Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 no.4 Porto Alegre Out./Dez. 2012
CLÍNICO / CLINICAL
Peri-implant esthetics through gingival conditioning
Estética perimplantar por meio de condicionamento gengival
Patrícia Lins Azevedo do NASCIMENTO I; Daniella Neves da ROCHA I; João Batista Oliveira MAIA I; Lucy COIMBRA I; Alexandre Henrique de Moura DIAS I
I Universidade Potiguar, Faculdade de Odontologia. Natal, RN, Brasil
ABSTRACT
In most cases, oral rehabilitation using implants provides esthetic excellence and consequently an improvement in the quality of life so cherished by edentulous patients. When there is interproximal papilla loss, this rehabilitation becomes difficult to achieve. To solve this problem, it is possible to use the gingival conditioning technique. This consists of rebuilding provisional crowns with acrylic resin during the phases of surgical healing through to the application of gradual pressure, leading to gingival papilla formation. The aim of this research was to show, by way of a clinical case, the esthetic possibilities obtained through gingival conditioning via the rebuilding of the provisional crown on the implant. It may be concluded that the gingival conditioning technique which uses gradual rebuilding of the temporary crown is simple, easily accomplished and particularly effective in the restoration of esthetics in implant rehabilitation, provided that patients can maintain correct oral hygiene and plaque control.
Indexing terms: Esthetics dental. Gingiva. Mouth rehabilitation.
RESUMO
As reabilitações orais por meio de implantes dentais permitem na grande maioria dos casos, a excelência estética e consequentemente o melhoramento na qualidade de vida tão almejada por parte dos pacientes edêntulos. Quando há perda de papila interproximal, essa reabilitação se torna dificultada. Para solucionar esse problema, podemos utilizar a técnica do condicionamento gengival. Esta consiste no reembasamento da coroa provisória com resina acrílica durante a fase de cicatrização cirúrgica, por meio de uma pressão gradual, levando à formação de papila gengival. Este trabalho tem como objetivo apresentar, através de caso clínico, o alcance estético obtido através de condicionamento gengival pela técnica de reembasamento do provisório sobre implante. Conclui-se que, a técnica de condicionamento gengival por meio de reembasamento gradativo do provisório é simples, fácil de ser executada e bastante eficiente no restabelecimento da estética em reabilitações com implantes, desde que o paciente mantenha uma correta higienização e controle de placa.
Termos de indexação: Estética dentária. Gengiva. Reabilitação bucal.
INTRODUCTION
Within modern day culture, the influence of and prioritization given to esthetics by society have been notable, giving rise to more anxious, demanding patients looking to find rejuvenation and beauty in the dental surgeries1. As a solution to some of these esthetic problems, osseointegrated implants have introduced a new dimension in the restoration of lost teeth, providing positive longitudinal results for a large number of patients2.
Many parameters have been studied, aiming to endorse the esthetics of peri-implant tissue. Prior to commencing treatment, it is necessary to plan well and, if necessary, intervene in the tooth while still in the cavity so that the hard and soft tissue is maintained and/or acquired in the initial phases, guaranteeing both esthetic success and the health of this tissue3.
Gomes4 alerted us to the challenge of unitary implants, primarily in terms of the observation of all the details of the architecture of the ridge, such as: bone volume in height and thickness, presence of interproximal crest, height and thickness of the keratinized mucous, adequate interproximal and inter-occlusal space, smile line and interproximal papillae. The authors also believed that, of all these requirements, the main challenge is the reconstruction of the lost interproximal papillae.
Parreira & Santos5 conceptualized the gingival papillae as being the healthy tissue that occupies the area below the proximal contact, being a part of the tooth contour.
The inter-implant distance at the level of the bone crest results in implants with only a small space between each other experiencing greater bone loss, and these losses could have an impact on the formation of the papilla between them1. This can happen when the implants are situated less than 3 mm from each other6.
According to Biggs & Litvak7, patients subjected to implants should have gingival tissue that has a natural, healthy appearance. However, despite the fact that implantology presents excellent clinical results, if there is no bone crest present, the restoration of the gingival contour is adversely affected. According to Tarnow et al.8, the distance between the bone crest and the point of contact is a determining factor in the presence, or otherwise, of interproximal papilla. The longevity of dental implants depends on the integration of implant with the bone and mucous tissue2.
