Services on Demand
Article
Related links
Share
RGO.Revista Gaúcha de Odontologia (Online)
On-line version ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.60 n.4 Porto Alegre Oct./Dec. 2012
CLÍNICO / CLINICAL
Should an asymptomatic unerupted mandibular molar be removed?
Um dente incluso assintomático deve ser removido?
Evandro Neves ABDO I; Marcelo Drummond NAVES I; Maria Cássia Ferreira de AGUIAR I; Ricardo Alves MESQUITA I
I Universidade Federal de Minas Gerais, Faculdade de Odontologia. Belo Horizonte, MG, Brasil
ABSTRACT
The purpose of this paper is to present a clinical case of a dentigerous cyst and to discuss the need to remove the asymptomatic, unerupted teeth. A 58-year-old white woman presented for removal of an asymptomatic unerupted left mandibular second molar. A periapical radiograph revealed a horizontal intra-alveolar unerupted second molar and the absence of the third molar. The second molar had a follicular space of less than 0.5 mm. The age of the patient, the absence of symptoms and the risk of losing the first molar during the surgery were sufficient for the patient to choose to undergo periodic checkups. In the 2nd year of checkups, the development was noted of a dentigerous cyst in the second molar. The dental surgeons must assess the risks involved in putting off surgery, the benefits to the patient and be aware of the need for periodic checkups at short intervals of time in cases of non-removal of the unerupted teeth. Also, it is important to be aware that it is not possible to predict whether or not certain pathologies might occur if they are not removed.
Indexing terms: Dentigerous cyst. Surgery oral. Unerupted tooth.
RESUMO
O caso clínico de um cisto dentígero e a discussão da necessidade de se remover ou não um dente incluso assintomático são apresentados. Uma paciente de 58 anos de idade apresentou-se para a remoção de um segundo molar inferior incluso, assintomático. Uma radiografia periapical revelou um segundo molar inferior incluso, horizontalmente e a ausência do terceiro molar. O folículo dental do segundo molar era menor que 0,5 mm. Em função da idade, do dente ser assintomático e da possibilidade de perda do primeiro molar durante a cirurgia optou-se pelo controle periódico. No segundo ano de controle constatou-se a formação de um cisto dentígero no segundo molar incluso. Os cirurgiões devem avaliar o risco de uma cirurgia tardia, os benefícios ao paciente e estarem conscientes da necessidade de um controle periódico. É importante também ter o conhecimento que é impossível predizer se alguma alteração irá ocorrer se o dente não for removido.
Termos de indexação: Cisto dentígero. Cirurgia bucal. Dente incluso.
INTRODUCTION
The removal of asymptomatic, unerupted teeth, especially third molars, is controversial. In some cases it is believed that only asymptomatic, unerupted teeth associated with pathologies must be removed1-2. On the other hand, asymptomatic unerupted teeth are routinely extracted in many countries, and it is believed that asymptomatic unerupted teeth, mainly the third molar, must be removed prophylactically3-5.
This paper presents a clinical case of a dentigerous cyst (DC) occurring in a 60 year-old woman and discusses the recommendations to remove asymptomatic unerupted teeth.
