Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.1 Porto Alegre Jan./Mar. 2013
ORIGINAL / ORIGINAL
The approval rating through the use of an interocclusal device
Grau de satisfação pelo uso de um dispositivo interoclusal
Francisco Artur Forte OLIVEIRAI; Clarissa Pessoa FERNANDESI; Filipe Nobre CHAVESII; Lorena Barreira MAGROI
I Faculdade São Leopoldo Mandic, Curso de Odontologia, Programa de Pós-Graduação em Disfunção Temporomandibular
II Universidade Federal do Rio Grande do Sul, Instituto de Ciências Básicas da Saúde, Departamento de Ciências Morfológicas. Porto Alegre, RS, Brasil
ABSTRACT
Objective
The objective of this study was to assess the approval rating of patients with muscular and/or joint TMD during the use of an interocclusal device.
Methods
51 consenting patients were selected with muscular and/or joint TMD, according to the criteria of the Research Diagnostic Criteria protocol (RDC/TMD) and needing the use of an interocclusal device as part of a conservative treatment at the São Leopoldo Mandic Dental Research Center in Campinas, São Paulo, Brazil. The interocclusal device was installed using the protocol defined by the manufacturer for its use and adaptation. The satisfaction questionnaire was applied to the subjects of the research after 30 days using the interocclusal device.
Results
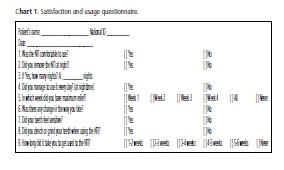
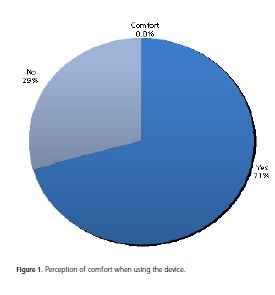
The results were: 71% of the patients had felt comfortable using the device; 73% used the device all night long, but 27% removed it at some time during the night, and 5 of these patients removed it every night, thus they did not succeed in using this type of device; 88% used it daily; 70% achieved the greatest relief from the main complaint in the first 3 weeks; 61% did not notice any change in bite; 47% did not feel any kind of tooth sensitivity; 51% did not grind their teeth with the use of the device and 72% took one or two weeks to get used to the device.
Conclusion
The majority obtained a high level of rating approval during the use of an interocclusal device.
Indexing terms: Instrumentation. Patient satisfaction. Temporomandibular joint dysfunction syndrome.
RESUMO
Objetivo
Avaliar o grau de satisfação por parte dos pacientes com disfunção temporomandibular muscular, articular ou ambas com o uso de um dispositivo interoclusal parcial anterior.
Métodos
Foram selecionados 51 pacientes com disfunção temporomandibular muscular, articular ou ambas, segundo os critérios de diagnóstico do protocolo Research Diagnostic Criteria (RDC/TMD) e que necessitassem do uso de um dispositivo interoclusal como parte de um tratamento conservador, na clínica do Centro de Pesquisas Odontológicas São Leopoldo Mandic, Campinas, São Paulo. O dispositivo foi instalado utilizando-se o protocolo definido pelo fabricante para seu uso e adaptação. Foi aplicado aos indivíduos da pesquisa o questionário de satisfação, após 30 dias do uso do dispositivo interoclusal.
Resultados
Os resultados obtidos demonstraram que: 71% dos pacientes sentiram conforto ao usar o dispositivo; 73% usaram o aparelho durante toda à noite, mas 27% não conseguiram sendo que cinco desses pacientes retiraram por todas as noites, ou seja, não alcançaram êxito com o uso desse tipo de dispositivo; 88% usaram diariamente. O alívio maior da queixa principal foi alcançado nas três primeiras semanas por 70% dos pacientes; 61% não notaram mudanças na mordida; 47% não relataram sensibilidade nos dentes; 51% não rangeram ou apertaram os dentes com o uso do dispositivo e 72% precisaram de uma a duas semanas para se acostumarem com o dispositivo.
