Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.3 Porto Alegre Jul./Set. 2013
ORIGINAL / ORIGINAL
Dentists' protective measures against occupational and sexual exposure to hepatitis B virus
Perfil de proteção de cirurgiões-dentistas frente à transmissão ocupacional e sexual do vírus da Hepatite B
Clarissa Pessoa FERNANDES I; Francisco Artur Forte OLIVEIRA I; Renata Mota Rodrigues Bitu SOUSA II; Paulo César de ALMEIDA III; Ricardo Gadelha de ABREU IV; José Maria Sampaio MENEZES JÚNIOR V; Márlio Ximenes CARLOS VI; Fabrício Bitu SOUSA I
I Universidade Federal do Ceará, Faculdade de Odontologia, Departamento de Clínica Odontológica. Av. da Universidade, 2853, Benfica, 60020-181, Fortaleza, CE, Brasil
II Universidade Federal do Ceará, Faculdade de Odontologia, Departamento de Saúde Comunitária. Fortaleza, CE, Brasil
III Universidade Federal do Ceará, Centro de Ciências da Saúde. Fortaleza, CE, Brasil
IV Ministério da Saúde, Departamento de Vigilância Epidemiológica. Brasília, DF, Brasil
V Associação Brasileira de Odontologia, Seção Ceará. Fortaleza, CE, Brasil
VI Conselho Regional de Odontologia do Ceará. Fortaleza, CE, Brasil
ABSTRACT
Objective
This study investigated the sexual and occupational exposure of dentists to hepatitis B virus.
Methods
The study used a self-administered, structured, and anonymous questionnaire to collect data from 318 dentists who attended the International Congress of Dentistry held in 2009. The findings were tabulated and associations between variables were determined by the chi-square and Fisher-Freeman-Halton tests.
Results
Most (84.9%) dentists used all the personal protective equipment. Roughly 68.0% had experienced percutaneous injuries but only 36.4% sought specialized care. An unimpressive 75.8% of the sample received the three doses of the hepatitis B vaccine, and a meager 27.0% was tested for hepatitis B surface antibodies (anti-HBs). Only 20.1% of the study dentists used condoms and those with more years of practice were less likely to use them (p=0.006).
Conclusion
The results show that the study sample is at sexual and occupational risk of hepatitis B infection.
Indexing terms: Dentistry. Hepatitis B. Sexuality.Transmission.
RESUMO
Objetivo
Comparar os riscos de transmissão sexual do Vírus da Hepatite B e o perfil de proteção profissional de cirurgiões-dentistas.
Métodos
Questionário auto-aplicável, estruturado e anônimo foi respondido por 318 profissionais participantes de Congresso Internacional de Odontologia, em 2009. Os achados foram agrupados em tabelas, e a associação de variáveis foi feita por meio do teste qui-quadrado e teste de Fisher-Freeman-Halton.
Resultados
Foi observado que 84,9% dos profissionais relataram utilizar todos os Equipamentos de Proteção Individual.Aproximadamente 68,0% já se feriram com instrumento pérfuro-cortante, mas apenas 36,4% procuraram serviço especializado. A prevalência de vacinação completa contra hepatite B foi 75,8%, todavia somente 27,0% realizaram o teste de conversão sorológica(anti-HBs). Quanto ao uso de preservativo, apenas 20,1% afirmaram ter utilizado esse insumo e o tempo de formado foi estatisticamente significante quando associado à menor frequência na utilização (p = 0,006).
Conclusão
Os resultados revelaram possível vulnerabilidade dos dentistas para hepatite B nos âmbitos sexual e profissional.
Termos de indexação: Odontologia. Hepatite B. Sexualidade. Transmissão.
INTRODUCTION
Hepatitis B is an acute or chronic disease caused by hepatitis B virus,which affects liver cells1-2.
Roughly 350 million people around the world are chronic carriers of the virus3-4. In Brazil, the West Amazon region and some micro-regions of the states of Espírito Santo, Paraná, Santa Catarina, and MatoGrosso are considered hyperendemic areas5. In general, the Brazilian South Region is an area of low endemicity and the Central- West, Northeast, and Southeast Regions are areas of intermediate endemicity6.
This serious public health problem have led dentists nowadays to be more concerned with their occupational exposure to hepatitis B virus and the use of personal protective equipment (PPE).
