Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.3 Porto Alegre Jul./Set. 2012
ORIGINAL / ORIGINAL
Midazolam conscious sedation in 2-4 years old children
Sedación consciente en pacientes de 2 a 4 años con Midazolam
Rubén Alberto BAYARDO I; Martha Leslie HERRERA I; Lizangela ACEVES I
I Universidad de Guadalajara, Centro Universitario de Ciencias de la Salud, Departamento de Clínicas Odontológicas Integrales. Av. Juarez, 976, Col. Centro, C.P. 44100, Guadalajara, Jalisco, México
ABSTRACT
Objective
The purpose of this study was to assess anxiety in 2 to 4 year-old children, treated under conscious sedation with midazolam.
Methods
We evaluated 20 subjects who presented negative behavior and totally negative behavior according to Frankl scale. During the first appointment they presented a maximum of 3 teeth in need of treatment.
Results
The results showed that the study group (N=7) presented better behavior for dental care than the control group (N=13) (p<0.05). In the evaluation of heart rate and oxygen saturation, no significant differences were found between the two groups (p>0.05).
Conclusion
The behavior of patients who underwent dental treatment with restraint and under conscious sedation with midazolam remained very calm; they did not cry and anxiety was lower than in the patients who were treated without sedation. Parents in the experimental group mentioned how satisfied they were with care under sedation.
Indexing terms: Children. Conscious sedation. Midazolam.
RESUMEN
Objetivo
El objetivo del presente trabajo fue evaluar la ansiedad en niños de 2-4 años atendidos bajo sedación consciente con midazolam.
Métodos
Fueron evaluados 20 niños que presentaron comportamiento negativo y totalmente negativo de la escala de Frankl en la primera cita y que presentaran un máximo de 3 dientes con necesidad de tratamiento.
Resultados
Los resultados mostraron que el grupo de estudio (n=7) presento mejor comportamiento durante la atención odontológica que el grupo control (n=13) (p< 0.05). Sin embrago al evaluar la frecuencia cardiaca y la saturación de oxigeno en los dos grupos no hubo diferencia significativa (p> 0.05).
Conclusiones
El comportamiento de los pacientes que les fue realizado el tratamiento odontológico con restricción física bajo sedación consciente con midazolam fue mucho tranquilo, sin llanto y su ansiedad era menor a diferencia de los pacientes que se atendieron sin sedación. Los padres de familia del grupo experimental comentaron su satisfacción de la atención bajo sedación.
Palabras clave: Niño. Sedación consciente. Midazolam.
INTRODUCTION
Behavior management in children is the cornerstone that differentiates pediatric dentistry from other specialties. It also focuses on patients with special characteristics, since their cognitive development requires appropriate knowledge and training in order to provide successful dental treatment. Behavior management of pediatric patients is primarily based on the study of evolutionary development and the child's behavior and social development within the family1.
The decision to use behavior management techniques in pediatric dentistry, does not only depend on professional criteria, but also on the social validity of the intervention involving parents, patients, the legal system, social security and personnel support1-2.
When the mental state of a young child is altered, it is not possible to establish proper communication with her/him, so that some restraint techniques are used to control the children, which are becoming less and less accepted by parents and organizations in defense of children's rights1,3.
Currently the use of sedative drugs is increasingly more accepted which, in combination with the usual approach to methods and communication, allow the achievement of objectives, promote education, alleviate fear and anxiety, and establish a relationship of trust between the dentist and child2-4.
Different sedative states may be obtained with the use of drugs in pediatric patients. Light sedation (oral), sedation with nitrous oxide (N2O) (inhalation) and deep sedation (rectal, nasal or intramuscular) are alternatives to general anesthesia that may be used when clinical rehabilitation is limited to a few teeth1.
In 1998, the American Academy of Pediatric Dentistry established guidelines for the use of conscious and deep sedation and general anesthesia in pediatric patients undergoing clinical intervention. These guidelines reflect the current understanding of the appropriate monitoring of the needs and characteristics of the five functional levels of sedation and general anesthesia that can be used in pediatric patients5.
Midazolam is a popular drug for conscious sedation in pediatric dentistry and the safety and efficacy of oral and nasal midazolam in infants and children has been reported2-3,5. Midazolam is a water-soluble benzodiazepine, which is more potent than diazepam and can be administered intramuscularly, intravenously, rectally, orally and intranasally. This drug has duration of action of approximately 30 minutes. The advantage of the intranasal route is the rapid absorption, without first-pass metabolism, but it causes a burning sensation in the nasal mucosa6.
