Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.2 Porto Alegre Abr./Jun. 2013
ORIGINAL / ORIGINAL
Evaluation of the laboratorial processes' quality applied to titanium prostheses: plasma casting and laser welding - metallographic analysis
Avaliação da qualidade de processos laboratoriais aplicados nas próteses em titânio: fundição a plasma e soldagem a laser - análises metalográficas
Maria Cristina PEDRAZINI; Ronaldo Andrade Figueiredo OLIVEIRAI; Sandra FABIANOI; Antonio Marcos MONTAGNERI; Thomaz WASSALLI
I Faculdade São Leopoldo Mandic, Curso de Odontologia, Programa de Pós-Graduação em Implantodontia. Rua José Rocha Junqueira, 13, Swift, 13045- 755, Campinas, São Paulo, Brasil.
ABSTRACT
Objective
The aim of this study was to evaluate the quality of laboratory processes in titanium alloys.
Methods
Eight bars were cast using the voltaic arch technique. Three bars after casting were cut at three points and received, in total, nine laser welding points. All samples were analyzed under naked eye; 50X; 100X and 200X lens with electronic microscopy.
Results
All samples showed a perfect casting, without continuity solution or defects such as emptiness, bubbles, cracks, porosity or inclusions. The nine welding points didn't present any union failures, cracks or empty spaces and comparing this result with previous studies, there was improvement in the processes' quality.
Conclusion
The good quality observed in these laboratorial processes were due to the improvement of the technician's learning curve, observation of the laboratorial protocols, the correction of possible defects in the equipment used and the application of statistical process control (SPC).
Indexing terms: Dental casting technique. Dental soldering. Titanium.
RESUMO
Objetivo
Avaliar a qualidade de processos laboratoriais aplicados em ligas de titânio.
Métodos
Oito padrões em cera foram fundidos com o uso da técnica de arco voltaico. Três barras, após fundidas, foram cortadas em três pontos gerando nove pontos de solda com a técnica a laser. Todas as amostras foram analisados a olho nú e em aumento de 50x, 100x e 200x usando microscopia eletrônica - análise metalográfica.
Resultados
Todas as amostras apresentaram boa fundição, sem soluções de continuidade, sem falhas como vazios, bolhas, trincas, porosidades e inclusões. Os nove pontos de soldas a laser não apresentaram falhas de união, trincas ou vazios e comparando estes resultados com achados anteriores, houve melhora na qualidade dos processos.
Conclusão
Conclui-se que a boa qualidade observada nesta investigação dos processos laboratoriais do titânio se deve tanto a melhora na curva de aprendizagem dos técnicos, observação dos protocolos laboratoriais como também correção dos possíveis defeitos nos equipamentos utilizados como também ao controle estatístico do processo (CEP).
Termos de indexação: Técnica de fundição odontológica. Soldagem em Odontologia. Titânio.
INTRODUCTION
Oral Implantology is one of the areas in Dentistry that has most advanced and changed over the years. Today, the objective of treatment with implants is prioritizing ways of rehabilitation that meet the expectations of the patient, so that balance and stability of occlusion is re-established as well as esthetic and phonetic factors.
In view of this new project, all ways to prevent failures in the final rehabilitation must be sought.
Implant-supported rehabilitations have high success rates, nevertheless there are some unexpected problems, such as fractures of component, esthetic material and bars that are viewed with great discomfort by the professionals and patients involved.
More specifically, the bar fracture made with titanium (Ti) alloy is one of the most frequent causes of rework and it can be attributed to mistakes in dimensional calculations, long cantilevers, bad distribution of loads, or failures in laboratory processes1-2.
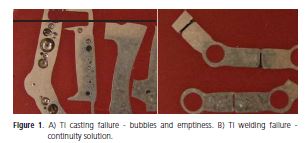
Failures were found in a study where the quality of laser welding and casting process were investigated in Ti and in Co-Cr (Figure 1a and 1b). The results left them with two uncertainties: one with regard to the quality of laboratory work received by prosthodontist who can't see internal failures in the castings and welds; and the second concerns the longevity of rehabilitation components containing failures, which are placed in patients1-2.
Titanium alloy is difficult to handle. It has a high melting point (around 2000°C), reacts with the investment, oxidizes easily, and requires special melting cycles with the protection of gases (argon) to prevent the contamination of the metal and oxygen reaction. As it has low density, it can't be cast in conventional centrifugal force machines, but in machines that combine centrifugal force with induction or those under vacuum, pressure and electrical arc. In relation to welding, this can only be performed with the use of laser, tungsten inert gas (TIG), or plasma as heat sources, protected by argon gas in special chambers3-4.