Although occupational exposure is not significant in the general population, hepatitis B virus infection and cross infection in health professionals are significant7. Hepatitis B virus can be transmitted directly through percutaneous and permucosal injuries exposed to infected blood and body fluids8 or indirectly by manually transporting the virus from contaminated counters and work tools to self, since this virus is stable in the environment for more than seven days9-10.Additionally, droplets of blood or secretions are also infectious, so it is possible to acquire the virus by inhaling contaminated aerosols10.
Because of the various routes of transmission of this virus in dental offices, it is understandable that of all infectious diseases, hepatitis B is one of the main causes of death among dentists and interruption of their practice. Moreover, in this context of high vulnerability, the risk of infection by hepatitis B virus increases with the dentist's experience, age, inconsistent use of safety glasses and white coat, and presumed contact with infected blood11-12.
Still in the topic of exposure to hepatitis B virus, another very important route of transmission is sexual intercourse. What is the contribution of these exposures to dentists' routine? Establishing a set of factors that increase the risk to or protection against hepatitis B virus requires analyzing how dentists combine protection strategies in the most important transmission spheres, that is, the professional (occupational exposure) and personal (sexual) spheres.
Sexual intercourse is one of the main routes of transmission of hepatitis B virus in areas of low and intermediate prevalences, such as most of Brazil13. Hepatitis B infection occurs throughout the world and the risk increases with the number of partners, years of sexual activity, history of another sexually transmitted disease (STD), and practice of receptive anal sex14. Nevertheless, data from a study done by the Ministry of Health in 2008 about sexual practices show that only a small portion of the adult population correctly protects itself against STDs, making the population vulnerable to these diseases15.
Given hepatitis B severity, high transmission rate, and low use of protective devices, health departments and education institutions should further incentivize vaccination and the use of condoms, since these are the main ways to prevent hepatitis B infection13,16.
The objective of the present study was to investigate dentists' occupational and sexual exposure to hepatitis B virus.
METHODS
The population of this cross-sectional, quantitative study consisted of 2,427 dentists enrolled in the III International Dentistry Congress held in Fortaleza, Ceará, in May 2009. Sample size (n=318) was determined by the formula for a finite population. The variable "knowledge of the disease" was set at P=50%, since this value results in a maximum sample size. The significance level was set to 5% and the sampling error to 4%. The dentists were selected systematically at the entrance of the forums, symposiums, and lectures.
The data were collected by a self-administered, structured questionnaire with questions about sociodemographic characteristics (gender, race, age, specialty/practice area, and years of practice); attitudes towards occupational risk, including questions about the routine use of PPE, use of additional PPE, occurrence of percutaneous injuries, and visit to a specialized service for treating those injuries; vaccination status with information about vaccination protocol and hepatitis B surface antibody (anti-HBs) testing; and sexual practices, including frequency and use of condoms.
The findings were tabulated and the associations were determined by the chi-square and the Fisher-Freeman- Halton tests. For the inferential analyses, the significance level was set at p≤0.05.
The study was approved by the Research Ethics Committee of the Cearence Academy of Dentistry, under protocol number 93/2009.
RESULTS
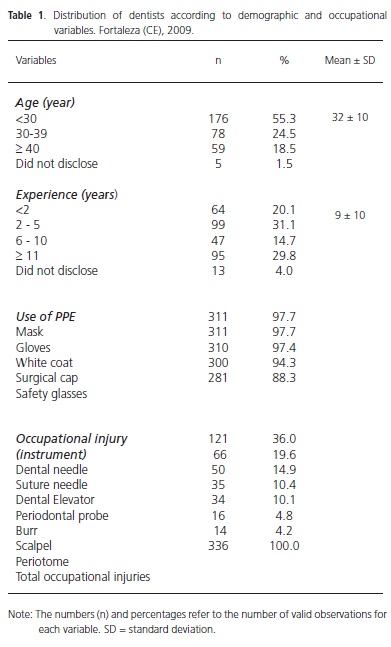
The final sample consisted of 318 dentists, most of them females (61.3%). Dentists aged less than 30 years (55.3%) prevailed and the mean age and standard deviation were 32 ± 10 years; the minimum age was 20 and the maximum, 72 years. Most dentists had two to five years of practice (31.1%) followed by those with more than eleven years of practice (29.8%); the mean experience was 9 ± 10 years, with a minimum experience of nine months and a maximum experience of 48 years. The most common specialty/practice areas were prosthodontics (11.0%), orthodontics (10.1%), general dentistry (8.2%), and endodontics (7.9%). Other demographic and occupational variables are listed in Table 1.
