Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.1 Porto Alegre Jan./Mar. 2013
ORIGINAL / ORIGINAL
Type of resin cement influences microleakage in ceromer inlays?
Tipo de cimento resinoso influencia a micorinfiltração em inlays de cerômero?
Raquel Viegas ELIASI; Ângela Brys OSÓRIOI; Hugo Ramalho SARMENTOI; Guilherme Brião CAMACHOI; Flávio Fernando DEMARCOI
I Universidade Federal de Pelotas, Faculdade de Odontologia, Programa de Pós-Graduação em Odontologia
ABSTRACT
Objective
To evaluate the influence of two resin cements on microleakage of ceromer inlays.
Methods
Twenty recently extracted human third molars were selected. Standard inlay mesio-occluso-distal cavities were prepared, with cervical margin in enamel (mesial) or dentin (distal). The specimens were randomly divided into two groups (n=10) and indirect restorations were made with Belleglass HP system (Kerr, Romulus, MI, USA). The cavities in the first group were treated with adhesive system Single Bond and restorations were cemented with dual curing cement RelyX ARC (3M ESPE, St. Paul, MN, USA). In the second group, the ED Primer (Kuraray, Tokyo, Japan) was applied and indirect restorations were cemented with Panavia 21 EX (Kuraray, Tokyo, Japan). The specimens were coated with varnish, except for the restorations and 1 mm around them and submitted to thermal cycling and then immersed in 2% basic fuchsine solution for 24 hours. Teeth were sectioned longitudinally and leakage scores were evaluated using a stereomicroscope at 40x magnification. Data were submitted to statistical analysis (Mann-Whitney test).
Results
Enamel showed lower dye penetration than dentin (p<0.05). Statistical difference between cements was only observed in enamel, with RelyX exhibiting less leakage (p<0.05).
Conclusion
Within the limitations of the study, the substrate had a significant effect for sealing ability and RelyX ARC performed better than Panavia 21 EX only in enamel.
Indexing terms: Composite resins. Dental leakage. Inlays. Resin cements.
RESUMO
Objetivo
Avaliar a influência de dois cimentos resinosos sobre a microinfiltração de inlays de cerômero.
Métodos
Vinte coroas de terceiros molars recentemente extraídos foram selecionadas.Cavidades do tipo Inlay padronizadas foram preparadas com a margem cervical em esmalte (mesial) ou dentina (distal). Os espécimes foram randomicamente distribuídos em dois grupos (n=10) e restaurações indiretas foram confeccionadas com o sistema Belleglass HP (Kerr, Romulus, MI, EUA). As cavidades do primeiro grupo foram tratadas com sistema adesivo Single Bond (3M ESPE, St. Paul, MN, USA) e as restaurações foram cimentadas com um cimento resinoso de cura dual (RelyX ARC, (3M ESPE, St. Paul, MN, EUA).No segundo grupo, ED Primer(Kuraray, Tokio, Japão)foi aplicado e as restaurações indiretas foram cimentadas com Panavia 21 EX (Kuraray, Tokio, Japão). Os espécimes foram pintados com verniz, exceto as restaurações e em torno de 1mm em volta destas,sendo então submetidos à termociclagem e imersos em solução de fucsina básica a 2% por 24 horas. Os dentes foram seccionados longitudinalmente e os escores de infiltração foram avaliados utilizando-se um estereomicroscópio com aumento de 40x. Os dados foram submetidos à análise estatística (teste de Mann-Whitney).
Resultados
O esmalte apresentou menor infiltração de corante que a dentina (p<0.05). Diferenças estatística entre cimentos foram observadas apenas em esmalte, com o cimento RelyX ARC exibindo menor infiltração (p<0.05).
Conclusão
Dentro das limitações deste estudo, observou-se que o substrato dentário apresentou um efeito significante para o selamento cavitário e o cimento RelyX ARC mostrou-se melhor que o Panavia 21 EX apenas em esmalte.
Termos de indexação: Resinas compostas. Infiltração dentária. Restaurações intracoronárias. Cimentos de resina.
