Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.2 Porto Alegre Abr./Jun. 2013
ORIGINAL / ORIGINAL
Denture hygiene: importance in denture stomatitis control
Higiene de próteses dentárias: importância no controle da estomatite protética
Laís César de VASCONCELOSI; Laurylene César de Souza VASCONCELOSII; Eloisa Lorenzo de Azevedo GHERSELII; Dejanildo Jorge VELOSOII; Paula Ângela Souto Montenegro de Almeida CUNHAII
I Universidade Federal da Paraíba, Programa de Pós-Graduação em Odontologia. Cidade Universitária, 58051-900, João Pessoa, PB, Brasil.
II Universidade Federal da Paraíba, Departamento de Clínica e Odontologia Social. João Pessoa, PB, Brasil.
ABSTRACT
Objective
To assess the denture hygiene for denture stomatitis control and establish a protocol for the cleaning these appliances.
Methods
From the population of prosthesis users assisted by the Integrated Clinics Subject taught at the Federal University of Paraiba, Brazil, 45 people were selected for convenience. Aspects related to the hygiene of the prosthesis, clinical characteristics of the lesion as well as candidosis diagnosis were evaluated before and after the protocol had been established for prosthesis hygiene. Data were collected through questionnaires, medical history, clinical and prosthesis examinations and analyzed using descriptive and inferential statistics.
Results
There was a statistically significant difference (p <0.001) to the level of prosthesis hygiene between the first and second examination. Regarding the type of injury, there was increased frequency of patients without lesions and reduction of positive mycological results.
Conclusion
The cleaning protocol for dentures was effective in both controlling the prosthesis biofilm as contributing to the reduction of clinical signs of denture stomatitis lesions.
Indexing terms: Dental prosthesis. Health education, dental. Oral hygiene. Stomatitis.
RESUMO
Objetivo
Avaliar a higiene das próteses para o controle da estomatite protética e instituir um protocolo de higienização desses aparelhos.
Métodos
Do universo constituído pelos usuários de prótese atendidos na Disciplina de Clínica Integrada do Hospital Universitário Lauro Wanderley - Universidade Federal da Paraíba, Brasil, foram selecionadas, por conveniência, 45 pessoas. Foram avaliados aspectos relacionados à higiene da prótese, características clínicas da lesão e diagnóstico de candidose antes e depois de instituído o protocolo de higiene da prótese. Os dados foram levantados através de questionários, anamnese, exame clínico e da prótese. Os dados foram avaliados através de estatística descritiva e inferencial (testes de Wilcoxon e Qui-Quadrado).
Resultados
Observou-se uma diferença estatisticamente significativa (p<0,001) em relação ao nível de higiene das próteses entre o primeiro e o segundo exame. Na mesma perspectiva, quanto ao tipo de lesão, houve um aumento na frequência de pacientes sem lesão e redução de resultados positivos no exame micológico, considerando o resultado do segundo exame.
Conclusão
A instituição do protocolo de higienização das próteses mostrou-se eficaz, tanto no controle do biofilme da prótese como também contribuiu para a redução dos sinais clínicos das lesões de estomatite protética.
Termos de indexação: Prótese dentária. Educação em saúde bucal. Higiene bucal. Estomatite.
INTRODUCTION
The Brazilian population pyramid has been modified over the past years because of iincreasing life expectancy and therefore the population aging. Much of the current elderly population has undergone an essentially curative dentistry, where the practice of extraction was the main therapeutic procedure, reason why most of the elderly are users of dentures, or need to use them1. The increase in demand for health care, including oral health, can eventually lead to an overload on public health systems2. Still, it is important to consider that this population needs better living conditions being the oral health a contributing factor, which promotes their welfare3.
There is a correlation between the precariousness of oral health of patients with complete dentures, poor hygiene and oral mucosal lesions and the highest incidence of denture stomatitis. The lack of oral hygiene care may trigger certain diseases, which induce burning, pain and thus discomfort to the patient, as in the case of candidosis and stomatitis4.
Barbeau et al.5, described the denture stomatitis as an inflammatory process primarily involving the palate mucosa when it is fully or partially covered by the denture. The etiology seems to be multi-parametric: advanced age and concomitant decline of the defense immune system, systemic diseases, smoking, use of prosthesis to sleep and poor oral hygiene, resulting in denture plaque accumulation.
