Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.3 Porto Alegre Jul./Set. 2013
ORIGINAL / ORIGINAL
Facial edema reduction after alveolar bone grafting surgery in cleft lip and palate patients: a new lymphatic drainage protocol
Redução do edema facial após cirurgia de enxerto ósseo alveolar em pacientes com fissura labiopalatina: um novo protocolo de drenagem linfática
Tatiane Romanini Rodrigues FERREIRAI; Marcia Zavaski SABATELLA (in memoriam)I; Thaisa Maria Santos SILVAI; Ivy Kiemle TRINDADE-SUEDAMII; José Roberto Pereira LAURISIII; Alceu Sergio TRINDADE JUNIORII
I Universidade Estácio de Sá, Faculdade de Odontologia, Departamento de Endodontia. Av. Alfredo Baltazar da Silveira, 580, Recreio, 22790-710, Rio de Janeiro, RJ, Brasil.
II Universidade de São Paulo, Hospital de Reabilitação de Anomalias Craniofaciais (Laboratório de Fisiologia), Faculdade de Odontologia, Departamento de Ciências Biológicas. Al. Octávio Pinheiro Brisola, 9-75, 17012-901, Bauru, SP, Brasil.
III Universidade de São Paulo, Faculdade de Odontologia, Departamento de Saúde Coletiva. Bauru, SP, Brasil.
ABSTRACT
Objective
To determine the effectiveness of standardized manual lymphatic drainage in reducing facial edema, interincisal distance and pain after alveolar bone grafting surgery in patients with cleft lip and palate.
Methods
In this randomized open controlled parallel trial, 51 patients with cleft lip and palate submitted to after alveolar bone grafting were randomly divided into two groups: 1) routine group (n=22): manual lymphatic drainage performed by the patient, pumping and sliding maneuvers, for 10 minutes, 3 times/day, on the operated hemiface, and, 2) drainage group (n=29): manual lymphatic drainage performed by the physical therapist, pumping, sliding and stationary cycles maneuvers, for 30 minutes, on both sides of the face. Interincisal distance and lines formed between the nasal ala and tragus (L1) and between the nasal ala and inferior region of the ear (L2) were assessed on the operated hemiface, preoperatively, two (PO2) and four days postoperatively (PO4). Pain analog scale was applied on PO1, PO2, PO3 and PO4.
Results
A significant reduction in facial edema from PO2 to PO4 was observed in drainage group (L1:11.50 to 11.38cm; L2:11.06 to 10.85cm) compared to routine group; interincisal distance increased significantly in both groups from PO2 to PO4 (routine group: 1.91 to 3.14cm; drainage group: 1.99 to 3.17cm, respectively). Drainage group patients reported absence of pain on PO3 while routine group patients only on PO4.
Conclusion
The proposed manual lymphatic drainage procedure provided significant reduction in facial edema reduction, in pain, and interincisal distance increase, reinforcing the hypothesis that this technique was effective in accelerating the recovery of patients with cleft lip and palate undergoing alveolar bone grafting surgery. Brazilian Register of Clinical Trials: RBR-4z7cnh.
Indexing terms: Bone transplantation. Cleft palate. Edema. Face. Lymphatic system. Massage.
RESUMO
Objetivo
Determinar a eficácia da drenagem linfática manual na redução do edema facial, da distância interincisal e da dor após cirurgia de enxerto ósseo alveolar em pacientes com fissura labiopalatina.
Métodos
Estudo paralelo controlado randomizado aberto de 51 indivíduos com fissura labiopalatina, submetidos ao enxerto ósseo alveolar, divididos aleatoriamente em 2 grupos: 1) grupo rotina (n=22), realizada pelo paciente, utilizando manobras de bombeamento e deslizamento, por 10 minutos, 3 vezes/dia, na hemiface operada, e, 2) grupo drenagem padronizada (n=29), realizada pelo fisioterapeuta, utilizando manobras de bombeamento, deslizamento e círculos estacionários, por 30 minutos, nos dois lados da face. Distância interincisal e as linhas formadas pela união de pontos localizados na asa nasal e tragus (L1) e asa nasal e região inferior do ouvido (L2) foram aferidas na hemiface operada no préoperatório, nos pós-operatórios de dois (PO2) e quatro dias (PO4). Aplicou-se Escala Analógica de Dor nos PO1, PO2, PO3 e PO4.