CASE REPORT
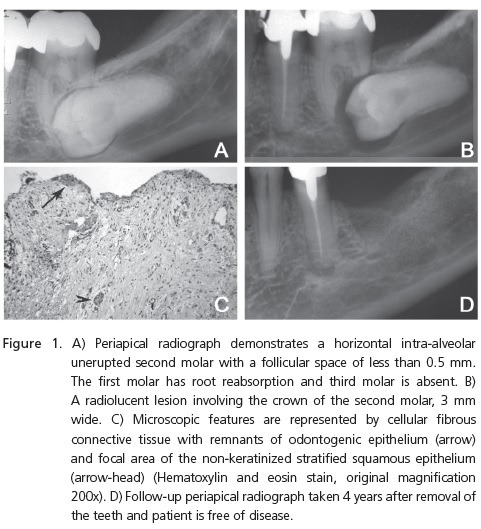
A 58 year-old white woman presented at the Oral Surgical Clinic of the School of Dentistry, Federal University of Minas Gerais (Belo Horizonte, Brazil) for the removal of an asymptomatic, unerupted left mandibular second molar, found in the x-ray. The periapical radiograph revealed a horizontal intra-alveolar, unerupted second molar and the absence of the third molar. The second molar had a follicular space of less than 0.5 mm. The first molar had pulp vitality, root reabsorption and no periodontal pocket or dental mobility (Figure 1A). The medical history was not significant. Due to the patient's age, the absence of symptoms and the risk of losing the first molar during surgery, periodic check-ups were recommended to the patient. In the 2nd year of check-ups, a radiolucent lesion was observed involving the crown of the impacted second molar (Figure 1B). The width of the radiolucent lesion was 3 mm. Once again, the pulp vitality of the first molar was confirmed. The clinical-radiographic diagnoses were odontogenic cysts (DC and odontogenic keratocysts), unicystic ameloblastoma and other odontogenic and nonodontogenic tumors. The surgical removal of the second and first molars was performed. Microscopic evaluation showed a cellular, fibrous, connective tissue with mononuclear inflammatory infiltrate and the remains of an odontogenic epithelium. Focal areas were lining by nonkeratinized, stratified, squamous epithelium (Figure 1C). A diagnosis of DC was made. There are no postoperative complications. The patient has been disease free for 4 years (Figure 1D).
DISCUSSION
The recommendations for the removal of asymptomatic unerupted teeth are many and frequently not based on reliable evidence6-7. There is a large discrepancy amongst oral surgeons in terms of opinion on the need for the removal of asymptomatic third molars and these opinions have not changed over the last 10 years6. Several studies suppose that asymptomatic unerupted teeth must be removed before pathological changes occur3-4, preventing the risk of post-surgical complications in older patients4,8-10.
Ahlqwist and Gröndahll11 concluded that long intervals may exist between follow-ups for asymptomatic, unerupted teeth. The current case illustrates the development of DC in a 60 year-old woman in a short period of follow-up. It demonstrates the need for and importance of regular follow-ups.
The benefit of a conservative approach is the avoidance of postoperative complications and the preservation of functional teeth and residual ridge1-2. However, postoperative complications occur with a frequency of less than 1% and an asymptomatic unerupted tooth does not play a role in this and the residual ridge is preserved with the correct surgical procedure13.
It is important to be aware that it is impossible to predict whether or not pathologies will occur if asymptomatic, unerupted teeth are not removed. The evaluation of the asymptomatic, unerupted teeth is mainly performed by radiographic examination. Sometimes, the radiographic appearance may not be a reliable indicator of the absence of disease within a dental follicle1,14. Glosser and Campbell15 described that the incidence of DC is higher than reported in radiographic studies. In the current case, the radiograph appearance was not sufficient to diagnose the radiolucent lesion involving the crown of the impacted second molar. So, there were different clinical-radiograph diagnoses and a histological evaluation was required for the final diagnosis.
Cysts may be encountered in the histopathological examination of asymptomatic third molars, especially in patients aged over 2016. In older patients, the morbidity associated with infection, general anesthesia and surgical procedures may be increased. Also, middle-age patients can develop the lesion9-10,17. So, surgical removal of impacted mandibular third molars should be carried out before the age of 249-10,17.
The early removal of asymptomatic impacted teeth can prevent future sequelae and risks to the patient and dental surgeons, it can be dramatically reduced by elective removal of the unerupted tooth4.
CONCLUSION
Oral surgeons must predict the risk of delayed surgery; the benefits to the patients and the need for a periodic checkup with short intervals of time in cases of the non- removal of the asymptomatic unerupted teeth. Also, it is important to be aware that it is impossible to predict whether or not some pathologies will occur if the teeth are not removed.