The prevalence of denture stomatitis is high among individuals with unhealthy lifestyle, with high counts of lactobacilli and also among people with poor oral hygiene. The presence of fungi was shown to be related to the volume of salivary secretion, the smoking habit, dietary habits and alcohol consumption6.
Unlike the other candidosis, stomatitis induced by use of prosthesis does not show plaque formation, but especially the proliferation of Candida albicans at the interface between the mucosa and dentures, being related to the fungi adherence of the resin base7. According to Girard Jr et al.8, the adhesion force of Candida albicans to the prosthesis surface is linked to the presence of plaque, and not only the yeast-acrylic resin interaction. The plaque formed by Streptococcus mutans in the presence of sucrose would be, in the opinion of these authors, an essential factor for the fungal adherence, causing the clinically observed inflammation
The diagnosis of denture stomatitis is based mainly on the clinical examination; nevertheless, confirmatory laboratory tests are very important. The clinical diagnosis is essential, being performed through a correct and complete medical history and clinical history of injury It is also fundamental to know the level of oral and prosthetics hygiene, as well as the remaining situation of the teeth elements9.
The etiology detection of denture stomatitis, followed by appropriate treatment leads to lesion regression and success of the therapy. The treatment of denture stomatitis involves measures such as oral and prostheses hygiene: avoiding the use of dentures overnight, placement of prosthetic in substances such as chlorhexidine or sodium hypochlorite and the antifungal therapy.
While proposing better ways of cleaning the prosthesis, this should always be based on previous oral hygiene education of the patient and, from these data, incorporate methods for maintaining hygiene fitted to the new reality10.
The participation of the dentist is essential to control the local factors triggering stomatitis related to wearing dentures, which must be explicitly clear in the guidelines regarding the use and cleaning of prosthesis by the patient11.
Taking into account that poor denture hygiene and long-term use are considered decisive factors for the development of denture stomatitis, it is necessary therefore to establish hygienic procedures and maintenance of dentures as supporting tools in this disease treatment, contributing to the improvement of oral health status of patients using prostheses through preventive as well as therapeutic procedures. The present study aimed to evaluate the effectiveness of cleaning the prosthesis in the biofilm control through guidance related to the correct procedures for prostheses cleaning and maintenance and also performing the diagnosis and treatment of candidoses among patients with denture stomatitis.
METHODS
The research was initiated after approval by the Ethics Committee in Research of Lauro Wanderley University Hospital - Federal University of Paraíba, Brazil (protocol 289/10). The realm consisted of patients who sought treatment at the Discipline of Integrated Clinic of the School of Dentistry. All patients were instructed about the study and signed a consent form to authorize the participation in the survey - Resolution 196/96 from the National Health Council.
As a condition to participate in the experiment the following criteria were established: patients using prostheses (total or partially removable with palatal coverage) with or without a clinical diagnosis of denture stomatitis (Newton's classification)12 and patients with or without candidoses. The sample consisted of 45 individuals,age range between 50 and 75 years old.
The data relating to the history of patients were properly set down in medical records. Data relating to the prosthesis use, such as manufacture time and frequency of cleaning were also raised by means of form.
The cleaning was evaluated against the presence or not of biofilm on any area of the prosthesis. On the first meeting, the upper prosthesis of participants in the study group were removed from the oral cavity and, in order to determine the plaque index, the prosthesis surface which is in contact with the palatal mucosa was stained with a solution in order to verify the amount of biofilm present on it (Replasul T - Iodontosul®, Porto Alegre, Brazil). The plaque index, recommended by Ambjornsen et al.13, was used with modifications. The stained surface was divided into six parts, and the record corresponding to each of them was made in proper form, according to the codes and the following criteria: 0 - no plaque, 1 - small plaque areas, 2 - less than half covered by plaque, 3 - more than half covered by plate; 4 - entire area covered by plaque. The scores assigned to each segment were added and the resulting value indicated the level of hygiene: good (less than 9), reasonable (between 9 and 15), precarious (over 15). After summing up the values the participants received new guidelines and training related to the cleaning and maintenance of the apparatus.