Resultados
Observou-se redução significativa do edema no grupo drenagem padronizada entre PO2 e PO4 (L1: 11,50 para 11,38cm; L2: 11,06 para 10,85cm) e aumento significativo na distância interincisal nos 2 grupos entre PO2 e PO4 (RG: 1,91 para 3,14cm; drenagem padronizada: 1,99 para 3,17cm, respectivamente). Ausência de dor foi relatada pelo grupo drenagem padronizada no PO3 e pelo grupo rotina no PO4.
Conclusão
A drenagem linfática manual proposta reduziu significantemente o edema facial, a dor e aumentou a distância interincisal quando comparado ao grupo rotina, reforçando a hipótese que a técnica proposta acelerou a recuperação de pacientes com fissura labiopalatina submetidos à cirurgia de enxerto ósseo alveolar. Registro Brasileiro de Ensaios Clínicos: RBR-4z7cnh.
Termos de indexação: Transplante ósseo. Edema. Face. Sistema linfático. Massagem. Fissura palatina.
INTRODUCTION
Cleft lip and palate is the most prevalent malformation in the maxillofacial region. Epidemiological data shows that 1:650 children are born with cleft lip and palate1. A cleft lip can result from a fail in fusion of the lateral and medial nasal processes with the anterior extension of maxillary processes on either side and the development of a cleft palate can occur from a failure of palatal ridges to contact because of a growth deficiency or disturbance in the ridge elevation mechanism, from a failure of the ridges to merge after contact has been established, because an unexpected rupture after the palatine ridges merge, or even because of defective consolidation of mesenchymal palatine ridges2.
Cleft lip and palate individuals require specific surgical procedures such as lip (cheiloplasty) and palate closure (palatoplasty), performed 3 to 12 months after birth, respectively. The remaining bone maxillary defect can be reconstructed by alveolar bone grafting, which reconstructs the maxillary cleft by filling it with autogenous cancellous bone harvested from the iliac crest. Its main goal is to provide bone tissue for the cleft site and, consequently, unite the maxillary segments3, allowing further development of normal occlusion. In 1994, the Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo (HRAC-USP) included secondary bone graft surgery in the treatment protocol of clefts affecting the alveolar process3, however, the postoperative period involves discomfort, pain, facial edema and limitation of oral movements.
It is known that, in the presence of mechanical traumas such as surgical procedures, there may be structural or functional alteration of the lymphatic vessels, caused by laceration or compression. This mechanical obstruction substantially alters the balance of stresses, thereby causing edema. Manual lymphatic drainage (MLD) procedures may accelerate the patient recovery in the postoperative period and contribute to reduce the inflammatory signs on the face. The goal of this treatment is to drain the excess fluid accumulated in the interstitial spaces, maintaining the balance of tissue and hydrostatic pressures4-5.
Initially published by Vodder in 1936, manual lymphatic drainage is performed with tender, slow, rhythmic and superficial procedures to mobilize the liquid inside the superficial lymphatic vessels. The hand pressure applied on the body should be light, around 30 to 40 mmHg, in order to avoid lymphatic collapse4,6.
Nowadays, manual lymphatic drainage has been applied for many treatment modalities. Bose & Aggithaya7, used manual lymphatic drainage for treating limb edema caused by lymphatic filariasis and, as a result, swelling and inflammatory episodes were diminished7. In patients with heart failure and lower limb lymphedema, the manual lymphatic drainage treatment decreased the edema as expected, and the heart rate also decreased following manual lymphatic drainage, in contrast with all other hemodynamic parameters which were not affected by manual lymphatic drainage. In cases of lymphedema after cancer treatment, Korpan et al.8 mention that further randomized trials are required to determine which component or combination of components in complex decongestive therapy works most effectively9. In addition to the physical benefit, the therapy provides a pleasant experience related to welfare and relaxation8.