Most dentists (84.9%) reported using all PPE. Of all the PPE, safety glasses were used the least, with 11.7% of the professionals not using them.
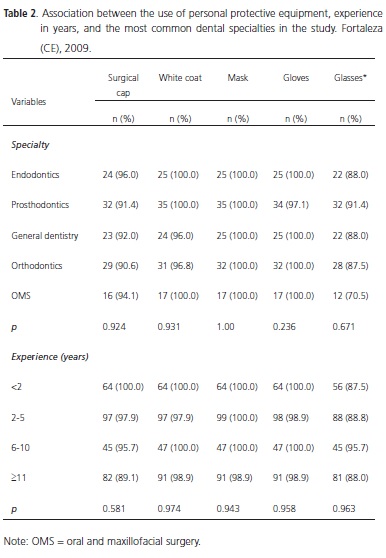
There was no association between the use of PPE and the most common dental specialties in this study (p>0.23), or between the use of PPE and experience (p>0.58) (Table 2).
Most dentists (63.5%) did not use any additional PPE when treating patients with hepatitis B virus but 36.5% did. Of these, 70.0% reported using two pairs of gloves and 18.5% reported using two pairs of gloves and two masks routinely.
The percentage of dentists who had experienced percutaneous injuries was also high (68.2%), but only 36.4% of these sought specialized care. A total of 216 dentists suffered 336 percutaneous injuries, averaging 1.5 injuries per person. The number of occupational accidents totaled 336, averaging 1.5 per injured person.The most recurrent instrument was the needle, responsible for 55.6% of these injuries: 36.0% were caused by dental needles and 19.6% by suture needles.
Approximately 76% of the dentists followed the entire vaccination protocol, that is, they received all three doses, but only 27.0% were tested for anti-HBs, a marker of protective immunity.
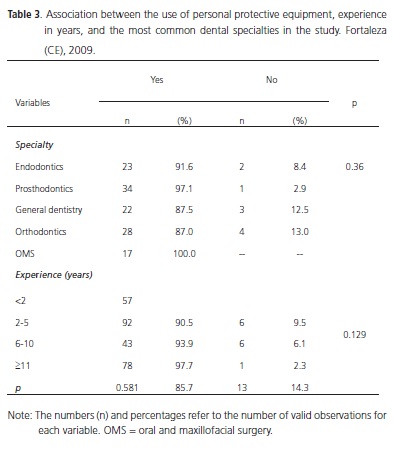
There was no association between vaccination status and specialty (p=0.36) or between vaccination status and experience (p=0.129) (Table 3).
The dentists also disclosed information about their sexual practices: 76.7% reported having intercourse frequently and 86.5% reported sexual monogamy.
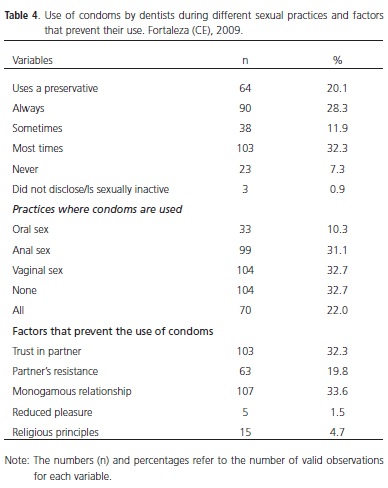
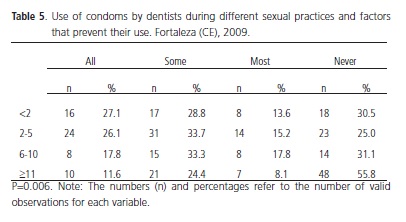
Table 4 shows the frequency with which dentists use condoms in various sexual practices and the factors that inhibit their use.
Many dentists (66.4%) reported that the risk of sexual hepatitis B transmission is high. However, only 20.1% used condoms all the time, 32.7% never used condoms in any sexual practice, 60.3% had never used condoms or used only a few times, and 72.3% admitted that it is important to use condoms all the time. When asked about condom avoidance, 33.6% reported not using condoms because they were in a monogamous relationship and 32.3% because they trusted their partner.
In the present study, professional experience was significantly associated with condom avoidance (p=0.006) (Table 5). Approximately 80.0% of the dentists with 11 or more years of practice used condoms sometimes or never during intercourse and only 11.6% used them all the time.