All participants were given guidelines regarding the use of dentures, cleaning methods (brush and mild soap), means of preservation and maintenance, useful lifetime and consequences of prolonged prosthesis use. Regarding the oral care, the patient was instructed about the importance of removing the prosthesis at night, cleaning the rim with damp gauze, and also brushing the tongue. After showing patients the presence of the biofilm on the prosthesis surface, the cleaning was performed with the use of pumice paste and rubber cup coupled to the handpiece.
The clinical diagnosis of denture stomatitis was provided by observing the signs of mucosal erythema according to the three stages of classification described by Newton12: punctiform hyperemia (type I), diffuse hyperaemia (type II) and nodular hyperplasia of the area covered by the denture (type III).
Patients with clinical signs of denture stomatitis were referred for mycological examination (Clinical Laboratory - Lauro Wanderley University Hospital), according to the methodology in mycological routine, and according to laboratory protocol. Once diagnosed the candidoses, antifungal therapy with Miconazole (Daktarin® oral gel, Janssen-Cilag Farmacêutica Ltda., São José dos Campos, Brazil) was prescribed. Patients were required to apply the medication on the prosthesis surface which remains in contact with the palate mucosa three times a day, after the prosthesis hygiene, for 15 days.
One month after the first measurement, a new evaluation of the biofilm amount present was performed. All members participated in this stage, where the same procedures previously conducted were performed. At this stage of the study, the educational treatment was evaluated by observing whether the prosthetic hygiene had improved, as well as the possible stomatitis regression and mycoflora suppression through the mycological examination.
Data were registered in a database on the SPSS program (Statistical Package for Social Sciences) for Windows®, version 15.0, and analyzed using descriptive and inferential statistics. For the descriptive procedures the raw and relative data (frequencies and percentages) were presented. Afterwards the procedures of statistical inference were performed based on non-parametric statistics using the Wilcoxon test, chi-square and calculating the Cramer's V coefficient. For interpreting the information, the range of 95% and at 5% significance was adopted (p <0.05).
RESULTS
In order to compare the evaluations of the first and second tests, data were subjected to the Wilcoxon test., Regarding the prosthesis hygiene level, it was initially found that the gradations "reasonable" and "precarious" decreased from the first to the second examination, while the level "good" was higher in the second test. This difference is statistically significant (p <0.001). In the same context, regarding the type of lesion found , there was reduction in the number of patients with Type I, II and III lesions, so that the frequency of patients with no lesion in the second test was higher showing significant difference from the statistical point of view.
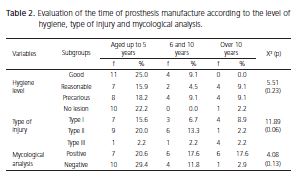
Finally, the results of the mycological analysis of two tests were compared and it was found that the number of positive results in the first examination was higher than the result in the second test. This difference between the examinations was considered statistically significant (p <0.001). The descriptive and inferential data related to this information are detailed in Table 1. The time of prosthesis manufacture was also assessed depending on the variables: hygiene level, type of injury and mycological analysis. Regarding the first variable, despite the frequency of patients over 10 years of prosthesis manufacture at the precarious and reasonable levels having been observed, statistical association (p = 0.23) cannot be estimated. Similarly, regarding the type of injury, even though it was observed a greater quantity of people up to five years of prosthesis manufacture without injury, this combination was not considered significant according to the statistical criteria (p = 0.06). The latter variable faced with the time of prosthesis manufacture was the mycological analysis, and there were no statistically significant correlations among variables (similarly to previous results) according to descriptive and inferential data presented in Table 2.
Finally, the daily frequency of the prosthesis hygiene was evaluated. Concerning the level of hygiene, it was found that people who perform the hygiene three times a day have good (20.5%), reasonable (18.2%) and precarious (18.2%) levels at equivalent proportions, so that the association among variables (p = 0.80) cannot be estimated. 