Few studies have investigated manual lymphatic drainage applied in facial surgeries. Some authors report its application for the edema after treatment of head and neck cancer10-13, tooth extraction14 and plastic surgeries15. However, there are no data in the literature on the application of manual lymphatic drainage in patients with cleft lip and palate submitted to alveolar bone grafting.
The Physical Therapy Sector of the Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo acts in the postoperative period of alveolar bone grafting surgery, and manual lymphatic drainage is among the procedures performed. The routine protocol for alveolar bone grafting recovery consists of manual lymphatic drainage performed by the patient or caretaker, first explained by the physical therapist. Thus, we assume that the effectiveness of manual lymphatic drainage and its benefits may be reduced. This study proposed a different approach for application of manual lymphatic drainage procedures than the one currently performed at the Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo, as well as to elucidate if this new procedure would effectively contribute to reduce the postoperative edema after alveolar bone grafting.
Therefore, this study aimed at determining the effectiveness of a new standardized manual lymphatic drainage procedure to reduce facial edema, interincisal distance and pain of patients with cleft lip and palate submitted to alveolar bone grafting surgery.
METHODS
The study was carried out at the Physical Therapy Sector, Laboratory of Physiology and Inpatient Sector of the Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo and was conducted on 51 patients with unilateral cleft lip and palate, aged 10 to 15 years, of both genders, submitted to alveolar bone grafting. Surgery and manual lymphatic drainage procedures were performed with no cost to the patient.
The present research was revised and approved by the Institutional Ethics Committee of the Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo (process n. 361/2008- SVAPEPE-CEP), RBR- 4z7cnh REBEC (Brazilian Register of Clinical Trials), and followed Helsinki Declaration. All patients provided written informed consent before surgery and manual lymphatic drainage procedure were undertaken.
The initial study population comprised 60 patients with cleft lip and palate and with indication for alveolar bone grafing surgery. Patients were randomly selected before surgery into drainage routine group (RG) or standardized manual lymphatic drainage group (DG). Manual lymphatic drainage procedures were performed from the second to the fourth postoperative day. At the end of the study, a total of 51 patients comprised the sample size. Nine patients were excluded from the study either because they were discharged from the dental team before the fourth postoperative day or because they received medications that did not comprise the routine protocol used at Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo.
In routine group, 22 patients (7 females and 15 males) were submitted to the procedures routinely performed at Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo, in which the professionals taught and explained manual lymphatic drainage procedures that were then performed by the patients themselves or by their caretakers. Manual lymphatic drainage procedures were characterized by pumping on the submandibular lymph nodes and superficial sliding only on the operated hemiface, for 10 minutes, 3 times a day, as well as facial mimics exercises (lip protraction, lateral traction of the angle of the mouth, smiling, and strongly opening and closing the eyes).
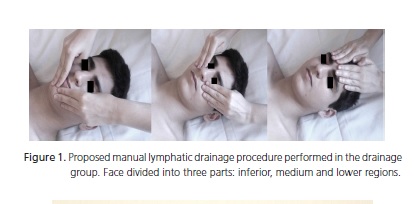
In drainage group, 29 patients (17 females and 12 males) were submitted to the proposed manual lymphatic drainage procedures using specific and standardized manual lymphatic drainage techniques, always performed by the physical therapist once a day, for 30 minutes, in a calm and comfortable environment, with the patient lying on a bed with the headboard raised at 25 degrees. Pumping, superficial sliding and stationary circles were performed on the face, applying light pressure with the hands according to the Vodder technique, always toward the adjacent lymph nodes, in a slow and constant rhythm4,17-20. Manual lymphatic drainage procedures were characterized by pumping maneuvers on the supraclavicular, cervical, retroauricular and submandibular lymph nodes, submental lymph nodes in the neck, and preauricular, submandibular and submental lymph nodes after sliding movements on the entire face. The face was divided into three parts: lower, medium and upper regions4,17,20 (Figure 1).