DISCUSSION
The percentage of dentists who use all PPE (84.9%) was lower than that reported in the literature. Garcia & Blank17 found that 91.0% of their sample always used gloves and 59.5% always used safety glasses. In the present study, 88.3% of the sample used safety glasses.
Retrospective data collected by a self-administered questionnaire may cause underestimations because study participants tend to report acceptable behaviors even when they do not practice them. This is known as the Hawthorne effect, a term coined by Henry A. Landsberger.
Some dentists (36.4%) also used additional PPE, showing that these individuals have little knowledge about biosafety, a probable fear of being infected during their work, and lack of confidence in the use of sharp instruments.The Centers for Disease Control and Prevention do not recommend the use of two pairs of gloves during the procedures, since the effectiveness of this practice has not been demonstrated. The Canadian Dental Association states that this practice should be related to the procedure, not to the patient, and it may affect hand dexterity and touch18.
Universal biosafety guidelines should be followed with all patients.Dentists may be using PPE incorrectly when they treat people with unknown infections, increasing their risk of exposure18.
The poor organization of work procedures with a focus on biosafety is evidenced by the fact that most individuals of the present study have experienced percutaneous injuries and few sought treatment in a specialized service. The low percentage of individuals who seek specialized care may be a reflection of the study population's disregard for diseases transmitted by percutaneous injuries.
Records of these injuries are essential for professionals to take protective measures and for authorities to consider dentistry a hazardous profession. There is an urgent need to implement procedures that record, notify, and investigate injuries and hazardous situations19 and to provide refresher lectures about biosafety and the risk of occupational exposure to infectious diseases in dental practice.
The finding that the needle is responsible for most occupational injuries (55.6%) is confirmed by the literature. Shah et al.20 reported that needles were responsible for 89% of the dental practice injuries in seven years of notification. Currently, the Centers for Disease Control and Prevention recommend safer work practices to avoid risk21. Increased awareness and continuing education may significantly prevent percutaneous injuries by implementing organized biosafety workflows.
According to the present findings, prevention of infectious diseases at work basically comes down to the use of PPE. Although the percentage of individuals who received all three doses of the hepatitis B vaccine (76.0%) exceeds22-24 or confirms10,25 the percentages reported in the literature, it is still unsatisfactory, especially because these vaccines for health professionals are providedby the Unified Health Care System. Ideally, dentists should start receiving the vaccines while in college, before engaging in clinical practice11-12, because unvaccinated dentists are five times more likely to acquire the hepatitis B virus if exposed, and 30% to 40% of these individuals will become seropositive7.
The percentage of study dentists who underwent the anti-HBs test (27.0%), a little studied issue, exceeded that reported by Batista et al.25 (5.7%) and fell far behind that reported by Petti et al.26 (53.8%). Therefore, the percentage found by the present study is far from ideal and indicates the need of advertising the test, which should be done one or two months after the third dose of the vaccine as recommended by the Centers for Disease Control and Prevention27, since some population groups respond poorly to the vaccine. Male gender, obesity, smoking, kidney failure, chronic liver disease, and immune deficiency contribute to low immunity28-29. Furthermore, it is important for dentists to know their anti-HBs status so that they may contribute to the post-percutaneous injury conduct.
In the present study, specialty was not statistically associated with vaccination status (p=0.36) even though many studies have found such association. MacCarthy& MacDonald30 found that orthodontists get vaccinated the least and are the least likely to have their staff vaccinated. This is important because their staff members frequently work with sharp instruments, so are at considerable risk of percutaneous injuries.
Despite the absence of association between years of practice and vaccination status (p=0.129), dentists with 11 years of practice or more tend to get vaccines less frequently, corroborating the findings published by Batista et al.25 and Martins & Barreto10 who found that the percentage of vaccinated dentists with more years of practice was significantly lower, showing the lack of refresher courses and vaccination campaigns for this population.
Although occupational exposure is an important route of transmission, we cannot forget that hepatitis B can also be transmitted sexually and this is the main route of transmission in most of Brazil13. The study participants know that hepatitis B virus can be sexually transmitted, but they do not use condoms often, especially those with 11 years or more of professional practice. Although 76.0% of these dentists have a 90% to 95% chance of being immune to hepatitis B, they may still acquire other STDs from their sexual partners, such as HIV/AIDS. This fact is supported by a study done by the Ministry of Health in 2008 that found that 21.5% of sexually active individuals had used condoms in all sexual intercourses they had had in the 12 months that preceded the study15.
