Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.3 Porto Alegre Jul./Set. 2012
CLINICAL / CLÍNICO
Oral leukoplakia: malignant transformation after four years of surgical excision
Leucoplasia bucal: transformação maligna após quatro anos da excisão cirúrgica
Bárbara Mayoral Pedroso WEYLL I; Thaís Feitosa Leitão de OLIVEIRA II; Bráulio CARNEIRO JÚNIOR III; Luciana Maria Pedreira RAMALHO I
I Universidade Federal da Bahia, Faculdade de Odontologia. Rua Caetano Moura, 107, Federação, 40210-340, Salvador, BA, Brasil
II Universidade de São Paulo, Faculdade de Odontologia. Bauru, SP, Brasil
III Universidade Estadual do Sudoeste da Bahia, Faculdade de Odontologia. Jequié, BA, Brasil
ABSTRACT
Leukoplakia is the most prevalent precancerous lesion of the oral cavity, and given it is malignant potential, patients must periodically be followed up. The aim of this article was to report a clinical case a woman patient, alcohol abuser and smoker for over 25 years, who is an oral leukoplakia carrier. Histopathological examination indicated the presence of a moderate epithelial dysplasia while immunohistochemistry for Ki-67 and cyclin D1 revealed the presence of cellular proliferation in suprabasal layers. Therefore, the removal of the lesion with surgical laser was the elected treatment. Since then, the patient has been followed up for 3 years, however, after two sequential follow up absences, she returned with recurrence of the lesion, with a history of eight months progression. Histopathological examination revealed the presence of a well differentiated carcinoma.
Indexing terms: Carcinoma. Leukoplakia oral. Surgery oral.
RESUMO
A leucoplasia é a lesão cancerizável mais prevalente da boca, foi definida pela Organização Mundial de Saúde como mancha ou placa branca, que não se caracterizada como outra lesão bucal. Devido ao seu potencial de malignização, os pacientes com leucoplasias devem ser acompanhados periodicamente. O objetivo desde artigo é relatar o caso de uma paciente do gênero feminino, etilista e tabagista há mais de 25 anos com leucoplasia bucal. O exame histopatológico indicou a presença de displasia epitelial moderada e a imunomarcação pelo Ki-67 e ciclina D1 revelou a presença de proliferação celular em camadas suprabasais. Por essa razão, optou-se pela remoção da lesão com o laser cirúrgico. A paciente permaneceu em acompanhamento semestral por três anos, entretanto, após faltar a duas revisões, retornou com recidiva da lesão com história de evolução de oito meses e cujo exame histopatológico revelou a presença de carcinoma espinocelular bem diferenciado.
Termos de indexação: Carcinoma. Leucoplasia bucal. Cirurgia bucal.
INTRODUCTION
Leukoplakia is the most common cancerous lesion of the oral cavity, and was defined by the World Health Organization (WHO) in 1978, as a white lesion that cannot not clinically or pathologically be characterized as any other disease1-3. Its diagnosis is clinical and is obtained by exclusion of other lesions4-5.
The choice of treatment must be based on the natural history of the disease and its characteristics6. Various treatments may be used for leukoplakic lesions: surgical excision by means of cryosurgery, CO2 laser and eletrocoagulation5-6, photodynamic therapy, or the use of medication therapy with licopene7-12.
However, complete removal of the lesion alone, does not guarantee cure, because studies have demonstrated the possibility of leukoplakia recurrence even when it has been excised, and in some cases, recurrence as carcinoma. This characteristic may be verified with greater frequency when the lesion is located in the floor of the mouth8-12. For this reason, the patient with leukoplakia must be periodically followed up, in order to prevent the appearance and progression of the more aggressive behavior of leukoplakia.