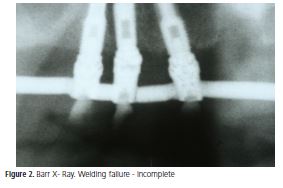
Considering radiographic evidence (Figure 2), clinical observation, the result of previous studies as well as doubts about what is acceptable and what is real failure, the aim of this study was to evaluate the quality of laboratory process under metallographic analysis5 and naked eye to establish whether or not the failures are inherent to the processes.
METHODS
An aluminum base, simulating a mandible where the bars were sculpted, with four stainless steel abutments was machined by the machinery company (Autocam do Brasil, Boituva, Brazil), for the laboratory assay.
The laboratory (in São Paulo, SP, Brazil) used in previous studies1-2 was contacted and alerted to the problems in that study, with the objective of reevaluating process quality. They received orientations about the necessities of the SPC program.
After this, eight bars measuring 3 mm in diameter and 6 cm long were sculpted to obtain the wax patterns that would be used for casting following the protocol (Dentaurum, Ispringem, Germany). Of the eight bars cast, three were cut, each one at three points, creating nine weld points by laser welding technique which were analysed together with the casting process. The samples (S) were sent for metallographic analysis where they were divided and embedded in bakelite phenolic resin (Arotec, Belo Horizonte, MG, Brazil), thus obtaining the body tests (BT) (Figure 3a).
Distribution of samples
Control group
a) 4 Ti pellets for casting made using industry foundry process (BT 1-2);
Test group
b) 3 bars cast in Ti, each one cut at three points and welded (casting analysis) (BT 3-4-5);
c) 9 welding points on bars cast, cut and welded (welding analysis) (BT 3-4-5);
d) 5 bars cast in Ti (casting analysis) (BT 6-7- 8) **
** The bodies test 6 and 7 with two bars inside
Obtaining the bars
The bars were obtained by waxing with Star Wax (Dentaurum, GE). An electric wax dropper was used to melt the wax. Axis cylinders (Dentaurum, GE) measuring 3 mm in diameter were used to join one coping to the other. The sprues (Dentaurum, GE) used were the same diameter, 3 mm. On the finish, wax patterns measuring 3 mm in diameter and 6 cm long, received a treatment with tensoactive agent (Dentaurum, GE).
Titanium casting
Tritan brand pellets (Dentaurum, GE) containing 99.5% Ti, the rest being Fe, O, H, N, and C were used for casting. The wax pattern was embedded in a ring with Rematitan Ultra Investment (Dentaurum, Germany). The set was heated in a conventional furnace at 850º C, in which the wax was volatilized. The mold was created, and was cooled in the same furnace until 430ºC, when it was taken to the casting machine protected with argon gas atmosphere (AutoCast, Dentaurum, GE). Ti pellets were melted at 1668°C inside the copper crucible by the action of non-consumable tungsten electrode that generate alternating current (voltaic arc or plasma technique), and liquefied metal was injected under vacuum and pressure inside the machine itself.
Titanium welding
Ti was performed with the welding machine (Desktop DL20002s, Dentaurum, GE) that uses a Nd:YAG crystal as a source of laser and the stereomicroscope reticulated lenses that aid in the alignment of the light. The bars were placed on the mandible model and taken to the chamber protected with an argon gas atmosphere that diminishes oxidation. A titanium wire was used with the same composition and from the same manufacturer of the alloy used (Dentaurum, GE) in the spaces between the parts to be welded. Small amounts of wear occured during sectioning.
Metallographic analysis
The metallographic analysis was performed by Autocam do Brasil, Brazil.
Each body test was submitted to a grinding process in the longitudinal direction every 1 mm. They were then polished in a polishing machine (Arotec, Brazil) with abrasive papers grits 120; 200; 400; 600 and lastly, with a felt disk and diamond paste.
The analyses were performed by an electronic microscope (Olympus BX51M, São Paulo, Brazil) capable of 1000x magnification, coupled to the camera (Evolution CLC Fuji Film, São Paulo, SP, Brazil) that sent the images directly to a computer where they were stored. The photographs were taken with naked eye; at 50X; 100X and 200X magnification.
Each body test was subsequently etched with Kroll's reagent (6ml HNO3, 3ml HF and 1000ml H2O) which is indicated for micrographic evaluation of titanium and its alloys. The reagent (100 ml) was placed in a Beaker cup. Each (BT) was immersed for eight minutes in the solution, at room temperature, approximately 24°C. After drying, other photos were taken.
RESULTS
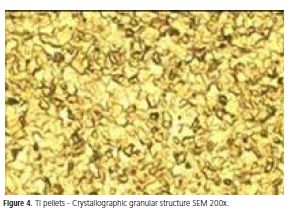
The control group formed by Ti pellets showed no failures and metallographic analyses with Kroll's reagent revealed that Ti pellets could have received a heat treatment that stabilized the crystals showing a granular structure, which suggests a more resistant structure (Figure 4).