INTRODUCTION
In the last few years, aesthetic concerns have produced an increased demand for tooth-colored restorations, even in posterior teeth. Direct composite restorations have gained in popularity, being an acceptable alternative to amalgam restorations. Despite the good results observed for direct composite restorations in posterior teeth, the inherent polymerization shrinkage could cause stress at the adhesive interface. If the resin contraction exceeds the bond strength between the material and dental tissue, a gap is formed, frequently detected in class II restorations, causing leakage. Moreover, obtaining adequate proximal contact is a problem when dealing with direct composite restorations1.
Since polymerization shrinkage has been associated with deleterious effects at the adhesive interface, different restorative techniques have been advocated to minimize the harmful effects on restoration longevity2. Indirect restorations have been used to reduce or minimize polymerization shrinkage. One possible reason for this is the small amount of resinous material (resin cement) used in luting procedures3-4.This technique provides better sealing than direct composites, on enamel2. Moreover, it is used to facilitate the reproduction of the dental anatomy, in order to improve control of the marginal fit, proximal and occlusal contacts3.
When compared to other indirect restorations, like ceramics, indirect composite restorations present a more simple fabrication technique, less wear on the antagonist teeth, the possibility of intra-oral repair and lower cost5. In addition, in vitro studies revealed that teeth restored with indirect ceromer showed statistically higher fracture resistance than certain ceramics6.
Microleakage is still considered to be a problem for indirect adhesive treatment, especially for inlay restorations, which represents a highly unfavorable C-factor (configuration factor), increasing polymerization stress7. Because of this, adverse effects could appear, such as contraction stress, sensitivity, recurrent caries and negative pulpal sequelae1. Substrate has influenced marginal sealing ability and microleakage tends to be more severe in cervical margins located in dentin7-8 than in enamel. However, the improvements in dentin bonding agent technology have produced similar bond strength values for enamel and dentin and recent studies have detected similar performances with regard to microleakage for direct and indirect Class II restorations with margins located in enamel or dentin9.
Since polymerization shrinkage is restricted to the resin cement in indirect restorations, the properties of these cements may significantly affect the performance of the restorations, in respect of the sealing ability of indirect restorations7.
The purpose of this study was to assess the microleakage of ceromer inlays at enamel and dentin margins using two resin cements. The null hypothesis to be tested is that different substrates and resin cements have similar sealing ability.
METHODS
Tooth selection and preparation: Twenty human third molars, recently extracted for periodontal reasons, were selected. After removal of soft tissue, the teeth were stored in 1% chloramine solution for 72 hours and frozen in distilled water awaiting testing. In addition, the teeth were evaluated under magnification (10x) to ensure that the specimens were free from any decay, cracks or previous restorations. Then the root base of each tooth was embedded in acrylic resin on a PVC matrix.
Preparation design
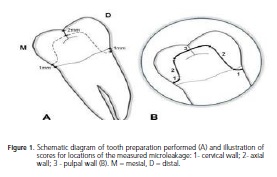
Standard Class II MOD (mesio-occluso-distal) inlay cavities were prepared. Diamond burs #4138 (KG Sorensen, Alphaville, Brazil) were mounted on a Galloni Machine (S. Colombano, Milan, Italy) to obtain a standardized cavity preparation. Burs were replaced after four cavity preparations to ensure high cutting ability. The occlusal box was 2 mm deep and 2 mm across in the bucco-lingual dimension. The mesial cervical wall was located in enamel (1 mm above the cementoenamel junction), with the distal surface located in cementum-dentin (1 mm below the CEJ - cementum-enamel junction-) (Figure 1). Buccal and lingual walls were tapered (6o) and internal angles were rounded7.
Inlay fabrication: Impressions were made from each cavity preparation, using condensation silicone (Silon, Caulk/Dentsply, Petrópolis, Brazil) to produce the models in stone matrices (Durone- Caulk/Dentsply, Petrópolis, Brazil) that were used to prepare the composite inlays.