DISCUSSION
The increase in the elderly population group is a well described phenomenon in Brazil as well as worldwide. The higher the population's average life span, the more important the life quality concept in which oral health has an important role. Oral health impairment can affect nutritional status, physical well-being and mental health and deprive the joy of having active social life,as well. One of the main consequences of the precariousness of oral health is the high rate of total edentulism found among the elderly, being the treatment with conventional total dentures the most common means for rehabilitation of these patients. However, it is worth noting that the elderly not only seeks the replacement of missing teeth, but also decent dental treatment that allows redoing the personal and social image14. Considering the patients' age range in this study (50-75 years old), we face a sad reality in which an elderly population with multiple tooth loss. Even more worrying is the fact that users of inadequate prosthetic devices (poor hygiene and function) require at the outset better targeting and monitoring of their oral health. Public health actions should be aimed towards oral hygiene education, in order to increase the patient's awareness and acknowlegement of denture stomatitis clinical signs2. The prevalence of denture stomatitis and the associated risk factors differ in several studies, mainly due to the differences in the research methodology (age and dental status of the study group, patients treated in dental schools, institutionalized or not institutionalized patients, statistical analysis and subjectivity of the classification)15.
Almeida Júnior et al.16 aiming at getting to know methods and hygiene habits of users of removable prosthesis, observed that regarding the frequency of cleaning the dentures, 77% of patients reported sanitize it three or more times a day. Whereas the level of prosthesis hygiene may be related to the cleaning frequency of these prostheses by the patient, it was found in this study however, that patients presenting good, reasonable or precarious level of prosthesis hygiene reported performing the cleaning three or more times a day. This finding may be related to the fact that either the patients, despite repeatedly prosthesis hygiene, did it in the incorrect manner or were afraid of revealing the actual frequency of cleaning the dentures.
In this study, when considering the prostheses manufacture time, there was no relationship with the level of hygiene, or with mycological analysis results or the aspect of the lesion found in the patient's palate (Table 2). These results corroborate those found in the study of Oliveira et al.17, when it was observed that the positive diagnosis of denture stomatitis did not correlate with the number of patients whose dentures had many years of use. However, it is important to note that the use of old dentures, without balanced occlusion, can cause trauma to the palatal mucosa, promoting reduction in tissue resistance to fungal infection. According to Castro et al11 the presence of microorganisms, especially Candida albicans, can certainly be enhanced by the prolonged prosthesis use. This fact has shown that the continuous use of prosthesis causes degeneration of the palatine salivary glands and reduced salivary secretion, favoring the accumulation of microbial plaque which in turn causes reduction in salivary pH and consequent fungal proliferation by assisting mechanical, chemical or biological triggering factors that combined during long periods of uninterrupted use of prosthesis, induce the emergence the lesions.
Thiele et al.18 performed a study on elderly patient users of dentures aiming at evaluating the severity degrees of denture stomatitis, predisposing factors, counts of salivary fungal burden and virulence factors of Candida species. This study concluded that there was no significant participation of the histolytic enzymes studied in the development of denture stomatitis and denture hygiene habits and the state of its conservation have a greater significance and clinical relevance.
It is believed that the level of oral and denture hygiene is also a determining factor for the development of denture stomatitis, since the lack of hygiene promotes the accumulation of plaque, and therefore of bacteria and fungi on the prosthesis surface which is in contact with the mucosa. In the opinion of Barbachan et al.19 and Vasconcelos et al.7, the environment beneath the prosthesis, where the mucosa is not exposed to grooming, plus the presence of plaque, turns the mucosa susceptible to infection, which aggravates the local inflammation.
Concerning the percentage representation of the levels of prosthesis hygiene after the first disclosure of the biofilm, a greater number of prosthesis with high levels of hygiene considered as reasonable or precarious (Table 1) was demonstrated, which shows the extremely high degree of patients' misinformation concerning standards of oral and prostheses hygiene. These results are in agreement with the studies of Vasconcelos et al.20 and Kossione15, who observed the abundant presence of biofilm and calculation coating the prosthesis surface characterizing a precarious patients' oral hygiene.
Silva-Lovato et al.21, while evaluating the hygiene educational level in denture users, observed that 80% of patients received no guidance regarding the prosthesis hygiene in 1989. 15 years later in 2004, researchers noted a significant improvement in this feature when 52% of patients had no guidelines. For the authors, although the level of education has improved over the years, the oral hygiene of denture users is even precarious, requiring greater attention to these patients' oral health. The evaluation on the denture hygiene of patients before and after hygiene guidelines was performed in this study. In the procedure of cleaning the prosthesis, patients were instructed to use toothbrush, preferably hard, coconut soap and then wash it under running water always after meals, in addition to remove it during the night. There was increased level of hygiene considered as good in this interval, ranging from 34.1% to 75.6%, and the consequent reduction in the levels considered as reasonable and precarious (Table 1), confirming that education is a key factor for acquiring most effective hygiene habits.