The eight bars cast showed no failures visible to the naked eye (Figure 3a). At 200X magnification, after being etched with Kroll's reagent, it revealed a new crystallographic structure with the formation of dendrites, inherent to the process (Figure 3b). All the samples had a homogeneous structure, no continuity solution, bubbles or empty spaces.
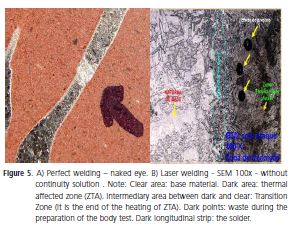
The nine weld points, three points on each bar, showed no defects visible to the naked eye (Figure 5a). At 100X magnification, the weld points showed good continuity of the metal, complete filling of the sectioning line, and a good coalition between base metal (MB) and addition metal (MA) (Figure 5b).
The results were described based on the observations of the body tests by the researchers, as well as in the technical conclusion of the analyses by Autocam.
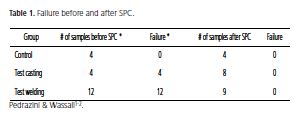
The data described in the Table 1 shows the absence of the flaws and it compares with previous works1-2.

DISCUSSION
In view of the affirmation that the laboratorial processes, casting and welding, must maintain the metal's continuity6 and the homogeneity of the physical, structural and mechanical properties7-8, all failures should be investigated and corrected.
The welding procedure is necessary for uniting the cast parts that were cut into sections after casting, and also for maintenance of extensive bars when fractured9. The laser technique can be applied in these cases to maintain the continuity of the metal, the homogeneous and compact structure, and an interface bar/weld without defects or porosity10.
Remembering that Ti alloy can only be welded by special techniques, but never by the torch brazing process3-4, it is noteworthy that the term "brazing" is not applied to laboratory processes used in Dentistry and the most adequate term to be used for joining metallic parts is "welding", irrespective of the heat source11-12.
The failures in laboratory processes, in general, are divided into errors caused by the low technician's learning curve and/or by failures of the material and the equipment used13. Although simple and used routinely in dental prosthesis laboratories, all the processes should be done strictly following the protocol procedures, so that precise, well fitting, and resistant metal structure can be obtained14.
The failures found in the casting processes2 are summarized in: "emptiness", caused by feeding channels with inadequate measures or in incorrect positions; "segregation", equipment without maintenance with alloys' remains; "fissures" or "cracks", and "bubbles", caused by a film of water in the coating, or gas inside the league15. To control the "superficial porosity", temperature differences should be reduced, heating the mold an additional 100º C to 150º C to receive the liquefied alloy7. The origin of "distortion" could be in the wax pattern or metal contraction, and "incomplete casting" may occur due to incomplete elimination of the wax, which hinders the mold from being completely filled with metal16-17. Even so, if everything is controlled, the result of cast work is acceptable, with a homogeneous structure, a fact also observed in this work.
The union point between metal parts can not present a discontinuity of physical and mechanical properties18. It must have a homogeneous and compact structure, without defects at the bar and weld interface, and be free of porosities10,19.
The technical viability of the equipment used must be observed20.
The incomplete welding of the laser technique observed in works before1 can be attributed to the sophisticated equipment used and complex technique.
The depth of penetration of the laser bunch must be corrected adjusting the voltage associated to the pulse and not the pulse's duration. It's necessary to observe the application angle of the laser's bunch and clean the stereomicroscope reticulated lenses that aids in the alignment of the light bunch with the components to be welded4,11,21-22.
In relation to penetration's depth of the laser bunch, there was not a consensus. The literature says from 1,5mm to 2,5mm of penetration21 concluding that the metal thickness can vary from 3mm to 5mm. However, other authors described that the metal thickness recommended could vary from 2,4mm to 3mm11,22.
In general, the weld points investigated in this work were shown to be perfect because all the factors that could generate problems mentioned above were controlled.
The results presented in this study show that if the technicians are trained and capable of manipulating sophisticated equipment, if the equipment is calibrated and in perfect condition, and if all necessary precautions are followed, that is to say, if the administrators are attentive to the needs of statistical process controls (SPC), the results are translated in quality pieces.
It is important to point out that these failures may not be the causes of fractures in the prosthetic parts. Excessive loads, mistaken dimensional calculations related to biomechanics, as well as inadequate materials, are also causes of fractures5.
CONCLUSION
The conclusion of this work corroborates with previous researchers conclusions: lowers learning curves and flaws in the equipment are the main causes of the flaws in the processes.
Ti alloy presents a good welding quality with the laser technique and accepts a good casting with voltaic arc technique, concluding that flaws are not inherent to the processes.
If the laboratories apply the SPC program regularly, following the laboratory protocols and maker's orientations; training technicians and finally, checking the equipment calibration, this will be translated in quality works and consequent satisfaction of those involved: technicians, prosthodontist and patients. New randomized studies must be done with larger samplings.