The polymerization of the indirect restorations was performed in accordance with manufacturer's recommendations. For Belleglass HP, TekLite unit (Kerr, Romulus, MI, USA) was used, which provides a high intensity with a 80W halogen light (wavelength of 400-500nm, for 60s). After this period, additional polymerization was carried out with an HP Curing Unit (Kerr, Romulus, MI,USA), under nitrogen pressure (60 psi) at 140°C, for 20 minutes.
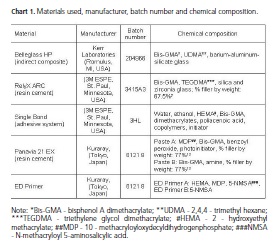
Initial preparation of samples: The internal surface of all ceromer restorations was prepared using sandblasting treatment (Microetcher Model II - Danville Engineering Inc., San Ramon, California) and a silane coupling agent was also applied (Caulk/Dentsply, Petrópolis, Brazil). The teeth were randomly allocated to two groups (n=10), in accordance with the resin cements. The materials used in this study, as well as their respective manufacturers, batch numbers and chemical composition, are presented in Chart 1.
Luting procedures
Prior to the luting procedures, the specimens were cleaned with bristles and polishing paste. To lute the ceromer inlays, a light curing unit (XL 3000, 3M ESPE, St. Paul, Minnesota, USA) was used, with energy greater than 450mWcm2, constantly monitored with the internal radiometer.
RelyX ARC: Tooth surfaces were conditioned with 35% phosphoric acid (3M ESPE, St. Paul, Minnesota, USA) for 15s. The surface was washed and lightly dried, keeping it moist. Two coats of the adhesive system Single Bond (3M ESPE, St. Paul, Minnesota, USA) were applied and photo-cured for 20s. RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) was dispensed, mixed and applied to the inlay's internal surface. Inlays were held in place for 8 minutes under 500 g of pressure, using a modified Vicat needle. Excess cement was removed using scalers before light curing of interfaces for 40 seconds.
Panavia 21 EX: The enamel was etched with phosphoric acid for 30 seconds. After washing and drying,ED primer was applied to the enamel and dentin. Panavia 21 EX cement was mixed and thinly applied to the internal surface of the inlay. The same modified Vicat needle was used to keep the restorations in place for 8 minutes. Excess cement was removed and the restoration margins were protected with Oxyguard. The inlay interfaces were light cured for 40 seconds.
The specimens were stored in distilled water for seven days, at which time the teeth were removed from the PVC matrixes. Polishing of inlay margins was performed using the Enhance system (Caulk/Dentsply, Petrópolis, Brazil) and polishing pastes (Diamond- FGM Produtos Odontológicos, Joinville, Brazil).
Microleakage test
The samples were subjected to thermal cycling in a thermocycler machine (Ética Odontológica, São Paulo, Brazil) for 500 cycles at 5°C and 55°C in water. The time of immersion in each bath was 30 seconds and transfer time between the two baths was 2 seconds.
The entire surface of each tooth was then coated with nail varnish, except for the margins of the restorations and 1 mm around them. Following 24 hours immersed in 2% basic fuchsine solution, the teeth were washed in tap water for 12 hours and the nail varnish was removed. The teeth were then embedded in transparent acrylic resin and a centrally located section was performed across the restorations using a band saw (Buhler Inc., Lake Buff, IL, USA), enabling the measurement of leakage.
To compute microleakage, the specimens were examined at a magnification of 40x using a stereomicroscope (Tecnival, Biosystems Ltda., Curitiba, Brazil). The leakage was assessed by three examiners using a standardized scoring method for dye penetration7: 0 - no penetration; 1 - restricted to the cervical wall; 2 - restricted to the axial wall; and 3 - reaching the pulpal wall (Figure 1). If the examiners disagreed about the leakage scores, a consensus was obtained.
Statistical analysis: Data were subjected to non-parametric statistical analysis (Mann-Whitney test) at a confidence level of 95%.
Ethical considerations: This study was conducted in accordance with the Declaration of Helsinki (2000).