Conclusão
A maioria dos indivíduos da pesquisa alcançou um alto grau de satisfação ao usar o dispositivo.
Termos de indexação: Instrumentação. Satisfação do paciente. Síndrome da disfunção da articulação temporomandibular.
INTRODUCTION
Temporomandibular dysfunction (TMD), a term adopted by the American Dental Association (ADA), is a set of joint and muscle disturbances in the orofacial area, primarily characterized by pain, joint noise and mandibular function which is abnormal or has some deviation1. The pain is not of neurogenic, psychogenic or visceral origin. Periodontal, dental and skin pains were also excluded from this definition2.
Interocclusal appliances are often used to treat patients with TMD with the aim of stabilizing the unstable occlusion, rearranging the function of chewing muscles, of TMJ, relieving the painful symptoms experienced by these patients3. They are also recommended for the protection of teeth of patients with nocturnal bruxism4.
The risk of side effects is low and depends on the appliance design and the length of use, since it is a conservative method of treatment5. When used incorrectly, they can produce serious, irreversible consequences6. The risk is particularly great in cases of mandibular advancement splints and with partial coverage devices (they only come into contact with parts of the antagonist teeth), used for a period of time in excess of four to six weeks, and without proper supervision7.
With the emergence of a new interocclusal device to treat TMDs, the nociceptive trigeminal inhibitor (NTI), studies have started to be carried out to prove its effectiveness8.
The aim of the present study was to evaluate the degree of satisfaction of patients with muscular TMD, joint TMD, or both, with the use of the partial anterior interocclusal device, the NTI.
Manns et al.9 selected 75 patients (9 males and 66 females aged between 13 and 53), with TMD symptoms. The vertical dimensions were taken with a minimum of muscle activity (evaluated via electromyography) for each patient, and based on these data, they were divided into three groups: group I with 1 mm of splint height; group II with an average height of 4.42 mm; and group III at 8.15 mm. It was found that the temporary use of the splint, with a height beyond the physiological rest position, did not cause an increase in muscle tone, nor hyperactivity of the masseter muscles; according to these authors, this provided greater neuromuscular relaxation.
Clark6 conducted a critical review with appliances with an anterior bite plane which was used in cases of occlusal alteration to reestablish a new vertical dimension and muscle relaxation. The author concluded that this type of interocclusal device could produce irreversible complications, such as dental intrusion and extrusion, when used for long periods, and are therefore recommended for emergency interventions such as trismus or reduced opening of the mouth.
Continuing this line of research, Boero4 performed a review of four basic types of splint (stabilizing, pivoting, resilient and repositioning). He concluded that the muscles that raise the lower jaw are more efficient when the vertical dimension is more increased than in the vertical dimension of occlusion and that the postural position with minimum muscle activity is vertically greater than the clinical rest position. The interocclusal splints that increase the vertical dimension beyond the free function space produce an accommodation of the central nervous system to this alteration, and as a consequence produce a reduction in electromyographic activity of the anterior temporal muscles.
List & Helkimo5 evaluated the effects of therapy with an occlusal splint in a sample of 61 patients with TMD (17 men and 44 women with ages ranging from 19 to 69). A total of 10% of patients were assessed as very comfortable, another 10% as comfortable, 80% said that it was neither comfortable nor uncomfortable, and one patient reported discomfort when using the occlusal splint.
Attanasio10 described the therapy with intraoral appliances with anterior bite plane, emphasizing that these lead to complete posterior disocclusion, there being no load on the structures of the stomatognathic system via the posterior teeth, and as such are well recommended for the control of nocturnal bruxism with painful symptoms in the muscles deriving from parafunctional behavior. This appliance reduces the activity of the temporal muscle when swallowing and also releases the mandibular along the antero-posterior axis for repositioning. Care should be taken with the possibility of the super-eruption of the posterior teeth with the continuous use of the appliance.
