radiopacity. Akerboom et al.10 and Rosenstiel et al.17 recommend that the radiopacity of cementing materials should be greater than or equal to that of dentin, while others3,5 believe that it should be greater than or equal to enamel. Goshima et al.9, however, report that this value should be greater than or equal to the thickness of aluminum, as defined by ISO 404914 and specified in ANSI/ADA no. 2715.
In the present study, all the cements evaluated fell within the radiopacity requirements required for cementing agents included in the standards issued by the ISO 404914 and ANSI/ADA15. The lowest radiopacity observed amongst the cements analyzed, regardless of type of system, was that of AllCem (FGM, Joinville, Brazil) with 2.06 Eq mmAl (Table 1), and therefore above the minimum required, as the specimens were 2 mm thick.
There was a significant difference between the cements (p<0.05) irrespective of the type of reading, confirmed using the Tukey test which showed that the cement Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil) possesses a somewhat different radiopacity, mainly in comparison with the cements AllCem (FGM, Joinville, Brazil), Cement Post (Ângelus, Londrina, Brazil), RelyX Unicem (3M ESPE, St. Paul, USA) and seT (SDI, Victoria, Australia). Amongst the materials studied, Enforce (Dentsply, Petrópolis) and RelyX ARC (3M ESPE, St. Paul, USA) presented intermediate values (Table 1).
The ideal cementing agent should be sufficiently radiopaque to allow recurring caries, marginal defects and excess material to be seen5-6,18, though this radiopacity should not be excessive, since it may have an impact on the visualization of dental structures, thus obscuring the diagnosis18.
Resin-based cements are made up of elements of inorganic filler arranged in a resin matrix normally formed by bisphenol A-glycidil methacrylate (Bis-GMA) or urethane dimethacrylate (UDMA) in combination with other monomers of lower molecular weight3.
The radiopacity of these cements depends on the type and amount of radiopaque inorganic filler in its make-up. In other words, a high percentage of filler with a high atomic number, such as barium (56), strontium (38) or zinc (30), leads to an increase in radiopacity6. Watts16 concluded that, in general, a radiopacity higher than that of enamel could be achieved by compounds containing more than 20% in mass of radiopaque oxide in the filler particles.
Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil), which demonstrated the highest radiopacity, is composed of a filler of 61%, while AllCem (FGM, Joinville, Brazil), which demonstrated the lowest radiopacity, had a filler of 68% by weight (Chart 1). The highest values obtained by the cement Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil) may be due to a larger amount of filler with high atomic numbers when compared to AllCem (FGM, Joinville, Brazil), even with a total percentage at a lower weight.
There is no advocated and/or recommended value for the maximum limit of radiopacity19, it not being possible to state from our study that that obtained through this material was excessive. Willems20 states that the number of glasses with atoms with high atomic numbers incorporated into the cement should be limited, as this affects other properties of the composite, such as translucence.
Other factors such as the angling of the x-ray beams, the thickness of the material, the type of radiographic film and fixing solutions may also have an influence on radiopacity11. However, as the experiment was conducted in a standardized fashion, these factors did not have an impact on the results due to the use of the penetrometer.
The conventional image capture system is gradually giving way to digital since, while the former uses a radiographic film which needs to be processed for the viewing of an unalterable image, the latter generally uses sensors which, once exposed, form a digital image which can be altered according to the operator’s requirements12. Authors such as Sanderink et al.21, however, note that it is difficult to compare the digital system with the conventional one since they have totally different characteristics.
The quality of the images generated by digital systems is still inferior to that of analog images22, however, as they permit adjustments to brightness and sharpness, for example, they make it possible to obtain maximum information23. Another advantage of this technique is the possibility of adjusting exposure time and dose in order to obtain maximum precision with the diagnosis, in addition to the image being produced almost instantaneously and with no need for treatment using chemicals24.
The images in this type of system may be acquired directly, indirectly or semi-directly. The first type permits the immediate production of the image via a sensor, the coupled charge device, which is directly connected to the computer. One of the main disadvantages is the inconvenience of the diminished size and greater thickness, in comparison with conventional film25-26.
The semi-direct method uses a flexible plate, a Phosphor Storage Plate, similar to radiographic film which, after exposure to x-rays, will be read by a laser scanner and the information obtained will be transmitted to the computer to build and view the image and if necessary to manipulate it6; the systems most used with this type of sensor are the Digora (Soredex, Helsinki, Finland) and the DenOptix (Gendex, Milan, Italy)27. It should be pointed out that some authors prefer to classify this type of acquisition as direct27.