Acknowledgements
We thank Messrs. Eduardo Renner de Castilho, Luiz Fernandes Gonçalves, Walter Winckler, and Ms Fátima Mariano of Autocam do Brasil, a high precision machining company, for their cooperation with the metallographic analysis. Our gratetude also to Mr. Edward Hekman and Mrs Lark Meadows D'Auria for the revision of this manuscript.
Collaborators
MC PEDRAZINI, RAF OLIVEIRA, S FABIANO, AM MONTAGNER and T WASSALL participated in all stages of the article.
REFERENCES
1. Pedrazini MC, Wassall T. Avaliação in vitro das falhas nas uniões soldadas à laser nas infra- estruturas de Ti e Co-Cr para próteses sobreimplantes. ImplanteNews. 2008;5(5):529-35. [ Links ]
2. Pedrazini MC, Wassall T. Falhas de fundição nas estruturas de próteses ferulizadas sobre implantes: ensaio en vitro. RGO - Rev Gaúcha Odontol. 2009;57(2):165-172.
2. Wiskott HW, Macheret F, Bussy F, Belser UC. Mechanical and elemental characterization of solder joints and welds using a gold-palladium alloy. J Prosthet Dent. 1997;77(6):607-16. doi: 10.1016/S0022-3913(97)70103-3.
4. Anusavice KJ. Phillip's science of dental materials. 10 th. Chicago: Guanabara Koogan; 1998.
5. Colpaert H. Metalografia dos produtos siderúrgicos comuns. São Paulo: Edgar Blücher; 1951.
6. Craig RG, Powers JM, Wataha JC. Materiais dentários: propriedades e manipulação. 7ª ed. São Paulo: Santos; 2002.
7. Gabrielli ACR, Cartise ABE, Panzeri H. Emprego da soldagem TIG (Tungstein Inert Gas) em ligas para uso odontológico contendo níquel, cobalto e titânio. RPG Rev Pós Grad. 2000;7(3):253-8.
8. Kappert HF. Schweiben mit plasma und laser. Quintessenz Zahntech. 1991;17:977-98.
9. Anusavice KJ. Materiais dentários. 11ª ed. Rio de Janeiro: Elsevier; 2005.
10. Manicone P, Valentini G, Raffaelli L, Raffaelli R. Titanium joints welded with laser and infrared techniques: comparative analysis of its microstructure. Minerva Stomatol. 2000;49(10):463-74.
11. Craig RG, Powers JM. Materiais dentários restauradores. 11ª ed. São Paulo: Santos; 2004.
12. Araujo PA, Abreu D, Netto JC. Materiais dentários II: metálicos. 3ª ed. Bauru: FOB-USP; 1978.
13. Patterson EA, Johns RB. Theoretical analysis of the fatigue life of fixture screws in osseointegrated dental implants. Int J Oral Maxillofac Implants. 1992;7(1):26-33.
14. Martignoni M, Schönenberger A. Precisão em próteses fixas: aspectos clínicos e laboratoriais. 2ª ed. São Paulo: Santos; 2001.
15. Zequetto MM, Silva EMM, Zuim PRJ, Rocha EP, Assunção WG. Falhas no processo de fundição que levam ao insucesso das próteses parciais fixas. Rev Bras Odontol. 2005;62(1-2):39-41.
16. Ryge G. Dental soldering procedures. Dent Clin North Am. 1958;2:747-57.
17. Wainer E, Brandi SD, Mello FDH. Soldagem: processo e metalurgia. São Paulo: Edgar Blucher; 1992.
18. Bergendal B, Palnquist S. Laser-welded titanium frameworks for fixed prostheses supported by osseointegrated implants: a 2 year multicenter study report. Int J Oral Maxillofac Implants. 1995;10(2):199-206.
19. Bezerra RM, Souza PCRD, Ramires I, Bottino MA, Guastaldi AC. Microestrutura e resistência à corrosão do Ti c.p. soldado a laser utilizando em próteses sobre implante. Eclet Quím. 1999;24:113-124.
20. El-Ebrashi MK, Asgar K, Bigelow WC. Electron microscopy of gold soldered joints. J Dent Res. 1968;47(1):5-11. doi: 10.1177/00220345680470012601.
21. Tambasco J, Anthony T, Sandven O. Laser welding in the dental laboratory: an alternative to soldering. J Dent Tecnol. 1996;13(4):23-31.
22. Pfluger AR, Lewis RE. Weld Imperfections: proceedings of a symposium at Lockheed Palo Alto Research Laboratory. California: Addison Wesley Publishing Company; 1966.
 Endereço para correspondência:
Endereço para correspondência:
MC PEDRAZINI.
e-mail: mcpequipe@sigmanet.com.br
Received on: 20/6/2012
Final version resubmitted on: 23/10/2012
Approved on: 22/11/2012