Para Widmalm7, despite divergence over the value of therapy using the splint, it is reasonable to recommend its use, as follows: to protect the oral tissue of patients with oral parafunction; to stabilize unstable occlusions; to eliminate the effect of occlusal interference and to test the effects that changes in occlusion could have on TMJ function and the chewing muscles prior to restorative treatment.
Omatsu et al.11 selected 10 healthy volunteers. Two types of device were fabricated for each individual, one incisal splint that covered the upper central incisors and had only one point of contact with the lower incisors in any position of the lower jaw and the stabilizing splint. They concluded that the incisal plate can significantly reduce muscle activity and should be used more for the treatment of the symptoms of nocturnal clenching.
Ekberg et al.12 selected 60 patients (52 women and 8 men with an average age of 29) out of 926 who sought treatment for TMD at the Faculty of Dentistry in Malmö. They obtained the following data: 23% of the patients in the treatment group and 30% in the control group complained of discomfort with the use of the splint; 83% of the treatment group and 77% in the control group said they had used the splint every night or nearly every night.
Helkimo13 issued an opinion for the Swedish Dental Association about the use of the NTI-tss device (nociceptive trigeminal inhibition - tension suppression system) for the treatment of stomatognathic problems and migraine. It is called this as it has a reduced frontal contact, leading to the reduction of bite force, clenching and grinding. The aforementioned "suppression" is ostensibly due to a natural reflex to prevent a load increase on the teeth, reducing or preventing the "muscle trigger component of migraine". There are no studies to prove that the NTI was superior to the other existing devices for the treatment of myofascial pain and TMD, or that there is some other mechanism whose effectiveness is different from the action mechanism of the other deprogrammers. Unlike the stabilizing splints, the NTI carries a risk of producing adverse effects on the occlusion.
Magnusson et al.14 selected 30 patients with signs and symptoms of TMD to be treated either with a stabilizing splint or with a new type of device based on the concept of nociceptive trigeminal inhibition (NTI). The result was that four subjects in the NTI group accepted a switch to the stabilizing splint group because of a lack of improvement or because of a worsening of the symptoms, considering this therapy to be unsatisfactory. On the other hand, no subject in the stabilizing splint group agreed to switch to the NTI group. Nine patients in the NTI group experienced using two types of appliance and seven of these deemed the stabilizer splint to be more comfortable than the NTI. The use of the NTI for a long period could be detrimental to occlusion. The positive effects attributed to the use of the NTI seem to be extremely exaggerated and no support was found for the statement that the NTI is a substitute for the conventional interocclusal appliance.
Jokstad et al.8 selected 40 TMD clinic patients. Two types of appliance were used: a Michigan stabilizing splint and the NTI. The differences in the devices were not described to the patients. Comfort with the use of the appliance seemed to be similar in the two groups based on the score in the visual-analog scale, although the NTI has shown a tendency to being more comfortable. As far as the NTI is concerned, the most frequent complaints were dry mouth attributed to the design of the appliance which obliges an open bite; appliance drops out or it is removed subconsciously while asleep; difficulty in swallowing; irritation at the tips and sensitivity of the lower anterior teeth.
Stapelmann and Turp15, in a systematic review, compared the available evidence on the efficacy and safety guaranteed by the NTI-tss manufacturer for the treatment and prevention of bruxism, TMD, tension headache and migraine. The review was performed on nine electronic databases and on NTI-tss associated websites. The results were that the NTI-tss led to complications with individual teeth or with occlusion. The recommendation to use the NTI-tss could be justified to reduce activity in the muscles used to close the lower jaw (tooth clenching or grinding), or as an emergency device for patients with acute temporomandibular pain and limitations on the opening of the mouth.