Midazolam is a widely used benzodiazepine in Pediatrics and Pediatric Dentistry due to its sedative properties that increase comfort, reduce stress and facilitate invasive diagnostic and therapeutic procedures, in addition to causing anterograde amnesia6.
In the treatment of children in Pediatric Dentistry, drug administration should not replace the different behavior management techniques, but rather, used in combination to allow the dentist to provide better care of difficult patients. One study compared intranasal midazolam with oral diazepam in 40 healthy patients aged 3-5 years without previous dental experiences. The results showed that midazolam is a good alternative for conscious sedation in Pediatric Dentistry because of its easy administration, low risk and short halflife. According to this article, oral administration may be a disadvantage due to bowel movements and the presence of gastric juices that reduce drug action7.
Overdose of benzodiazepines is manifested by excessive sleepiness, confusion, coma, hypotension and respiratory depression that can be treated with flumazenil. This drug is a competitive antagonist of the short-acting benzodiazepine receptor administered at doses of 0.2 mg IV every 15 to 60 seconds until the desired level of consciousness is achieved8.
The aim of the present study was to evaluate the behavior of pediatric patients treated under conscious sedation with midazolam administered orally.
METHODS
This study was approved by the Ethics Committee of the Specialty in Pediatric Dentistry of the University of Guadalajara (Report 2011-03). Twenty children aged between 2 and 4 participated in the study. These patients were selected because they had a negative and totally negative behavior (Frankl Scale) during the children's first appointment. The ASA physical status classification (type I, II)9 was taken into consideration. After selecting the children and explaining the research to parents or guardians, they signed a written consent.
Within the inclusion criteria, a maximum of three teeth in need of treatment for rehabilitation was required, with the intention that treatment under sedation would be performed in one session. The procedure was scheduled for the next appointment to perform the dental treatment in the experimental group (n = 7) and control group (n = 13).
In the experimental group, the patient was weighed on a scale and a pediatric anesthesiologist applied midazolam at a dose of 0.5mg/kg. The drug was mixed in a glass with 2ml of apple juice, and to enable the patient to ingest it, a needleless syringe was used to administer the mixture in the retromolar area, 10 minutes before starting treatment. During this period the patients were accompanied at all times by a parent or guardian and monitored by the anesthesiologist. At the end of 10 to 15 minutes, the child was observed to be under the effects of sedation (cheerful, calm, relaxed, sleepy).
In both groups, the patients came to the clinic accompanied by their respective mothers. Each patient was laid down in the dental chair under physical restraint and the oximeter was placed on the big toe of the right foot, to record the heart rate and oxygen saturation at the beginning, during and before completing treatment. In both groups, behavior was observed from the time the child arrived at the clinic, during the rehabilitation process, and their general behavior was assessed. Finally, the parents answered some questions about their perception of events during treatment.
RESULTS
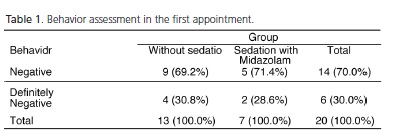
Of the 20 patients, 14 were girls (70%) and 6 boys (30%) with a mean age of 36 months. The ages ranged between 24 to 48 months. The behavior of both groups was negative and definitely negative according to Frankl scale on the first appointment (Table 1).
When assessing the vital signs of both groups with regard to the heart rate and oxygen saturation during dental treatment, it was observed that patients treated without sedation showed a higher heart rate and lower oxygenation, however, they did not differ significantly (p> 0.05).
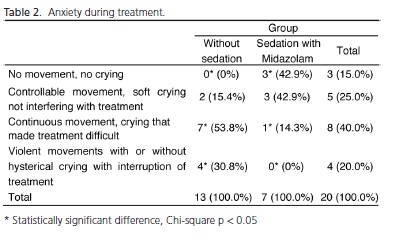
The level of anxiety before treatment after the administration of the drug was lower in the experimental group, with significant difference (p <0.05). Of the 13 children in control group, 9 were very anxious and crying (69.2%), but no children under sedation showed this behavior.
Table 2 shows that 100% of patients in the experimental group were under a sedative effect. When assessing the response of the patients during treatment, it was found that 3 out of 7 children (42.9%) in the group under sedation showed no movement or crying, but in the control group all patients were crying and moving around making treatment difficult. When comparing the groups, it was found that 85% of patients in the control group made treatment difficult against only 15% in the experimental group.