CASE REPORT
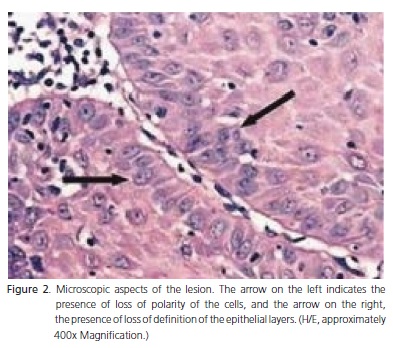
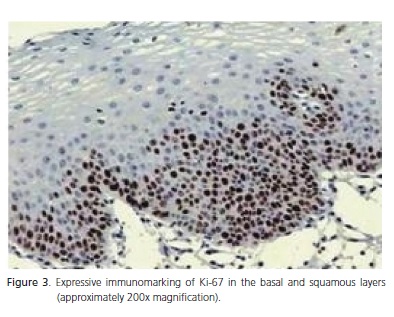
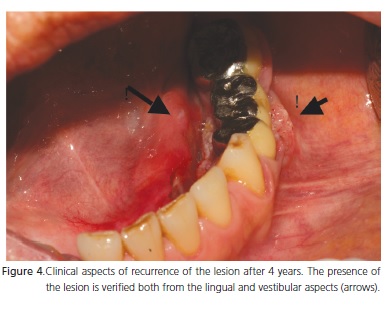
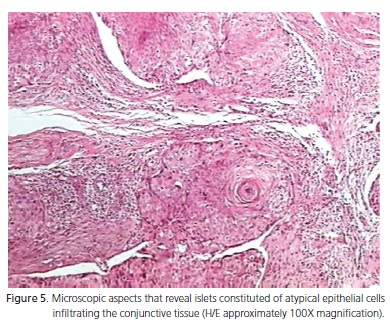
The patient, H.S., a 54-year-old woman, alcohol abuser and smoker for over 25 years, was referred to the Stomatology Service in the year 2002. The physical exam revealed the presence of a homogeneous, non scrapable, asymptomatic white lesion in the floor of the mouth, with progression of one year (Figure 1). The clinical diagnosis was oral leukoplakia. Toluidine blue was applied on the lesion and the area positive to the stain was elected for performing the incisional biopsy. The histopathological result indicated the presence of epithelial hyperplasia associated with moderate dysplasia (Figure 2). Immunomarking with Ki-67 and cyclin D1 revealed expressive presence of cellular proliferation in suprabasal layers (Figure 3). For this reason, the option taken was to perform complete removal of the lesion with surgical CO2 laser. In the following years the patient was periodically followed up, however, when she returned in 2006, after missing the two previous six-monthly evaluations, the patient reported burning in the region of the left mandibular alveolar ridge, with progression of eight months. Thus, a white lesion with an erythematous halo, suggestive of leukoplakia was observed, close to the fixed dental prosthesis, at the same site from which the lesion had been removed. (Figure 4). The lesion was therefore again stained with toluidine blue, and an incisional biopsy performed where the marking was positive. The histopathological report affirmed that it was a well differentiated squamous cell carcinoma (Figure 5). As no medication therapy was performed at any stage of follow up, after the histopathological report the patient was referred to the head and neck surgeon for oncological treatment.
It is important to point out that the patient had signed a term of free and informed consent of the Stomatology course, at the Federal University of Bahia, and therefore the authors are authorized to publish the case.

DISCUSSION
Due to leucoplakia being a relatively common lesion, corresponding to 85% of lesions that may become cancerous12-15, early diagnosis and treatment must be performed in order to minimize or prevent the malignant transformation that occurs in some cases16-18,. With regard to the patient, in the first instance, the option was to perform complete removal of the lesion with CO2 laser, due to the presence of moderate dysplasia. In a prospective study conducted by van der Hem6 in patients with leukoplakia treated with CO2 laser, low recurrence of the lesion was verified after 219 months, and in only 3 cases presented was there malignant transformation, 2 of which were in the floor of the mouth.
Malignization of the lesion in the reported case, eight months after the first surgical removal may be related to the phenomenon of field cancerization, the localization and biologic behavior of the lesion and strong relationship of smoking and alcohol abuse with oral cancer9,15. According to Bánóczy et al.17 and Roosaar et al.18, it is possible for regression of leukoplakia to occur after discontinuing the use of tobacco17. The smoking habit must be abolished with the purpose of diminishing the risk of development of the cancer19. An attempt was made to make the patient aware of the need to eliminate the associated factors such as tobacco use, but without success.