METHODS
A total of 51 volunteer patients were selected, of both sexes, regardless of race and aged between 17 and 73 (average age 41.94), and comprised 6 men (11.76%) and 45 women (88.24%), with muscular and/or joint TMD, according to the diagnostic criteria of the I-a and l-b axes of the Research Diagnostic Criteria protocol (RDC/TMD)16 and who needed to use an interocclusal device as part of a conservative treatment, in the clinic of the São Leopoldo Mandic Center for Dental Research, Campinas (in the state of São Paulo). The only exclusion criterion was the refusal of the patient to take part in the study.
This was a cross-sectional, clinical study, with no dropouts during the treatment, in which the interocclusal device (Standard NTI-tss model) was installed using the protocol defined by the manufacturer. After explaining the study and acquiring the agreement of the volunteers to take part in the study, the Free and Informed Consent Form was signed.
For the data collection, the individuals were given a satisfaction questionnaire to complete (Chart I), after 30 days using the interocclusal device. The patient received the card and answered the questions, requesting assistance from the operator in the event of any doubtson how to fill it in. The data obtained were tabulated and graphs produced.
The research project was submitted to and approved by the Ethics in Research Committee at the São Leopoldo Mandic Center of Dental Research on March 19, 2007, filed under reference 07/475, being in compliance with the ethical principles contained in the Declaration of Helsinki (2000), and also in compliance with the specific legislation of the country in which the study was conducted.
RESULTS
The results are arranged in the form of figures:
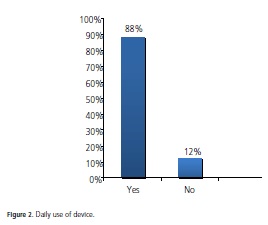
With regard to the usage of the device, 88% of patients used it every day, that is to say, every night for 30 days, while 12% did not.
As for the use of the device throughout the night, 73% of patients used it the whole night while 27% did not.
Of the 14 patients, one removed it on three occasions, one for four nights, one for seventeen nights, two for one night, two for two nights, two for five nights and five removed the device every night, i.e. they were unable to go on using this type of device.
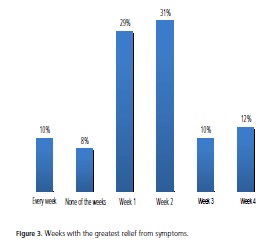
As far as the primary complaint is concerned, the greatest relief occurred in the first week for 29% of patients, the second week for 31%, the third week for 10%, fourth week for 12%, the same every week for 10% and no relief for 8%.
In relation to the occlusal/dental aspects, 39% of patients experienced some form of change in their bite (the teeth came into contact with each other differently immediately after using the device, returning to the previous position during the following morning) and 61% did not note any change.
More than a half of patients (53%) felt their teeth to be sensitive (lower anterior teeth through nocturnal grinding or clenching and upper anterior teeth through having to put up with the device).
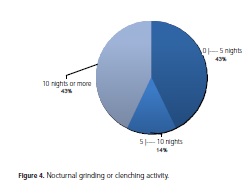
With regard to nocturnal activity: 49% grinded or clenched the teeth when using the device.
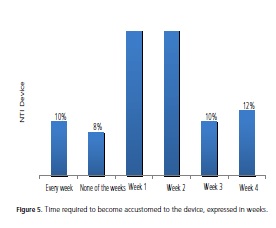
In relation to the time required to become accustomed to the device, the majority (72%) took one to two weeks, 10% took two to three weeks, 2% took three to four weeks, 2% took four to five weeks, 4% took five to six weeks and 10% were unable to get used to the device.
DISCUSSION
According to the results of this study, 71% of patients felt comfortable. Ekberg et al.12 showed, in their study, that 23% of patients in the treatment group and 30% in the control group complained of discomfort when using the splint. In the study by Magnusson et al.14, however, of the nine patients who used the NTI and the stabilizing splint, seven rated the stabilizing splint as more comfortable than the NTI. In two other comparative studies, the assessment was that they were similar: in Dahlström and Haraldson17, there was no statistical difference between the two groups evaluated (Hawley18 modified retainer and stabilizing splint) in terms of the discomfort index at the beginning of the study, however by the end, five patients in the Hawley18 modified retainer group rated it as being less uncomfortable, two as more uncomfortable and two did not alter their initial assessment. As for the group with the stabilizing splint, seven patients rated it as less uncomfortable, none as being more uncomfortable and three maintained their initial assessment. In the study by Jokstad et al.8, the degree of comfort with the use of the stabilizing splint and the NTI seemed to be similar, though the NTI did show a tendency to be more comfortable.