Collaborators
EN ABDO was responsible for the clinical case and the composition of the article. MD NAVES was responsible for the bibliographic survey and the composition of the article. MCF AGUIAR and RA MESQUITA were the pathologists responsible for the report and participated in the composition of the article.
REFERENCES
1. Adelsperger J, Campbell JH, Coates DB, Summerlin J-J, Tomich CE. Early soft tissue pathosis associated with impacted third molars without pericoronal radiolucency. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(4):402-6. [ Links ]
2. Hill CM. Removal of asymptomatic third molars: an opposing view. J Oral Maxillofac Surg. 2006;64(12):1816-20. doi: 10.1016/j. joms.2006.04.007.
3. Saglam AA, Tüzüm S. Clinical and radiological investigation of the incidence, complications, and suitable removal times for fully impacted teeth in Turkish population. Quintessence Int. 2003;34(1):53-9.
4. Kaminishi RM, Lam PS, Kaminishi KS, Marshall MW, Hochwald DA. A 10-year comparative study of the incidence of third molar removal in the aging population. J Oral Maxillofac Surg. 2006;64(2):173-4. doi: 10.1016/j.joms.2005.10.007.
5. Rafetto LK. Removal of asymptomatic third molars: a supporting view. J Oral Maxillofac Surg. 2006;64(12):1811-5.
6. Hamasha AA, Al Qudah MA, Bataineh AB, Safadi RA. Reasons for third molar teeth extraction in Jordanian adults. J Contemp Dent Pract. 2006;7(5):88-95.
7. Knutsson K, Brehmer B, Lysell L, Rohlin M. Dentists´decisons on prophylactic removal of mandibular third molars: a 10-year followup study. Community Dent Oral Epidemiol. 2001;29(4):308-14. doi: 10.1034/j.1600-0528.2001.290411.x.
8. Benediktsdóttir IS, Wenzel A, Petersen JK, Hintze H. Mandibular third molar removal: Risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(4):438-46. doi: 10.1016/j. tripleo.2003.10.018.
9. Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: Postoperative complications and their risk factors. J Can Dent Assoc. 2007;73(4):325.
10. Chuang SK, Perrot DH, Susarla SM, Dodson TB. Age as risk factor for third molar surgery complication. J Oral Maxillofac Surg. 2007;65(9):1685-92. doi: 10.1016/j.joms.2007.04.019.
11. Ahlqwist M, Gröndalhl H-G. Prevalence of impacted teeth and associated pathology in middle-aged and older Swedish women. Community Dent Oral Epidemiol. 1991;19(2):116-9.
12. Mercier P, Precious D. Risks and benefits of removal of impacted third molars. J Oral Maxillofac Surg. 1992;21(1):17-27. doi: 10.1016/S0901-5027(05)80447-3.
13. Haug RH, Perrott DH, Gonzalez ML, Talwar RM. The American association of oral and maxillofacial Surgeons age-related third molar study. J Oral Maxillofac Surg. 2005;63(8):1106-14. doi: 10.1016/j.joms.2005.04.022.
14. Monteiro L, Peña J, Fonseca L, Paiva A, Amaral B. Odontogenic cysts - A descriptive clinicopathological study. Braz J Oral Sci. 2005;4(12):670-5.
15. Glosser JW, Campbell JH. Pathologic change in soft tissues associated with radiographically "normal" third molar impactions. Br J Oral Maxillofac Surg. 1999;37(4):259-60. doi: 10.1054/ bjom.1999.0061.
16. Baykul T, Saglam AA, Aydin C, Basak K. Incidence of cystic changes in radiographically normal impacted lower third molar follicles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(5):542-5. doi: 10.1016/j.tripleo.2004.08.010.
17. Girod SC, Gerlach KL, Krueger G. Cysts associated with longstanding impacted third molars. Int J Oral Maxillofac Surg. 1993;22(2):110-2.
 Correspondence to:
Correspondence to:
EN ABDO
e-mail: evandro.abdo@gmail.com
Received on: 15/7/2008
Approved on: 8/12/2008