In denture stomatitis, candidosis may be first connected with the contamination of the inner surface of the prosthesis by fungi, Candida albicans in particular. This yeast by itself is not capable of inducing this change. There must be other local or general factors correlated, predisposing to the development of local pathological change20. Mycological analysis of the different types of injuries presented by patients in this study showed positivity for fungi of genus Candida and the albicans species, and there was significant percentage reduction in the mycoflora between the first and second mycological examinations (Table 1). Food debris, located between the denture and the gums or between the prosthesis and the palate permit the multiplication of bacteria and Candida species causing the denture stomatitis. The interactions between oral bacterial microbiota and Candida albicans are important in the formation of fungal-bacterial biofilms of the prosthesis. Among the virulence factors of Candida albicans, such as adherence, interference with the host defense system, synergism with bacteria and production of hydrolases or metabolites, those considered of greater importance are the adherence and persistence22, in addition to releasing the yeast antigens and toxins present in the prosthesis biofilm2.
After establishing the prosthesis hygiene protocol used in this study, there was improvement of clinical appearance overall in the three types of injury, which influenced the increase of 35.6% of patients without lesion between the first and the second examinations (Table 1). Castro et al.11 suggest that suspending the use of denture associated with proper oral hygiene allows rapid healing of the area affected by the stomatitis in denture users. For Catão et al.14 and Ribeiro et al.23, it is reasonable to recommend the monitoring of prosthesis hygiene for patients in order to show the current condition of their dentures hygiene and objectives to be achieved regarding the cleaning of the prosthetic equipment through regular dental check-ups. It is believed therefore, being essential the participation of the dentist as a motivator in the development of hygiene habits by the patient regarding the prosthesis as an integrative care feature for this group of individuals.
CONCLUSION
The institution of the dentures hygiene protocol was effective both in controlling the prosthesis biofilm as well as contributing to the reduction of clinical signs of denture stomatitis lesions. The guidance for the correct procedures of oral hygiene, cleaning and maintenance of the prostheses were assimilated by patients, which contributed greatly to the satisfactory results obtained in this study.
The diagnosis of candidiasis and the institution of drug therapy were effective as adjunct in the treatment of stomatitis related to the use of prostheses in the study group.
Collaborators
LC VASCONCELOS and LCS VASCONCELOS contributed substantially in the conception and design of the study and data collection. ELA GHERSEL participated in the data collection. DJ VELOSO e PASMA CUNHA participated in the analysis and interpretation of data. All authors contributed significantly in drafting the manuscript and revising it critically with the content. Finally, all authors approved the final version of the manuscript to be published.
REFERENCES
1. Moimaz SAS, Santos CLV, Pizzato E, Garbin CAS, Saliba NA. Perfil de utilização de próteses totais em idosos e avaliação de eficácia de sua higienização. Ciênc Odontol Bras. 2004;7(3):72- 8. [ Links ]
2. Santos CM, Hilgert JB, Padilha DMP, Hugo, FN. Denture stomatitis and its risk indicators in south Brazilian older adults. Gerodontology. 2010;27(2):134-40. doi: 10.1111/j.1741- 2358.2009.00295.x.
3. Oliveira RC, Brum SC, Oliveira RS, Goyatá, FR. Aspectos clínicos relacionados à estomatite protética. Int J Dent. 2007;6(2):51-4.
4. Saliba NA, Moimaz SAS, Garbin CAS, Brandão IG, Casitho, AP. Manual para conservação de prótese dentária. Araçatuba: UNESP; 2001.
5. Barbeau J, Séguin J, Goulet, JB, de Koninck L, Avon SL, Lalonde B, et al. Reassessing the presence of Candida albicans in denture-related stomatitis. Oral Surg Oral Med Oral Pathol. 2003;95(1):51-9. doi: 10.1067/moe.2003.44.
6. Sakki TK, Knuuttila ML, Laara E, Anttila SS. The association of yeasts and denture stomatitis with behavioral and biologic factors. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(6):624-9. doi: 10.1016/S1079-2104(97)90363-2.
7. Vasconcelos LCS, Sampaio MC, Sampaio FC, Higino JS. Use of punica granatum as an antifungal agent against candidosis associated with denture stomatitis. Mycoses. 2003;46(5-6):192- 6. doi: 10.1046/j.1439-0507.2003.00884.x.