RESULTS
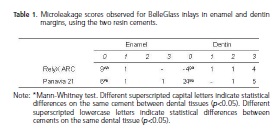
Dye penetration scores for ceromer restorations luted with both resin cements, on enamel and dentin margins, are displayed in Table 1. The non-parametric test (Mann-Whitney) revealed lower leakage on enamel than on dentin margins (p<0.05).
With enamel margins, better sealing performance was observed in indirect inlays luted with RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) (p<0.05) in relation to those luted with Panavia. In 90% of the inlays cemented with RelyX, enamel leakage-free margins were observed, whereas in those cemented with Panavia, the leakage-free margin rate was 60%.
For the dentin interface, no statistical significant difference was found between the groups (p>0.05). Both resin cements provided the same rate of leakage-free interface (40%). The tested null hypothesis was rejected, since the materials and the substrate had a significant influence on sealing capacity.
DISCUSSION
In vitro studies provide important information when assessing new techniques to improve bonding to dental tissues. Since studies showed that cementation techniques currently in use for indirect restorations are not capable of producing complete sealing of the exposed dentin, leaving a potential pathway for bacterial infiltration, it is important to evaluate the microleakage of resin cements used to bond this kind of restoration8. Generally, microleakage has been evaluated on in vitro models, dye penetration being the method most frequently used. Despite the low cost and ease of application, this kind of test presents some limitations, such as the subjectivity of reading, high diffusibility of the dyes due to their low molecular weight10. However, since new materials are constantly emerging and as clinical evaluations are time-consuming and expensive, in vitro methods for microleakage are important tools for evaluating the possible performance of the materials with regard to sealing ability7. In this study, qualitative measurement of dye penetration and fuchsine basic selection to reveal leakage, were based on a review of the literature in respect of microleakage methodology8,10. Recently, extracted human third molars were used to simulate the clinical condition. However, the age of the tooth, the occlusal forces on the tooth, the patient's eating habits and the forces applied during tooth extraction are uncontrollable, confusing variables that may have an effect on the tooth condition at the marginal interface and could cause an unpredictable standard deviation in the microleakage patterns11.
Indirect resin composites were introduced to reduce polymerization shrinkage and improve the properties of the material. Moreover, a ceromer restoration shows better marginal adaptation than ceramics due to lower polymerization contraction4. In this study, all restorations were previously subjected to thermal cycling in order to subject them to the challenges of thermal expansion/contraction. The different thermal expansion coefficients of tooth tissue in comparison with restorative materials may lead to gap formation3. To assess the in vitro performance of resin materials, thermocycling has been a commonly used method to simulate the long-term stresses to which the resin restorations are clinically exposed.
Some degree of infiltration was found in both cements used in this study, and these findings agree with other studies2,7-8,12. According to Browning and Safirstein12, microleakage between the tooth substrate and restorative materials can be expected for all restorative polymers. A reasonable explanation for this is that the adhesive bond is weakened or even broken by the inevitable dimensional changes that occur when materials polymerize13. However, polymerization shrinkage is just one of the parameters that plays a role in the mechanisms and durability of adhesion. There are a number of other factors, including the extent of marginal gap, varying the coefficient of thermal expansion for the restoration and cementing materials14, degradation of particular bonding or restorative materials15, or the dissolution of liners or smear layers1. In the present study, two resin cements were applied to bond BelleGlass inlayrestorations. In dentin, both materials performed similarly, but in enamel the RelyX had significantly lower leakage than Panavia. These resin cements have not been previously compared with regard to their ability to seal ceromer inlays. In bonded amalgam restorations, RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) presented similar leakage patterns to Panavia 21 EX9. In some studies, it was observed that indirect ceramic inlays, bonded with Panavia 21, showed higher microleakage values than RelyX ARC (3M ESPE, St. Paul, Minnesota, USA), for margins in enamel17,18 but no significant differences were found in dentin margins17.The same occurred in this study, where microleakage in enamel was lower in RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) than with Panavia 21 and similar in dentin.