Jaber et al.20 in a study to determine the clinical pattern and natural history of lesions diagnosed as being epithelial dysplasias in patients resident in the United Kingdom, verified that severe epithelial dysplasias were more associated with lesions in the floor of the mouth and edge of the tongue, whereas mild epithelial dysplasia was more related to lesions in the oral mucosa. The majority of white lesions (43.8%) were characterized by the presence of mild epithelial dysplasia, however 30% presented evidence of moderate dysplasia and 24.7% severe dysplasia21.
In this context, the use of toluidine blue in the follow-up of cancerizable lesions is routine at our clinic and was of fundamental help to locate the site of the biopsy. In addition, the positive staining was compatible with the presence of cell proliferation, both in the case of moderate epithelial dysplasia and in the presence of squamous cell carcinoma. It is known that malignant or atypical cells present a larger genetic material content, and as toluidine blue dye has an affinity for nuclear material with a high DNA or RNA content, areas that present these alterations have the capacity to retain a larger quantity of the dye22-23. A study conducted by Gandolfo et al.24 verified that the strong staining of the test with toluidine blue demonstrated a true-positive result and showed that the dye intensity was related to the severity of the lesion.
In spite of the indices suggesting that the more aggressive clinical aspects and histopathological patterns with a higher degree of dysplasia are indicative of greater possibility of malignant transformation, these morphological aspects are insufficient for predicting this event. The advancements in molecular biology and genetics have allowed the identification of markers, which probably are more reliable for predicting the biological behavior of the lesion16.
There is a constant search for reliable markers that are capable of predicting malignancy in cancerizable lesions25. Among the methods for evaluating the biologic behavior of dysplastic and neoplastic lesions, is the use of immunohistochemical markers that make it possible to analyze the antigens expressed by tumoral and stromal cells. With the use of this technique it is possible to evaluate the tumor growth fraction with the use of cell proliferation markers such as Ki-67 and Cyclin D126.
In the clinical case in question, there was strong immunomarking for cyclin D1 and Ki-67. Studies have demonstrated that the expression of Cyclin D1 increases parallel to the severity of the leukoplakia25 and this same relationship may also be verified with regard to Ki-67, in which significant differences have been observed between the immunomarking of keratinocytes without atypias, epithelium with mild, moderate and severe dysplasias, and in cases of carcinomas in situ and microinvasive carcinomas27-28. Perhaps, as a result of these findings, in the literature Ki-67 is considered the best cell proliferation marker at present29.
The degrees of dysplasia vary from mild to severe, lesions with a greater degree of dysplasia are related to higher malignization potential. The presence of epithelial dysplasia is usually accepted as an important prognostic factor for the malignization of cancerizable lesions. Nevertheless, lesions with dysplasia do not necessarily develop into cancer30.
CONCLUSION
From the clinical case reported, the importance of periodical follow up of cancerizable lesions, even after their complete removal, may be verified. In this context, toluidine blue is outstanding as an auxiliary instrument in the follow up of leukoplakias and in the choice of the biopsy site, and so are the cell proliferation markers, for evaluating the biologic behavior of these lesions.
Collaborators
BMP WEYLL followed-up the patient, conducted the literature review, and wrote the article. TFL OLIVEIRA participated in writing and correcting the article, and assisted the surgeon with the biopsy. B CARNEIRO JÚNIOR was responsible for the biopsy and initial follow-up of the patient, and also participated in writing the article. LMP RAMALHO was the pathologist responsible for the biopsies, and participated in writing the article.
REFERENCES
1. Rodrigues TLC, Lino JS, Sampaio MCC, Rodrigues FG, Costa ALL. Leucoplasias bucais: relação clínico-histopatológica. Pesqui Odontol Bras. 2000;14(4):357-61. doi: 10.1590/S1517- 74912000000400009. [ Links ]
2. Gabriel JG, Cherubini K, Yurgel LS, Figueredo MAZ. Considerações gerais e abordagem clínica da leucoplasia. Rev Bras Patol Oral. 2004;3(4):187-94.