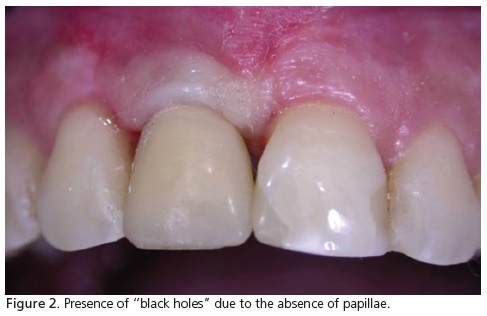
Tooth loss brings with it a series of deformations that must be evaluated as to the amount of bone loss and the subsequent gingival alteration, as well as the absence of the interdental papilla, which is extremely important, not only for the restoration of a more natural gingival contour, eliminating the so-called "black holes", but also for phonetics and for this reason, this tissue should be part of the prosthetic planning1,9-10.
According to Ottoni & Maiolini3, the loss of interdental tissue occurs as a result of the following: injury; tooth extraction; congenital defects; incorrect brushing; iatrogenic restorations; conventional resective surgery; spaced dentition; chronic or aggressive periodontal disease or bad implant planning.
The presence of keratinized gums is not a fundamental prerequisite for the survival of osseointegrated implants, however their presence does hold the following advantages: the gingival margin remains more constant and resistant to recession; better esthetics; helps with dental hygiene; easier surgical manipulation; facilitates the molding process and avoids the buildup of bacterial plaque by protecting the periodontal tissue from infection and the impaction of food remains5,11-13 .
Alconforado14 and Groisman & Júnior15 alerted us to the fact that it is not only osseointegration that has to be observed in the surgical insertion of implants, as even with osseointegration, success may not be achieved if the implant is badly placed. When badly placed, this could make rehabilitation impossible or render esthetic reconstruction unviable. Moreover, a poorly selected diagnosis of the condition of future, soft peri-implant tissues could lead to the esthetic failure of any rehabilitation.
Gingival conditioning aims to improve the format of the residual ridge in height and thickness, providing suitable space and design for the emergency profile of the bridge to be inserted in that location16.
According to Franciscone & Vasconcelos17, the progressive growth of the cervical contour of the temporary restoration permits the gingival orientation towards esthetic optimization, with the subsequent shaping of the concave gingival arch.
Pegoraro18 stressed that gingival conditioning should satisfy some of the requirements: correct dental hygiene of the area to be conditioned; gingival tissue of a thickness sufficient to permit conditioning; conditioned area with no ulceration after conditioning; decision on a temporary prosthesis in a form desirable to the papillae. This author highlighted the importance of the handling of the temporary prosthesis via the Nealon technique, by way of gradual rebuilding using acrylic resin so as to permit gum contouring and stimulate the formation of gingival papillae on the fixed prostheses. When used in implantology, this technique facilitates esthetic optimization, principally in the anterior region in patients with gingival smiles16,19-20.
Jiménez-Lópes21 stressed that a perfect fit of the crown should be sought on the temporary component giving a vestibular shape to it which is most similar to the adjacent tooth, so that the soft tissue may acquire, during the healing process, an esthetic shape that is acceptable as the end result.
Onno et al.22 argued for the need to intervene prior to the creation of the definitive prosthesis in order to promote a significant quantity of keratinized gingival tissue. Muco-gingival problems seem to prefer places where the alveolar bone is not very thick on the vestibular and lingual sides of the implant, and where there is little in the way of keratinized gums. At least 5 mm of gum is desirable for the insertion of implants since in natural teeth, inflammation frequently occurs when the restoration is subgingival.
As far as Edelhoff et al.23 are concerned, the rebuilding of temporary to long-term restorations plays an important role, determining the area of contact of the temporary prosthesis and the remodeling of the receiving gum. The authors also argued for the use of low viscosity flow resin applied to the temporary prosthesis in small, photopolymerized increments, providing a better tissue response with compound resin in contrast to acrylic resin.