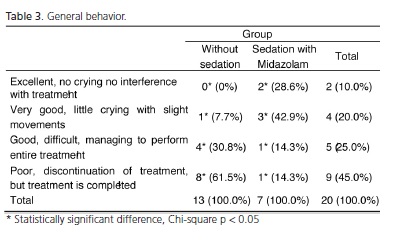
The result of the overall behavior (before, during and after treatment) is shown in Table 3, in which the behavior was shown to be statistically better in the experimental group than in the control group (p<0.05), therefore, dental treatment was successful when misbehaved patients were under sedation.
In the opinion of 57% of the mothers of patients in the experimental group, they found their children's behavior was excellent compared with previous appointments during which the anamnesis and intraoral examination was performed.
DISCUSSION
The study population has special characteristics such as being: very uncooperative, fearful and anxious. The decision to administer a sedative depends more on cooperation than on age. The behavior of the children in the experimental group showed better cooperation and treatment was facilitated, though performed under physical restraint.
In this study, with regard to the vital signs, oxygen saturation was lower and heart rate was higher in patients without sedation with no significant difference (p >0.05). These results are in agreement with those of another study in which intranasal administration was used7.
In both groups, the heart rate was above the maximum of 130 beats per minute. However, it is known that these levels can reach 170 beats per minute if the patient is crying or restless.
Previous studies2,7 have shown that midazolam induces a decrease in anxiety and its effect was more significant in children with higher levels of anxiety. A satisfactory result in behavior in this study was achieved with a dose of 0.50mg/kg, which is still considered a low dose according to the literature.
It is important to point out that the drug administered orally and diluted in apple juice was the midazolam solution of 15mg, since the tablet presentation is no longer available and it is difficult to make young children take the tablet. Although the taste is a little bitter, the oral administration of the medication is better than by the intranasal route, as this causes a burning sensation in the mucosa7.
The administration of midazolam should be performed by a trained person and the equipment needed to monitor vital signs, oxygen and resuscitation equipment must be available. Preferably the sedation procedure should be performed by a pediatric anesthesiologist.
Dental care for children under 4 years of age can be very difficult due to behavior management, so when patients do not have many affected teeth, conscious sedation is an excellent alternative for treatment.
It is noteworthy that care with physical restraint is increasingly accepted by the parents and pediatric dental treatment under sedation is becoming increasingly more accepted9. This was also observed in the present study because parents commented that they preferred care under sedation for their children.
CONCLUSION
The behavior of patients who underwent dental treatment with restraint and under conscious sedation with midazolam remained very calm; they did not cry and anxiety was lower than in the patients who were treated without sedation.
Parents in the experimental group mentioned how satisfied they were with care under sedation.
ACKNOWLEDGEMENTS
The authors thank Dr. Rogelio Troyo Sanroman for his contribution in the statistical analysis. The authors also thank Dr. Rocio Mariaud Schmid for her methodological review of the study. The authors also thank Dr. Celina Velarde Scull for monitoring sedation.
Collaborators
RA BAYARDO director of research and tutor of students. ML HERRERA and L ACEVES student's of the specialty and project participant.
REFERENCES
1. Bordoni N, Escobar A, Castillo R. Odontologia pediatrica. Buenos Aires: Medica Panamericana; 2010. [ Links ]
2. Wilson S. Pharmacological management of the pediatric dental patient. Pediatr Dent. 2004;26(2):131-6.
3. Peretz B, Zadik D. Parents attitudes toward behavior management techniques during dental treatment. Pediatr Dent. 1999;21(3):201-4.
4. Boy JR, Catalá M, Garcia BC, Mendoza A. Sedación pediátrica: odontopediatria. Barcelona: Mason; 2005.
5. Quality assurance criteria. American Academy of Pediatric Dentistry. Pediatr Dent. 1996;18(6):82-98.
6. López Av, Arroche AA, Bestrand JR, Ocaña NF. Us and misuse of benzodizepines. Medisan. 2010;13:4.
7. Lee-Kim SJ, Fadavi S, Punwani I, Koerber A. Nasal versus oral midazolam sedation for pediatric patients J Dent Child (Chic). 2004;71(2):126-30.
8. Lee J, Vann W, Roberts M. A cost analysis of treating pediatric dental patients usin general anesthesia versus conscious sedation. Pediatr Dent. 2000;22(1):27-32.
9. Keats AS. The ASA classification of physical status - a recapitulation. Anesthesiology. 1978;49(4):233-5.
 Correspondence to:
Correspondence to:
RA BAYARDO
e-mail: rubenbayardo@hotmail.com
Received on: 16/5/2012
Approved on: 11/8/2012