3. Silva ICO, Carvalho ATD, Silva LBO, Nagahama MCVFB. Leucoplasia: uma revisão de literatura. RGO - Rev Gaúcha Odontol. 2007;55(3):287-9.
4. Femiano F, Gombos F, Scully C, Battista C, Belnome G, Esposito V. Oral leukoplakia: open trial of topical therapy with calcipotriol compared with tretinoin. Int J Oral Maxillifac Surg. 2001;30(5):402-6. doi: 10.1054/ijom.2001.0107.
5. Ishii J, Fujita K, Komori T. Laser surgery as a treatment for oral leukoplakia. Oral Oncol. 2003;39(8):759-69. doi: 10.1016/ S1368-8375(03)00043-5.
6. van der Hem P, Nauta JM, van der Wal JE, Roodenburg JL. The results of CO2 laser surgery in patients with oral leukoplakia: 25 year follow up. Oral Oncol. 2005;41(1):31-37. doi: 10.1016/j. oraloncology.2004.06.010.
7. Sieron A, Adamek M, Kawczyk-Krupka A, Mazur S, Ilewicz L. Photodynamic therapy (PDT) using topically applied deltaaminolevulinic acid (ALA) for the treatment of oral leukoplakia. J Oral Pathol Med. 2003;32(6):330-6. doi: 10.1034/j.1600- 0714.2003.00068.x.
8. Lodi G, Sadella A, Bez C, Demaosi F, Carrassi A. Systematic review of randomized trials for the treatment of oral leukoplakia. J Dent Educ. 2002;66(8):896-902.
9. Singh M, Krishanappa R, Bagewadi A, Keluskar V. Efficacy of oral lycopene in the treatment of oral leukoplakia. Oral Oncol. 2004;40(6):591-6. doi: 10.1016/j.oraloncology.2003.12.011.
10. Góes C, Weyll B, Sarmento VA, Ramalho LMP. Diagnóstico diferencial e manejo da leucoplasia bucal - caso clínico: acompanhamento de 4 anos. RGO - Rev Gaúcha Odontol. 2007;55(1):95-100.
11. Dinis Freitas M, Blanco-Carrion A, Gandara-Vila P, Antunez- Lopez J, Garcia-Garcia A, Gandara Rey JM. Clinicopathologic aspects of oral leukoplakia in smokers and nonsmokers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(2):199- 203. doi: 10.1016/j.tripleo.2005.12.009.
12. Bsoul SA, Huber MA, Terezhalmy GT. Squamous cell carcinoma of the oral tissues: a comprehensive review for oral healthcare providers. J Contemp Dent Pract. 2005;6(4):1-16.
13. Saito T, Sugiura C, Hirai A, Notani K, Totsuka Y, Shindoh M, et al. Development of squamous cell carcinoma from pre-existent oral leukoplakia: with respect to treatment modality. Int J Oral Maxillofac Surg. 2001;30(1):49-53.
14. Petti S. Pooled estimate of world leukoplakia prevalence: a systematic review. Oral Oncol. 2003;39(8):770-80. doi: 10.1016/ S1368-8375(03)00102-7.
15. Chandu A, Smith AC. The use of CO2 laser in the treatment of oral white patches: outcomes and factors affecting recurrence. Int J Oral Maxillofac Surg. 2005;34(4):396-400. doi: 10.1016/j. ijom.2004.10.003.
16. Jayatilake JAMS, Samaranayake YH, Cheung LK, Samaranayake LP. Quantitative evaluation of tissue invasion by wild type, hyphal and SAP mutans of Candida albicans, and non-albicans Cândida species in reconstituted human oral epithelium. J Oral Pathol Med. 2006;35(8):484-91. doi: 10.1111/j.1600- 0714.2006.00435.x.