Morais et al.24 stated that non-surgical gingival conditioning could be performed prior to the reopening, or afterwards with the temporary prosthesis inserted on the implant. In the case reported by the authors, gingival conditioning was performed prior to the occasion of the second surgery, where the entire gingival tissue present above the level of the implant underwent compression, prematurely reestablishing the emergency profile and eliminating the need to open the implant, which could give rise to a loss of tissue or contraction of the gingival margin.
For Machado et al.25, the rebasing of the temporary prosthesis is necessary for the adaptation of the conjunctive tissue to the new situation and this temporary prosthesis should remain in place for a minimum of 60 days for subsequent definitive molding, as this period of time is necessary for carrying out the modification of the conjunctive tissue thereby avoiding subsequent alterations to the definitive molding in the shape and contour of the conditioned ridge.
The aim of this study is to show, through a clinical case, the esthetic range achieved with the use of gingival conditioning using the technique of rebuilding the temporary prosthesis on to the implant.
CASE REPORT
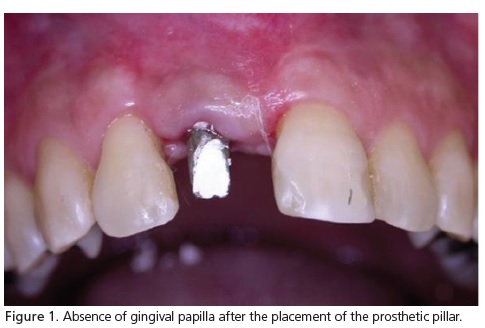
Patient NVC, female, aged 42, turned up at the prosthetic department of the Faculty of Dentistry at the University of Potiguar, reporting a fracture of element 11. Due to the condition of the aforementioned element, the option was taken to rehabilitate with an implant and In- Ceram ceramic crown. The extraction of the element was performed and bone graft removed en bloc from the area of the mandible. The titanium implant was inserted after three months and then there was a six month wait for osseointegration (Figure 1).
As there was loss of the gingival papilla, in order to reestablish the esthetic, conditioning was done using the temporary prosthesis rebuilt with acrylic resin every fifteen days (Figures 2 and 3).
Following gingival conditioning, the peri-implant appearance obtained was quite favorable. The patient used the temporary crown over the implant in element 11 for three months and during this period received whitening of the neighboring teeth and lower arch. Her gingival health was monitored during the entire period of conditioning (Figures 4 and 5).
After the gingival conditioning, an In-Ceram crown was inserted on the aforementioned element (Figure 6).
For the purposes of carrying out the clinical procedures, all the ethical principles contained in the Helsinki declaration (2000) were observed, as well as compliance with specific country legislation.




DISCUSSION
Ottoni & Maiolini3 and Gomes4 stated that, to achieve satisfactory, esthetic results working with a prosthesis over the implant in the anterior region, it is important to perform a three-dimensional analysis of the correct positioning of the implant, as well as the relationship with the basal bone and soft tissue in the region to be rehabilitated. The understanding of the importance of the papilla to the red esthetic is vital to the avoidance of the appearance of black holes. Groisman & Júnior15, corroborating the above statements, also warned that the top of the implant should be positioned 3 mm from the gingival margin, in an apical direction, and that the maximum diameter of the implant should not encroach upon the minimum space of 2 mm between tooth and implant. In other words, the optimal final dental position in the initial stage of treatment is fundamental and this should be clinically ascertained as it represents a reference, a baseline for determining the required reconstruction of the hard and soft tissue11. Based on this information, the present study links the esthetic outcome to the correct positioning of the implant and to the presence of marginal bone crest.
Alveolar bone reabsorption, accompanied by gingival contours, is one of the biggest difficulties creating obstacles to the reconstruction of teeth with prostheses on osseointegrated implants. To minimize these difficulties, Adell et al.2 and Morais et al.24 agreed that planning, when well-founded on a correct diagnosis of the tissue condition in the area that is to receive the implants, mainly the esthetic areas, is essential to the success of the rehabilitation. Considering that an insufficient quantity of bone may have repercussions for the improper positioning of the implant, interfering with the gingival esthetic, producing a different appearance to that of the adjacent tooth and if the bone and gingival tissue deficiency is not corrected using regenerative techniques, the dental prosthesis will appear long and possess over-contouring of the gums3. Because of bone reabsorption arising from traumatic extractions or atrophies, bone grafts seem to provide favorable conditions for peri-implant esthetics, a fact confirmed by this study.