As opposed to the two systems mentioned above, the indirect digital image system uses conventional film which, after exposure for the capture of the image, is processed and scanned, to then form the image on the computer screen25-26, the disadvantage being the need for the film to be chemically processed, sophisticated digital scanning techniques and a longer lead time for the acquisition of the image23.
The building of the image in the digital system is based on the conversion of information contained in the sensors into pixels. Each pixel will have a digital value equivalent to a shade of gray, obeying an amplitude that goes from absolute black (maximum radiopacity) through to absolute white, which presents maximum radiolucency. Therefore, with digital radiography, the number of shades of gray (contrast resolution) and the size of the pixels (spatial resolution) determine the overall resolution of the digital image22.
It can be observed that there was a significant difference between the two types of system (p<0.05), the digital method presenting higher radiopacity values, regardless of type of cement, when compared to the conventional system (Table 1). However, the present study does not allow us to appraise which is the better system, since the objective was to observe the degree of radiopacity of the cements and not the sensitivity of the system. The sensitivity of a radiographic technique is usually defined as the capacity to discern variations in the thickness of the materials studied28.
CONCLUSION
Bearing in mind the results obtained in the study, we would conclude that all the cements evaluated, namely AllCem (FGM, Joinville, Brazil), Cement Post (Angelus, Londrina, Brazil), Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil), Enforce (Dentsply, Petrópolis, Brazil), RelyX ARC (3M ESPE, St. Paul, USA), RelyX Unicem (3M ESPE, St. Paul, USA) and seT (SDI, Victoria, Australia), conform to the requirements established by ANSI/ADA specification no. 27 and ISO 4049, which state that cements should have a radiopacity greater than or equal to one thickness of aluminum.
In addition, it was noted that the cement Fill Magic Dual Cement (Vigodent, Rio de Janeiro, Brazil) exhibited the highest degree of radiopacity and AllCem (FGM, Joinville, Brazil) the lowest, irrespective of the type of system, however it cannot be stated that any of the cements exceeded the maximum acceptable limit of radiopacity, since there is no maximum limit. In addition, it was found that the digital system presented the highest values, when compared to the conventional system.
Based on the information set out above, it is clear that the determination of maximum radiopacity of cementing materials, in future research, would be a huge clinical / scientific contribution.
ACKNOWLEDGMENTS
We would like to thank the Nuclear Energy Department at the Federal University of Pernambuco, and in particular Dr. Helen Khoury and the master’s student Isabela Brasileiro, for making the Metrology Laboratory available for the performance of the experimental part of the study.
Collaborators
LO FERNANDES E PFC SILVA took part in the bibliographical survey, the performance of the experimental piece (preparation of specimens, exposure of the samples to x-rays, processing to obtain the images, optical density measurements, acquisition of aluminum equivalence in millimeters, analysis of results and composition of the article. ME MASSA directed the research and took part in the bibliographical survey, assistance in the preparation of specimens, optical density measurements, analysis of results and composition of the article. RF PEDROSA was responsible for the bibliographical survey, statistical analysis of the results and the composition of the article. SMO CARDOSO took part in the bibliographical survey, acquisition of images and composition of the article.
REFERENCES
1. Campos TN, Mori M, Henmi AT, Saito T. Infiltração marginal de agents cimentantes em coroas metálicas fundidas. Rev Odontol Univ São Paulo. 1999;13(4): 357-62. doi: 10.1590/ S0103-06631999000400007. [ Links ]
2. Baratiere LN, Monteiro Junior S, Melo TS, Ferreira KB, Hilgert LA, Schilichting LH, et al. Odontologia restauradora: fundamento e técnicas. São Paulo: Editora Santos; 2010.
3. Rubo MHM, El-Mowafy O. Radiopacity of dual-cured and chemical-cured resin-based cements. Int J Prosthodont. 1998;11(1):70-4.
4. Tsuge T. Radiopacity of conventional, resin-modified glass ionomer, and resin-based luting materials. J Oral Sci. 2009;51(2):223-30.
5. El-mowafy OM, Benmergui C. Radiopacity of resin-based inlay luting cements. Oper Dent. 1994;19(1):11-5.
6. Attar N, Tam LE, McComb D. Mechanical and physical properties of contemporary dental luting agents. J Prosthet Dent. 2003;89(2):127-34. doi: 10.1067/mpr.2003.20.
7. Santos LB, Souza SM, Andrade TA, Uetanabaro APT, Rocha GP, Vilela AC. Estudo comparativo in vivo entre o cimento de fosfato de zinco e o resinoso. Odonto Clin.-Científ. 2009;8(3):257-61.