17. Bánóczy J, Gintner Z, Dombi C. Tobacco use and oral leukoplakia. J Dent Educ. 2001;65(4):322-7.
18. Roosaar A, Yin L, Johansson AL, Sandborgh-Englund G, Nyren O, Axell T. A long-term follow - up study on the natural course of oral leukoplakia in Swedish population-based sample. J Oral Pathol Med. 2007;36(2):78-82. doi: 10.1111/j.1600- 0714.2007.00501.x.
19. Poate TWJ, Warnakulasuriya S. Effective management of smoking in an oral dysplasia clinic in London. Oral Dis. 2006;12(1):22-6. doi: 10.1111/j.1601-0825.2005.01146.x.
20. Jaber MA, Porter SR, Speight P, Eveson JW, Scully C. Oral epithelial dysplasia: clinical characteristics of western European residents. Oral Oncol. 2003;39(6): 589-96. doi: 10.1016/S1368- 8375(03)00045-9.
21. Hsue SS, Wang WC, Chen CH, Lin CC, Chen YK, Lin LM. Malignant transformation in 1458 patients with potentially malignant oral mucosal disorders: a follow -up study based in a Taiwanese hospital. J Oral Pathol Med. 2007;36(1):25-9. doi: 10.1111/j.1600-0714.2006.00491.x.
22. Martin IC, Kerawala CJ, Reed M. The application of toluidine blue as a diagnostic adjunct in the detection of epithelial dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(4):444-6. doi: 10.1016/S1079-2104(98)90071-3.
23. Onofre MA, Posto MR, Navarro CM. Reability of toluidine blue application in the detection or oral epithelial dysplasia and in situ and invasive squamous cell carcinomas. Oral Surg Oral Med Oral Pathol Oral Endod. 2001;91(5):535-40. doi: 10.1067/ moe.2001.112949.
24. Gandolfo S, Pentenero M, Broccoletti R, Pagano M, Carozzo M, Scully C. Toluidine blue uptake in potentially malignant oral lesions in vivo: clinical and histological assessment. Oral Oncol. 2006;42(1):89-95. doi: 10.1016/j.oraloncology.2005.06.016.
25. Femiano F, Scully C. DNA cytometry of oral leukoplakia and oral lichen planus. Med Oral Patol Oral Cir Bucal. 2005;(10):9-14.
26. Ramalho LMP, Yurgel LS, Machado DC, Sant´Ana-Filho M. Expressão Imuno-histoquímica da ciclina D1, Ki-67 e PCNA em carcinomas espinocelulares de boca: análise comparativa da zona central e da zona de invasão tumoral. Rev Odonto Ciência. 2000;15(31):71-86.
27. Kovesi G, Szende B. Prognostic value of ciclin D1, p 27 and p 63 in oral leukoplakia. J Oral Pathol Med. 2006;35(5):274-7. doi: 10.1111/j.1600-0714.2006.00396.x.
28. Korokawa H, Matsumoto S, Murata T, Yamashita Y, Tomoyose T, Zhang M, et al. Immunohistochemical study of syndecan -1 down - regulation and the expression of p53 protein or Ki-67 antingen in oral leukoplakia with or without epithelial dysplasia. J. Oral Pathol Med. 2003;32(9):513-21. doi: 10.1034/j.1600- 0714.2003.00117.x.
29. Santos-Garcia AS, Abad-Hernandez MM, Fonseca-Sanchez E, Cruz-Hernandez JJ, Bullon-Sopelana A. Proteic expression of p53 and cellular proliferation in oral leukoplakias. Oral Surg Oral Med Oral Pathol. 2005;10(5):1-8.
30. Reibel J. Prognosis of oral pre-malignant lesions: significance of clinical, histopathological, and molecular biological characteristics. Crit Rev Oral Biol Med. 2003;14(1):47-62. doi: 10.1177/154411130301400105.
 Correspondence to:
Correspondence to:
BMP WEYLL
e-mail: binhaweyel@yahoo.com.br
Received on: 14/6/2010
Final version resubmitted on: 25/11/2010
Approved on: 15/1/2011