The explanation for 73% of patients not having removed the device during the night may be due to its comfortableness, it being recognized by the organism as an integral part of the occlusal/masticatory system.
The data in this study show that 88% of patients used the device every day, similar to the results found by Ekberg et al.12, where 83% of the treatment group and 77% of the control group said they had used the splint every or nearly every night.
A total of 70% of the patients enrolled in this study obtained greater relief in the first three weeks and ran no risk of complications as these risks are more prevalent in cases of mandibular advancement splints and in cases involving appliances with partial tooth coverage used for a period longer than four to six weeks without proper supervision7.
Regarding the change in bite (61% of patients did not note any change in their bite), there is quite a lot of controversy in the literature as the use of the splint could produce a change in muscle activity during the day4 and reduce the activity of the temporal muscle when swallowing, as well as releasing the mandibular in an antero-posterior manner for its repositioning10. The continuous use of this device could cause super-eruption of the posterior teeth, there being a risk of intrusion of the antagonist teeth. The patient should be advised to make a return visit to reevaluate the dental occlusion7,10,14-15.
One of the complaints with the use of the NTI is the sensitivity of the lower anterior teeth8. Side effects are rare and consist mainly of alterations in saliva flow (an increase or decrease) and a sensation of pressure on the teeth5, which is consistent with the data obtained in the present study which indicated that 53% of patients experienced some form of tooth sensitivity.
Practically one half of the patients (51%) did not grind their teeth when using the NTI device. This outcome serves to broaden the discussion on the topic since splints with or without occlusal coverage reduce muscle activity associated with nocturnal bruxism in 50% of instances19, and reduce electromyographic activity in the anterior temporal muscles, thereby reducing the total amount of nocturnal activity in patients with bruxism4. The incisal splint could significantly reduce muscle activity and should be used rather for the treatment of nocturnal clenching symptoms11. The recommendation to use the NTI could be justified to reduce activity of the muscles used in closing the lower jaw, or as an emergency device in patients with acute temporomandibular pain and with mouth opening limitations15.
During sleep, however, some patients perform greater parafunction with the splint than without it20, the parafunctional activity of nocturnal bruxism not stopping21. On the other hand, the study by Magnusson et al.14 states that the NTI maintained the clenching and grinding of the teeth that were recorded at the start of the treatment.
The majority (72% of patients) took from one to two weeks to get accustomed to using the device, differing from Clark et al.20 who alerted to the fact of the splint being a foreign body and that during the adaptation phase, in addition to the possibility of aggravated symptoms, some patients performed greater parafunction with the splint than without it, thereby making adaptation difficult.
Despite 88% of patients having used the device every night, there was a percentage of these patients who did not manage to use it throughout the whole night, removing it during this period. It is possible that different patients, when subjected to the same splint therapy present with different responses due to their adaptive ability, or on account of individual, intrinsic questions that are as yet not well understood.
As far as the TMD evaluation criterion is concerned, the literature contains a series of questionnaires that seek to assist the health professional. With the aim of creating universal standardization of results, that avoids conflicting diagnostic failures that could be perpetuated, Dworkin et al.16 created a protocol for standardizing clinical research related to Temporomandibular Disorders, by establishing an examination methodology. The present study, in order to establish meticulous, reliable results based on standardization, opted for RDC. Pettengill et al.22, Raphael and Marbach23 and Ekberg et al.12 also used this standard (RDC/TMD16). Selligman et al.24, Gesch et al.25 and Gesch et al.26 resorted to the use of the guidelines issued by the American Academy of Orofacial Pain. As for Dahlström and Haraldson17 and Magnusson et al.14, they used the Helkimo classification index; others made use of criteria such as those of Clark, used by Pullinger et al.27 and of Gutiwski, used by Celic et al.28.