The results also showed a higher microleakage in dentin than in enamel, regardless of the cement used. These findings disagree with the results previously found by Soares et al.19, who reported that indirect restorations showed the same microleakage as direct restorations when the gingival margin preparation was placed in enamel, and less microleakage on indirect restoration when the margin was placed in dentin. In order to work around this limitation of resin cements, some studies have observed that a resin liner around the cavities, after applying the adhesive system and before restoration cementation, provided less microleakage in dentin, even where self-adhesive cements are employed, with no significant improvements in the enamel-restoration interface8,20. Moreover, a study showed that chlorhexidine application prior to the adhesive system, reduces gingival microleakage in an etch-and-rinse cement even after aging by water storage8.
A study18 showed that Panavia 21, associated with ED Primer, showed the lowest microleakage compared to the other Panavia 21/ dentin adhesive combinations. According to results found in the present study, this study showed that Panavia 21, combined with ED Primer, led to significantly higher microleakage values in enamel margins compared to RelyX ARC (3M ESPE, St. Paul, Minnesota, USA)18. This can be explained by the 2 different enamel bonding mechanisms of the total-etch and the self-etching techniques. The slow polymerization rate of Panavia 21 may allow more water to diffuse from the dentin into the hydrophilic interface between the Panavia 21 primer and dentin, due to its more hydrophilic nature21-22. Although there is a susceptibility to hydrolytic degradation on the Panavia 21/ dentin interface exposed to water, no significant difference in microleakage was observed between the cements used in the present study. This observation may be attributed to the presence of MDP in both ED primer and Panavia 21.
Results of the current study showed that the etch-and-rinse cementation bonding protocol was more effective in reducing microleakage on enamel than the self-etching protocol. This may have occurred because the self-etching primer used in this study is acidic and has a hydrophilic monomer, presenting a high HEMA concentration (30% to 50%), which can lead to water uptake and hydrogel formation8 during thermocycling. This additional path for water movement can lead to degradation of the bonding interface under water storage in the long term23. Furthermore, the evaporation of water in mixtures of water-HEMA present in self-etching primers, is more difficult24. The incomplete polymerization due to the remaining water and increased permeability in a one-step self-etch adhesive can make the substrate-adhesive interface more susceptible to hydrolytic degradation. In this regard, it has been advocated that applying an additional resin layer after application of self-etching adhesives, results in a significant reduction in dentin microleakage after a 6-month period of water storage, although no significant advantage with microleakage in enamel was noticed8.
Both in vivo and in vitro studies, showed that the width of the marginal gap was significantly higher in proximal margins (in dentin) than occlusal margins (enamel)8,25-26. The same was observed in this study. This may be due to the fact that, while enamel is an almost completely mineralized tissue, with low organic composition, dentin has lower mineral content, with an organic matrix and a wet surface due to the presence of dentin fluid. Thus enamel adherence has generally been reported to be stronger and more stable than that obtained in dentin27. In another study, dual-cure resin cements RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) and Panavia used to bond full cast crowns, were associated with a higher degree of microleakage, both in enamel and dentin, than conventional glass-ionomer cement (Fuji I) and the resin-modified glass–ionomer cement (Fuji Plus)26. The greater leakage of the resin cements RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) and Panavia F, when compared to the conventional glass-ionomer cement Fuji I and the resin-modified glass-ionomer Fuji Plus, was attributed to polymerization shrinkage of the resin cements, combined with the coefficients of thermal expansion of the materials involved (i.e. tooth substrate, cement, metal crown), during aging14.
RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) and Panavia are cements with different chemical compositions and inorganic filler content, but differences in our results might not be explained by the different performance observed in enamel margins. Probably the main factor regarding sealing ability observed in enamel is associated with the different adhesion mechanisms of the tested cements. RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) is used with a total etch adhesive, where the entire cavity is conditioned with phosphoric acid, which will promote enamel and dentin demineralization, with complete removal of smear layer, exposing a collagen network. The application of the adhesive system (Adper Single Bond) will encapsulate this unprotected collagen, forming the hybrid layer. As for Panavia, the acid etching was restricted to enamel producing the demineralization of this substrate, and the entire cavity was treated with a self-etching agent (ED Primer) that modifies the smear layer.