Among the reasons for not using condoms, a monogamous relationship and trust in the partner, which are the most common reasons given by the general population, are not officially considered protective against STDs given that the above mentioned study also found that 21% of the men and 11% of the women who live with a partner had casual sex, and 63% of these individuals did not always use condoms15.
This scenario begs for actions that promote vaccination against hepatitis B, including agreements with universities. Dentistry courses also need to better discuss sexuality and safe sex, especially the prevention of STDs. Finally, actions that promote safe sexual practices are needed, especially for more experienced dentists.
CONCLUSION
The study results show that the present sample may be clinically vulnerable to hepatitis B infection since twothirds had already experienced percutaneous injuries and of these, only 36% sought specialized care. Furthermore, the vaccination rate against hepatitis B was low:fewer than 80% of the participants were vaccinated and only 27% knew their immunity status. Given that the main route of transmission of hepatitis B virus is sexual, that only onefifth of the participants always used condoms, and that higher age was directly associated with lower condom use, the study participants are at high risk of acquiring the disease outside of their offices.
Collaborators
CP FERNANDES and FAF OLIVEIRA helped to conceive and plan the study, collect and interpret data, and write and review the article. RMRB SOUSA helped to conceive the study, interpret data, and write and review the article. PC ALMEIDA helped to conceive the study, interpret data, analyze the data statistically, and write and review the article. RG ABREU, JMS MENEZES JUNIOR, and MX CARLOS helped to write and review the article. FB SOUSA helped to conceive and plan the study, and write and review the article.
REFERENCES
1. Zanetti AR, van Damme P, Shouval D. The global impact of vaccination against hepatitis B: A historical overview. Vaccine. 2008;26(49):6266-73. doi: 10.1016/j.vaccine.2008.09.056. [ Links ]
2. Gillcrist JA. Hepatitis viruses A, B, C, D, E and G: implications for dental personnel. J Am Dent Assoc. 1999;130(4):509-20.
3. Goldstein ST, Zhou F, Hadler SC, Bell BP, Mast EE, Margolis HS. A mathematical model to estimate global hepatitis B disease burden and vaccination impact. Int J Epidemiol. 2005;34(6):1329-39. doi: 10.1093/ije/dyi206.
4. Kao JH, Chen DS. Global control of hepatitis B virus infection. Lancet Infect Dis. 2002;2(7):395-403.
5. Figueiredo GM. Breve histórico da emergência da hepatite B como problema de saúde pública. J Bras AIDS. 2007;8(1):8-13.
6. Chávez HJ, Campana SG, Haas P. Panorama da hepatite B no Brasil e no Estado de Santa Catarina. Rev Panam Salud Publica. 2003;14(2):91-6. doi: 10.1590/S1020-49892003000700003.
7. Gir E, Netto JC, Malaguti SE, Canini SR, Hayashida M, Machado AA. Accidents with biological material and immunization against hepatitis B among students from the health area. Rev Latino-Am Enfermagem. 2008;16(3):401-6. doi: 10.1590/ S0104-11692008000300011.
8. Franco E, Bagnato B, Marino MG, Meleleo C, Serino L, Zaratti L. Hepatitis B: epidemiology and prevention in developing countries. World J Hepatol. 2012;4(3):74-80. doi: 10.4254/wjh. v4.i3.74.
9. Alter MJ. Epidemiology of hepatitis B in Europe and worldwide. J Hepatol. 2003;39:S64-S69.
10. Martins AMEBL, Barreto SM. Vacinação contra hepatite B entre cirurgiões-dentistas. Rev Saúde Pública. 2003;37(3):333-8. doi: 10.1590/S0034-89102003000300011.
11. Cavalcanti FM, Melo RGSV, Patrício DPS, Zimmermann RD. Hepatite B: conhecimento e vacinação entre os acadêmicos da Faculdade de Odontologia de Caruaru - PE. Odontol Clín-Cient. 2009;8(1):59-65.
12. Mahboobi N, Agha-Hosseini F, Mahboobi N, Safari S, Lavanchy D, Alavian SM. Hepatitis B virus infection in dentistry: a forgotten topic. J Viral Hepat. 2010;17(5):307-16. doi: doi: 10.1111/j.1365-2893.2010.01284.x.