The interocclusal device is a form of conservative therapy that produces favorable results with regard to TMD. Nevertheless, there are other mechanisms involved in the therapeutic response of this pathology which are as yet poorly understood29, or they could simply be the result of the placebo effect10.
It is necessary to carry out fresh research with a different methodology that makes it possible to isolate the effect of this device and to correlate the data on its use with the results of symptom control, as well as taking into consideration the TMD subtypes.
CONCLUSION
In accordance with the methodology employed in the present study, it may be concluded that, for the majority of patients, there was a high degree of satisfaction with the use of the NTI device.
Collaborators
LFR PEGADO and E GROSSMANN were responsible for implementing the methods and writing of the article. AS GUIMARAES was the creator of the work and participated in the writing of the article. LF PEGADO, FL SILVA were responsible for the literature review and writing of the article. AS GUIMARAES, E GROSSMANN attended the correction and article writing.
REFERENCES
1. Okeson JP. Fundamentos de oclusão e desordens temporomandibulares. 2ª ed. São Paulo: Artes Médicas; 1992. [ Links ]
2. Zarb GA, Carlsson GE. Temporomandibular joint: function and dysfunction. Copenhagen: Munksgaard; 1979. [ Links ]
3. Nelson SJ. Principles of stabilization bite splint therapy. Dent Clin North Am. 1995;39(2):403-21. [ Links ]
4. Boero RP. The physiology of splint therapy: a literature review. Angle Orthod. 1989;59(3):165-80. [ Links ]
5. List T, Helkimo M. Adverse events of acupuncture and occlusal splint therapy in the treatment of craniomandibular disorders. Cranio. 1992;10(4):318-24. [ Links ]
6. Clark GT. A critical evaluation of orthopedic interocclusal appliance therapy: design, theory, and overall effectiveness. J Am Dent Assoc. 1984;108(3):359-64. [ Links ]
7. Widmalm SE. Use and abuse of bite splints. Compend Contin Educ Dent. 1999;20(3):249-59. [ Links ]
8. Jokstad A, Mo A, Krogstad BS. Clinical comparison between two different splint designs for temporomandibular disorder therapy. Acta Odontol Scand. 2005;63(4):218-26. doi: 10.1080/00016350510019982. [ Links ]
9. Manns A, Miralles R, Santander H, Valdivia J. Influence of the vertical dimension in the treatment of myofascial paindysfunction syndrome. J Prosthet Dent. 1983;50(5):700-9. doi: 10.1016/0022-3913(83)90213-5. [ Links ]
10. Attanasio R. Intraoral orthotic therapy. Dent Clin North Am. 1997;41(2):309-24. [ Links ]
11. Omatsu S, Ishigaki S, Kajiwara K, Morishige E, Kurozumi T. 2332 Electromyographic evaluation of the effect of two types of occlusal splints on the muscle activity in the decubitus* position [cited 2010 Fev 15]. Available from: <http://www.nti-tss.com/Science/Japanese-NTI-study.html> [ Links ].
12. Ekberg E, Vallon D, Nilner M. The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. a randomized, controlled, short-term trial. J Orofac Pain. 2003;17(2):133-9. [ Links ]
13. Helkimo M. The Swedish Dental Association turned to the Swedish National Board of Health (Socialstyrelsen) [cited 2010 Fev 15]. Available from: <http://www.pdfio.com/k-1213794.html> [ Links ].