8. Girard Jr B, Landry RG, Giasson L. La stomatite prothétique: etiologie et condérations cliniques. J Can Dent Assoc. 1996;62(10):808-12.
9. Vasconcelos LCS, Sampaio MCC, Costa LJ. Tempo de uso e higiene das próteses em portadores de estomatite protética. Rev Bras Ciênc Saúde. 2003;7(1):25-32.
10. Pinelli LAP, Marra J, Fais LMG, Silva RHBT, Guaglianoni, DG. Análise da condição de higiene oral de pacientes usuários de prótese parcial fixa. ROBRAC. 2007;16(42):1-6.
11. Castro AL, Furuse TA, Gaetti-Jardim Júnior E, Castro, EVFL, Jardim, PTC, Paro, MLC. Estomatite protética induzida pelo mau uso de prótese total: caso clínico. Rev Fac Odontol. 2006;27(2):87-90.
12. Newton AV. Denture sore mouth: a possible ætiology. Br Dent J. 1962;102(1):357-60.
13. Ambjornsen E, Rise J, Haugejorden A. A study of examiner error associated with measurement of denture plaque. Acta Odontol Scand. 1984;42(3):183-91.
14. Catão CDS, Ramos INC, Silva Neto JM, Duarte SMO, Batista AUD, Dias AHM. Chemical substance efficiency in the biofilm removing in complete denture. Rev Odontol UNESP. 2007;36(1):53-60.
15. Kossione AE. The prevalence of denture stomatitis and its predisposing conditions in an older Greek population. Gerodontology. 2011;28(2):85-90. doi: 10.1111/j.1741- 2358.2009.00359.x.
16. Almeida Júnior AA, Neves ACC, Araújo CCN, Ribeiro, CF, Oliveira, JLG, Rode SM. Avaliação de hábitos de higiene bucal em portadores de próteses removíveis da Faculdade de Odontologia da Universidade Federal de Sergipe. Comum Ciênc Saúde. 2006;17(4):283-9.
17. Oliveira TRC, Frigerio MLMA, Yamada MCM, Birman EG. Avaliação da estomatite protética em portadores de próteses totais. Pesqui Odontol Bras. 2000;14(3):219-24. doi: 10.1590/ S1517-74912000000300006.
18. Thiele MCM, Rosa EAR, Rosa RT. Estomatite protética: estudo dos fatores predisponentes e fatores de virulência da Candida spp. Braz Oral Res. 2005;19:146.
19. Barbachan JJD, Rados PV, Sant'ana Filho M, Domingues, MG. Estudo clínico da estomatite protética: avaliação preliminar. Rev Fac Odontol Porto Alegre. 1995;36(1):27-31.
20. Vasconcelos LCS, Sampaio FC, Sampaio MCC, Pereira MSV, Peixoto MHP. Streptococcus mutans in denture stomatitis patients under antifungal therapy. Rev Odonto Ciênc. 2010;25(2):120-5. doi: 10.1590/S1980-65232010000200003.
21. Silva-Lovato CH, Paranhos HFO, Mello PC, Cruz PC, Freitas KM, Macedo LD. Rising of the instructions degree and of materials and methods of hygiene used by complete dentures users. Rev Odontol UNESP. 2006;35(2):125-31.
22. Nikawa H, Equsa H, Makihira S, Yamashiro H, Fukushima H, Jin C, et al. Alteration of the coadherence of Candida albicans with oral bacteria by dietary sugars. Oral Microbial Immunol. 2001;16(5):279-83. doi: 10.1034/j.1399- 302x.2001.016005279.x.
23. Ribeiro DG, Pavarina AC, Giampaolo ET, Machado AL, Jorge JH, Garcia PP. Effect of oral hygiene education and motivation on removable partial denture wearers: longitudinal study. Gerodontology. 2009;26(2):150-6. doi: doi: 10.1111/j.1741- 2358.2008.00272.x.
 Endereço para correspondência:
Endereço para correspondência:
LC VASCONCELOS
e-mail: laiscv@uol.com.br
Received on: 21/8/2012
Final version resubmitted on: 14/9/2012
Approved on: 28/2/2013