13. Mauss S, Berg T, Rockstroh J, Sarrazin C, Wedemeyer H. Hepatology: a clinical textbook [text internet]. Baltimore: Flying Publisher; 2009 [citado 2009 Dez 10]. Disponível em: <http:// www.hepatologytextbook.com>.
14. de Franchis R, Hadengue A, Lau G, Lavanchy D, Lok A, McIntyre N, et al. EASL Jury. EASL International Consensus Conference on Hepatitis B. 13-14 September, 2002 Geneva, Switzerland. Consensus statement (long version). J Hepatol. 2003;39(Suppl 1):S3-S25.
15. Brasil. Ministério da Saúde. Pesquisa de conhecimentos, atitudes e práticas da população brasileira de 15 a 64 anos de idade. Brasília: Ministério da Saúde; 2008 [citado 2009 Dez 9]. Disponível em: < http://www.aids.gov.br/sites/default/files/ anexos/publicacao/2009/40352/pcap_2008_f_pdf_13227.pdf>.
16. Bernabe-Ortiz A, Carcamo CP, Scott JD, Hughes JP, Garcia PJ, Holmes KK. HBV infection in relation to consistent condom use: A population-based study in peru. PLoSOne. 2011;6(9):e24721.
17. Garcia LP, Blank VLG. Prevalência de exposições ocupacionais de cirurgiões-dentistas e auxiliares de consultório dentário a material biológico. Cad Saúde Pública. 2006;22(1):97-108. doi: 10.1590/S0102-311X2006000100011
18. Lux J. Infection control practice guidelines in dental hygiene: part 1. Can J Dent Hygiene. 2008;42(2):63-103.
19. Rapparini C, Reinhardt EL. Manual de implementação: programa de prevenção de acidentes com materiais perfurocortantes em serviços de saúde. São Paulo: Fundacentro; 2010.
20. Shah SM, Merchant AT, Dosman JA. Percutaneous injuries among dental professionals in Washington State. BMC Public Health. 2006;6:269.
21. Centers for Disease Control and Prevention. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for Postexposure Prophylaxis. MMWR. 2001;50(RR-11): 1-52.
22. Rimkuviene J, Puriene A, Peciuliene V, Zaleckas L. Percutaneous injuries and hepatitis B vaccination among Lithuanian dentists. Stomatologija. 2011;13(1):2-7.
23. Di Giuseppe G, Nobile CG, Marinelli P, Angelillo IF. A survey of knowledge, attitudes, and behavior of italian dentists toward immunization. Vaccine. 2007;25(9):1669-75. doi: /10.1016/j. vaccine.2006.10.056.
24. Ottoni CMC, Penna FJ, Oliveira CG, Souza C. Prevalência de marcadores sorológicos de hepatite B em estudantes de odontologia e dentistas em Belo Horizonte, Brasil. Bol Oficina Sanit Panam. 1995;118(2):108-14.
25. Batista SMF, Andreasi MSA, Borges AMT, Lindenberg ASC, Silva AL, Fernandes TD, et al. Seropositivity for hepatitis V virus, vaccination coverage, and vaccine response in dentists from Campo Grande, Mato Grosso do Sul, Brazil. Mem Inst Oswaldo Cruz. 2006;101(3):263-7. doi: 10.1590/S0074- 02762006000300006.
26. Petti S, Messano GA, Polimeni A. Dentists' awareness toward vaccine preventable diseases. Vaccine. 2011;29(45):8108-12. doi: 10.1016/j.vaccine.2011.08.034
27. Centers for Disease Control and Prevention. Immunization of Health-Care Personnel. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR. 2011;60(RR-07):1-45.
28. Chen DS. Hepatitis B vaccination: The key towards elimination and eradication of hepatitis B. J Hepatol. 2009;50(4):805-16. doi: 10.1016/j.jhep.2009.01.002.
29 Ferreira CT, da Silveira TR. Hepatites virais: aspectos da epidemiologia e da prevenção. RevBrasEpidemiol. 2004;7(4):473- 87. doi: 10.1590/S1415-790X2004000400010.
30. Macarthy GM, Macdonald JK. A comparison of infection control practices of different groups of oral specialists and general dental practitioners. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 1998;85(1):47-54. doi: 10.1016/S1079-2104(98)90397-3.
 Endereço para correspondência:
Endereço para correspondência:
FB SOUSA
e-mail: fbitu@hotmail.com
Received on: 21/10/2011
Final version resubmitted on: 5/6/2012
Approved on: 3/9/2012