Oliveira et al.1, Azevedo et al.10 and Pegoraro18 stated that bone defects are just relative contraindications and may be corrected using grafts, prior to the planning of the gingival conditioning. Gradual pressure should be exerted to prevent ulcerations or gum retraction from occurring. Ottoni & Maiolini3, Azevedo et al.10 and Pegoraro18 argued for the use of slow pressure and the need for several clinical sessions in order to achieve satisfactory gingival conditioning, but this manipulation of the soft tissue for papilla formation should only be performed in the second surgical stage, since if it is carried out in the first stage, it could lead to the total, or at least partial, destruction of the gingival papilla1,3,11,14. In the present study, it was noted that, despite the clinical time spent on rebuilding sessions, the use of gradual pressure is necessary when carrying out gingival conditioning by means of temporary prostheses. The rebuilding of the bridge with acrylic resin, using the Nealon technique for the conditioning of soft tissue, is recommended as being particularly effective1,12,14-16,18-19. As for Edelhoff et al.23 and Groismann & Vidigal6, they recommended the use of photopolymerizable resin for the rebuilding of the temporary prosthesis for the formation of gingival papillae. The patient used the temporary crown for a period of 90 days, a posture which is corroborated by Neves9 and Machado et al.25, who advocated that the temporary prosthesis should remain in place for at least 60 days, before the definitive molding. The temporary crown should be rebuilt every 15 days so that a gradual pressure can be exerted on the formation of the gingival papilla, as argued by Pegoraro18 and Miraglia et al.19. This fact was also observed in this study, in which there was evidence of a good gingival appearance.
Pegoraro18 stated that gingival conditioning may be carried out through pressure of the bridges and by using diamond drill bits; Oliveira et al.1 are in agreement; both assume that the use of gradual pressure, being a non-surgical procedure which is minimally invasive and also reversible, should be preferred over scarification. Although there are differences of opinion, the fact is that gradual gingival conditioning, besides being reversible, is more efficient and gives a particularly satisfactory esthetic appearance to the gums.
CONCLUSION
The technique of gingival conditioning is simple, easy to perform and particularly effective in reestablishing red esthetic excellence in rehabilitation using implants. The rebuilding of the temporary prosthesis should be gradual in order to maintain health and provide suitable gingival conditioning. The patient's cooperation with regard to hygiene and the control of plaque is essential to achieving a successful treatment.
Collaborators
PLA NASCIMENTO was responsible for carrying out the reported treatment, bibliographical survey and composition of the article. DN ROCHA was responsible for the bibliographical survey and composition of the article. JBO MAIA was responsible for the spell-checking and composition of the article. L COIMBRA assisted with the performance of the reported treatment and took part in the composition of the article. AHM Dias directed the study and took part in the composition of the article.
REFERENCES
1. Oliveira JA, Ribeiro EDP, Conti PCR, Valle AL, Pegoraro LF. Condicionamento gengival: estética em tecidos moles. Rev Fac Odontol Bauru. 2002;10(2):99-104. [ Links ]
2. Adell R, Eriksson B, Lekholm V. A long term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants. 1990;5(4):347-59.
3. Ottoni, J, Maiolini, MTM. Estética em implantes. In: Ottoni J, Magalhães LF. Cirurgia plástica periodontal e periimplantar: beleza com proporção e harmonia. São Paulo: Artes Médicas; 2006. p. 355-70.
4. Gomes JC. Estética em clínica odontológica. Curitiba: Editora Maio; 2004.
5. Parreira GG, Santos LM. Cerâmicas odontológicas: conceitos e técnicas. São Paulo: Santos; 2005.
6. Groisman M, Vidigal Júnior GM. Tipos de superficies de implantes. In: Almeida RV. Implantodontia: a atuação clínica baseada em evidências científicas. São Paulo: Artes Médicas; 2005. p. 39-52.