In vitro tests are useful tools to predict the clinical performance of dental materials, but the results of such studies should be carefully reported to the clinic. However, long-term clinical evaluations are key to the selection of dental materials. So, the final evaluation of a material, including resin cements, should be performed in long-term clinical studies.
CONCLUSION
Given the limitations of this in vitro study, it was possible to conclude that: substrate was a significant factor in sealing ability; microleakage in ceromer inlays was lower with enamel than dentin; the two resin cements evaluated in this study had similar performance on dentin, but on enamel, RelyX ARC (3M ESPE, St. Paul, Minnesota, USA) had better sealing than Panavia 21 EX.
Collaborators
RV ELIAS, ÂB OSÓRIO and HR SARMENTO contributed to the experimental procedures in the study, data analysis and composition of the article. GB CAMACHO contributed to the study conception and experimental design definition, data analysis and composition of the article. FF DEMARCO contributed to the study conception and experimental design definition, data analysis and composition of the article.
REFERENCES
1. Demarco FF, Correa MB, Cenci MS, Moraes RR, Opdam NJM. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28(1):87-101. doi: 10.1016/j. dental.2011.09.003. [ Links ]
2. Duquia ReC, Osinaga PW, Demarco FF, de V Habekost L, Conceição EN. Cervical microleakage in MOD restorations: in vitro comparison of indirect and direct composite. Oper Dent. 2006;31(6):682-7. doi: http://dx.doi.org/10.2341/05-132. [ Links ]
3. Coelho-De-Souza FH, Camacho GB, Demarco FF, Powers JM. Fracture resistance and gap formation of MOD restorations: influence of restorative technique, bevel preparation and water storage. Oper Dent. 2008;33(1):37-43. doi: 10.2341/07-27. [ Links ]
4. Nandini S. Indirect resin composites. J Conserv Dent. 2010;13(4):184-94. doi: 10.4103/0972-0707.73377. [ Links ]
5. Peutzfeldt A. Indirect resin and ceramic systems. Oper Dent. 2001;6:153-76. [ Links ]
6. Soares CJ, Martins LR, Pfeifer JM, Giannini M. Fracture resistance of teeth restored with indirect-composite and ceramic inlay systems. Quintessence Int. 2004;35(4):281-6. [ Links ]
7. Mota CS, Demarco FF, Camacho GB, Powers JM. Microleakage in ceramic inlays luted with different resin cements. J Adhes Dent. 2003;5(1):63-70. [ Links ]
8. Shafiei F, Doozandeh M, Alavi AA. Effect of resin coating and chlorhexidine on the microleakage of two resin cements after storage. J Prosthodont. 2011;20(2):106-12. doi: 10.1111/j.1532-849X.2010.00670.x. [ Links ]
9. Cenci M, Demarco F, de Carvalho R. Class II composite resin restorations with two polymerization techniques: relationship between microtensile bond strength and marginal leakage. J Dent. 2005;33(7):603-10. [ Links ]
10. Raskin A, D'Hoore W, Gonthier S, Degrange M, Déjou J. Reliability of in vitro microleakage tests: a literature review. J Adhes Dent. 2001;3(4):295-308. [ Links ]
11. Dennison JB, Sarrett DC. Prediction and diagnosis of clinical outcomes affecting restoration margins. J Oral Rehabil. 2012;39(4):301-18. doi: 10.1111/j.1365-2842.2011.02267.x. [ Links ]
12. Browning WD, Safirstein J. Effect of gap size and cement type on gingival microleakage in Class V resin composite inlays. Quintessence Int. 1997;28(8):541-4. [ Links ]