8. Prakki A, Carvalho RM. Cimentos resinosos dual: características e considerações clínicas. Rev Fac Odontol Sao Jose dos Campos. 2001;4(1):21-6.
9. Goshima T, Goshima Y. Optimum radiopacity of composite inlay materials and cements. Oral Surg Oral Med Oral Pathol. 1991;72(2):257-60. doi: 10.1016/0030-4220(91)90173-A.
10. Akerboom HBM, Kreulen CM, van Amerongen WE, Mol A. Radiopacity of posterior composite resins, composite resin luting cements, and glass ionomer lining cements. J Prosthet Dent. 1993;70(4):351-5. doi: 10.1016/0022-3913(93)90221-9.
11. Fonseca RB, Branco CA, Soares PV, Correr-Sobrinho L, Haiter- Neto F, Fernandes-Neto AJ, et al. Radiodensity of base, liner and luting dental materials. Clin Oral Investig. 2006;10:114-8. doi: 10.1007/s00784-005-0030-3.
12. Bueno NLO, Dotto SR, Ferreira R, Dotto GN, Casagrande L, Silveira BLS, et al. Radiologia odontológica e a imagem digital. J Acessor Odontol. 1999;3(15):28-33.
13. Sales MAO, Costa, LJ, Neto JBSN. Controvérsias em radiologia digital. Rev Bras Patol Oral. 2002;1(1):13-8.
14. International Organization for Standardization 4049. Polymerbased filling, restorative and luting materials. Geneva, Switzerland: International Organization for Standardization; 2000.
15. American National Standard. American Dental Association. Specification n. 27 for resin-based filling materials. Chicago, IL: American Dental Association, Council on Dental Materials and Equipament; 1993.
16. Watts DC. Radiopacity vs. composition of some barium and strontium glass composites. J Dent. 1987;15(4):38-43. doi: 10.1016/0300-5712(87)90096-0.
17. Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: a review of the current literature. J Prosthet Dent. 1998;80(3):280-301. doi: 10.1016/S0022-3913(98)70128-3.
18. Espelid I, Tveit AB, Erickson RL, Keck SC, Glasspoole EA. Radiopacity of restorations and detection of secondary caries. Dent Mater. 1991;7(2):114-7. doi: 10.1016/0109- 5641(91)90056-5.
19. Salzedas LMP, Louzada MJQ, Oliveira Filho AB. Radiopacity of restorative materials using digital images. J Appl Oral Sci. 2006;14(2):147-52. doi: 10.1590/S1678- 77572006000200015.
20. Willems G. Resinas compostas. In: Baratieri LN, Monteiro Junior S, Andrada MAC, Vieira LCC, Cardoso AC, Ritter AV. Estética: restaurações adesivas diretas em dentes anteriores fraturados. 2ª ed. São Paulo: Editora Santos; 1998. p. 73-113.
21. Sanderick GC, Huisken R, van der Stelt PF, Welander US, Stheeman SE. Image quality of direct digital intraoral x-ray sensors in assessing root canal length. Oral Surg Oral Med Oral Pathol. 1994;78(1):125-32. doi: 10.1016/0030- 4220(94)90128-7.
22. Haiter Neto F. Estágio atual da radiografia digital. Rev ABRO. 2000;1(3):1-6.
23. Versteeg CH, Sanderink GCH, van der Stelt PF. Efficacy of digital intra-oral radiography in clinical dentistry. J Dent. 1997;25(3- 4):215-24. doi: 10.1016/S0300-5712(96)00026-7.
24. van der Stelt PF. Filmless imaging: the uses of digital radiography in dental practice. J Am Dent Assoc. 2005;136(10):1379-87.
25. Khademi JA. Digital images & sound. J Dent Educ. 1996;60(1):41-6.
26. Bissoli CF, Takeshita WM, Melo Castilho JC, Medici Filho E, Moraes MEL. Digitalização de imagens em radiologia: uma nova visão de futuro. Rev Odonto. 2007;15(30):34-9.
27. Parks E, Williamson G. Digital radiography: an overview. J Contemp Dent Pract. 2002;3(4):23-39.
28. Pugliesi R, Andrade MLG, Stanojev Pereira MA, Pugliesi F. Neutron-induced electron radiography. Nucl Instrum Methods Phys Res. 2005;542:81-6. doi:10.1016/j.nima.2005.01.015.
 Correspondence to:
Correspondence to:
LO FERNANDES
e-mail: lua_osorio@hotmail.com
Received on: 17/1/2011
Approved on: 17/6/2011