7. Biggs WF, Litvak Jr AL. Immediate provisional restorations to aid in gingival healing and optimal contours for implant patients. J Prosthet Dent. 2001;86(2):177-80. doi: 10.1067/ mpr.2001.116683.
8. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal papillae. J Periodontol. 1992;63(12):995-6.
9. Neves JB. Implantodontia oral: otimização da estética - Uma abordagem dos tecidos mole e duro. São Paulo: Centro de Odontologia Integrada; 2001.
10. Azevedo SAB, Pires AA, Lange Jr. MRL. Condicionamento gengival através da técnica da pressão gradual, aplicado à otimização da estética em prótese parcial fixa: relato de caso clínico. Rev Naval de Odontol. 2004;17-21.
11. Scarso Filho JS, Barreto M, Tunes UR. Estética dos tecidos moles em implantodontia. In: Tunes UR. Atualização em periodontia e implantodontia. São Paulo: Artes Médicas; 1999. p. 319-69.
12. Rosa JCM. Manutenção da altura da margem gengival e das papilas interdentais para a implantodontia. Rev Catar Implant Florianópolis Clininplante, Estudos e Pesquisa. 2001;2(2):2-5.
13. Neves JB. Manipulação dos tecidos moles em implantodontia. In: Francischone CE, Nary Filho H, Matos DAD. Osseointegração e o tratamento multidisciplinar. São Paulo: Santos; 2006. p. 251-86.
14. Alconforado G. Tecidos perimplantares: conseqüências estéticas das diversas abordagens cirúrgicas. Portugal Implantologia. 2002;(1):9-10.
15. Groisman M, Júnior GMV. Estética perimplantar. In: Querido MRM, FAN YL. Implantes osseointegrados: inovando soluções. São Paulo: Artes Médicas; 2004. p. 37-56.
16. Zavanelli AC, Dekon SFC, Zavanelli RA, Mazaro JVQ, Nepomuceno VC, Fernandes AUR. Condicionamento gengival. PCL: Rev Ibero-am Protese Clin Lab. 2004;6(32):357-63.
17. Francischone CE, Vasconcelos LW. Osseointegração e as próteses unitárias: como otimizar a estética. São Paulo: Artes Médicas; 1998.
18. Pegoraro LF. Coroas provisórias. In: Pegoraro LF, Valle AL, Araujo CRP. Prótese fixa. São Paulo: Artes Médicas; 1998. p. 111-48.
19. Miraglia SS, Nogueira RP, Batista JG. Condicionamento gengival, estética periodontal e fonética. PCL: Rev Ibero-am Protese Clin Lab. 2000;2(10):44-8.
20. Rosa DM, Zardo CM, Neto JS. Odontologia estética e a prótese fixa dentogengival. São Paulo: Artes Médicas; 2003. p. 91-121.
21. Jiménez-Lópes V. Reabilitação bucal em prótese sobre implantes. São Paulo: Quintessence; 2000. p. 21-52.
22. Ono Y, Nevins M, Cappetta EG. A importância do tecido ceratinizado para os implantes. In: Nevins M, Mellonig JT. Implantoterapia: abordagens clínicas e evidências de sucesso. São Paulo: Quintessence; 2003. p. 227-38.
23. Edelhoff D, Spiekermann H, Yildirim M. A review of esthetic pontic options. Quintessence Int. 2002;33(10):736-46.
24. Morais JAND. Obtenção de estética em próteses sobre implantes osseointegrados: caso clínico. RBP Rev Bras Implantodont Protese Implant. 2003;10(39):210-4.
25. Machado WAS, Machado Junior DZ, Silva Junior JA, Kahn S. Aumento de coroa clínica com condicionamento de rebordo e reconstrução da papila interdental. RGO - Rev Gaúcha Odontol. 2005;53(2):113-6.
 Correspondence to:
Correspondence to:
PLA NASCIMENTO
e-mail: patricialanascimento@hotmail.com
Received on: 25/7/2008
Final version resubmitted on: 5/3/2009
Approved on: 14/4/2009