13. Irie M, Suzuki K. Current luting cements: marginal gap formation of composite inlay and their mechanical properties. Dent Mater. 2001;17(4):347-53. doi: 10.1016/S0109-5641(00)00093-2. [ Links ]
14. Cenci MS, Pereira-Cenci T, Donassollo TA, Sommer L, Strapasson A, Demarco FF. Influence of thermal stress on marginal integrity of restorative materials. J Appl Oral Sci. 2008;16(2):106-10. doi: 10.1590/S1678-77572008000200005. [ Links ]
15. Thordrup M, Isidor F, Hörsted-Bindslev P. A 5-year clinical study of indirect and direct resin composite and ceramic inlays. Quintessence Int. 2001;32(3):199-205. [ Links ]
16. Fortin D, Swift EJ, Denehy GE, Reinhardt JW. Bond strength and microleakage of current dentin adhesives. Dent Mater. 1994;10(4):253-8. doi: 10.1016/0109-5641(94)90070-1. [ Links ]
17. Gerdolle DA, Mortier E, Loos-Ayav C, Jacquot B, Panighi MM. In vitro evaluation of microleakage of indirect composite inlays cemented with four luting agents. J Prosthet Dent. 2005;93(6):563-70. doi: 10.1016/j.prosdent.2005.04.004. [ Links ]
18. Uludag B, Ozturk O, Ozturk AN. Microleakage of ceramic inlays luted with different resin cements and dentin adhesives. J Prosthet Dent. 2009;102(4):235-41. doi: 10.1016/S0022-3913(09)60161-X. [ Links ]
19. Soares CJ, Celiberto L, Dechichi P, Fonseca RB, Martins LR. Marginal integrity and microleakage of direct and indirect composite inlays: SEM and stereomicroscopic evaluation. Braz Oral Res. 2005;19(4):295-301. [ Links ]
20. Kitayama S, Nasser NA, Pilecki P, Wilson RF, Nikaido T, Tagami J, et al. Effect of resin coating and occlusal loading on microleakage of Class II computer-aided design/computer-aided manufacturing fabricated ceramic restorations: a confocal microscopic study. Acta Odontol Scand. 2011;69(3):182-92. [ Links ]
21. Salz U, Zimmermann J, Salzer T. Self-curing, self-etching adhesive cement systems. J Adhes Dent. 2005;7(1):7-17. [ Links ]
22. Carvalho RM, Pegoraro TA, Tay FR, Pegoraro LF, Silva NR, Pashley DH. Adhesive permeability affects coupling of resin cements that utilise self-etching primers to dentine. J Dent. 2004;32(1):55-65. doi: 10.1016/j.jdent.2003.08.003. [ Links ]
23. Sauro S, Pashley DH, Montanari M, Chersoni S, Carvalho RM, Toledano M, et al. Effect of simulated pulpal pressure on dentin permeability and adhesion of self-etch adhesives. Dent Mater. 2007;23(6):705-13. doi: 10.1016/j.dental.2006.06.010. [ Links ]
24. Pashley EL, Zhang Y, Lockwood PE, Rueggeberg FA, Pashley DH. Effects of HEMA on water evaporation from water-HEMA mixtures. Dent Mater. 1998;14(1):6-10. doi: 10.1016/S0109-5641(98)00003-7. [ Links ]
25. Gemalmaz D, Kükrer D. In vivo and in vitro evaluation of marginal fit of class II ceromer inlays. J Oral Rehabil. 2006;33(6):436-42. doi: 10.1111/j.1365-2842.2005.01562.x. [ Links ]
26. Piwowarczyk A, Lauer HC, Sorensen JA. Microleakage of various cementing agents for full cast crowns. Dent Mater. 2005;21(5):445-53. doi: 10.1016/j.dental.2004.07.009. [ Links ]
27. De Munck J, van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84(2):118-32. doi: 10.1177/154405910508400204. [ Links ]
 Correspondence to:
Correspondence to:
FF DEMARCO
Rua Gonçalves Chaves, 457/504, Centro, 96015-560, Pelotas, RS, Brasil.
e-mail: ffdemarco@gmail.com
Received on: 21/10/2011
Final version resubmitted on: 2/4/2012
Approved on: 23/4/2012