14. Magnusson T, Adiels A, Nilsson H, Helkimo M. Treatment effect on signs and symptoms of temporomandibular disorders: comparison between stabilization splint and a new type of splint (NTI). A pilot study. Swed Dent J. 2004;28(1):11-20. [ Links ]
15. Stapelmann H, Turp JC. O aparelho NTI-tss para terapia do bruxismo, desordens temporomandibulares e dor de cabeça: aonde estamos? Uma sistemática e qualitativa revisão da literatura. BMC Oral Health. 2008;8:22. [ Links ]
16. Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6(4):301- 55. [ Links ]
17. Dahlström L, Haraldson T. Bite plates and stabilization splints in mandibular dysfunction: a clinical and electromyographic comparison. Acta Odontol Scand. 1985;43(2):109-14. [ Links ]
18. Hawley CA. A removal retainer. Int J Orthod. 1919;5:291-9. [ Links ]
19. Dube C, Rompre PH, Manzini C, Guitard F, Grandmont P, Lavigne GJ. Quantitative polygraphic controlled study on efficacy and safety of oral splint devices in tooth-grinding subjects. J Dent Res. 2004;83(5):398-403.doi: 10.1177/154405910408300509. [ Links ]
20. Clark GT, Beemsterboer PL, Solberg WK, Rugh JD. Nocturnal electromyographic evaluation of myofascial pain dysfunction in patients undergoing occlusal splint therapy. J Am Dent Assoc. 1979;99(4):607-11. [ Links ]
21. Holmgren K, Sheikholeslam A, Riise C. Effect of a full-arch maxillary occlusal splint on parafunctional activity during sleep in patients with nocturnal bruxism and signs and symptoms of craniomandibular disorders. J Prosthet Dent. 1993;69(3):293-7. doi: 10.1016/0022-3913(93)90109-2. [ Links ]
22. Pettengill CA, Growney Junior MR, Schoff R, Kenworthy CR. A pilot study comparing the efficacy of hard and soft stabilizing appliances in treating patients with temporomandibular disorders. J Prosthet Dent. 1998;79(2):165-8. doi: 10.1016/S0022-3913(98)70211-2. [ Links ]
23. Raphael KG, Marbach JJ. Widespread pain and the effectiveness of oral splints in myofascial face pain. J Am Dent Assoc. 2001;132(3):305-16. [ Links ]
24. Seligman DA, Pullinger AG. Analysis of occlusal variables, dental attrition, and age for distinguishing healthy controls from female patients with intracapsular temporomandibular disorders. J Prosthet Dent. 2000;83(1):76-82. doi: 10.1016/S0022-3913(00)70091-6. [ Links ]
25. Gesch D, Bernhardt O, Kocher T, Jonh U, Hensel PE, Alte D. Association of malocclusion and functional occlusion with signs of temporomandibular disorders in adults: results of the population-based Study of Health in Pomerania. Angle Orthod. 2004;74(4):512-20. [ Links ]
26. Gesch D, Bernhardt O, Mack F, John U, Kocher T, Alte D. Association of malocclusion and functional occlusion with subjective symptoms of TMD in adults: results of the Study of Health in Pomerania (SHIP). Angle Orthod. 2005;75(2):179-86. [ Links ]
27. Pullinger AG, Seligman DA, Gornbein JA. A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J Dent Res. 72(6):968-79. [ Links ]
28. Celic R, Jerolimov V. Association of horizontal and vertical overlap with prevalence of temporomandibular disorders. J Oral Rehabil. 2002;29(6):588-93. doi: 10.1046/j.1365-2842.2002.00865.x. [ Links ]
29. Dao TT, Lavigne GJ. Oral splints: the crutches for temporomandibular disorders and bruxism? Crit Rev Oral Biol Med. 1998;9(3):345-61. doi: 10.1177/10454411980090030701. [ Links ]
 Correspondence to:
Correspondence to:
LFR PEGADO
Rua José Rocha Junqueira, 13, Swift, 13045-755, Campinas, SP, Brasil
e-mail: nekko@ig.com.br
Received on: 13/11/2009
Final version resubmitted on: 19/5/2010
Approved on: 9/8/2010