After manual lymphatic drainage, patients performed facial mimics exercises, six times each (opening and closing the eyes, contraction of nose and nasal ala muscles, protraction of closed lips, protraction and lateral movement of the lips, and distention of open lips)15. Considering that in routine group drainage was carried out exclusively by the patient and in drainage group drainage was performed by the therapist, it was not possible to blind them.
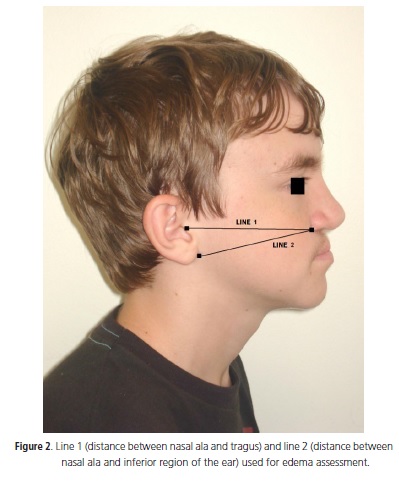
In both groups, facial edema and interincisal distance were measured preoperatively (PRE) and two (PO2) and four days postoperatively (PO4). For the assessment of facial dimensions (Figure 2), three points were marked on the face using a surgical marker and then two lines were formed and measured, in centimeters, using a conventional tape measure. These lines corresponded to the distance between nasal ala and tragus (line 1), and distance between nasal ala and inferior region of the ear (line 2). Measurements were assessed on the operated hemiface, three times on each evaluation period, and the mean value was considered for the analysis. The maximum active interincisal distance was evaluated with a manual pachymeter on the quadrant that presented the best dental arch alignment, to measure how much the swelling interfered with the movement. Interincisal distance was obtained three times and the mean value was considered for the analysis. For pain assessment, patients were asked to score their pain on PO1, PO2, PO3 and PO4 using a visual analog pain scale, a ten point scale where 0 corresponded to absence of pain and 10 corresponded to an agonizing pain.
In drainage group, patients were asked about the feelings experienced with the proposed therapy, such as reduction of pain, sensation of relaxation and sleep, during therapy and on PO2, PO3 and PO4. Questions were delivered for the patient's own answer and corresponded to: 1) Was your pain reduced after therapy? 1a) If positive, please score the improvement as 0-10 2) How much pain are you feeling now? 3) Did you feel better and more relaxed after therapy? 3a) If positive, please score the relaxation as 0-10. 4) Did you sleep during therapy? Questions were not applied to routine group because manual lymphatic drainage was performed at times defined by the patients, with different characteristics compared to the method used in the drainage group.
Patients from both groups were submitted to the same pharmacological treatment with cefazolin and ibuprofen during and after surgery, in accordance with the protocols of Hospital for Rehabilitation of Craniofacial Anomalies of University of São Paulo.
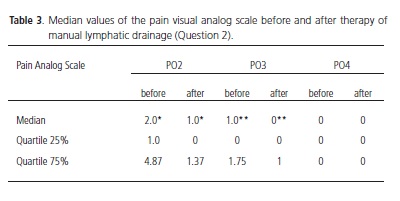
Regarding the mean values of lines 1 and 2 and interincisal distance, a confidence limit of 95% was considered for statistical analysis. Values at the preoperative period, PO2 and PO4 were compared by analysis of variance for repeated measures and by the Tukey test. Comparison between groups was done by Student´s t test. Pain visual analog scale values were tabulated and the medians and quartiles were obtained. Comparison between groups was performed by the non-parametric Mann-Whitney test. Questions about the therapy were analyzed by calculation of the relative frequency of answers. For analysis of question 2, data from pain visual analog scale before and after manual lymphatic drainage were evaluated by the non-parametric Wilcoxon test. A significance level of p<0.05 was considered for all tests.
RESULTS
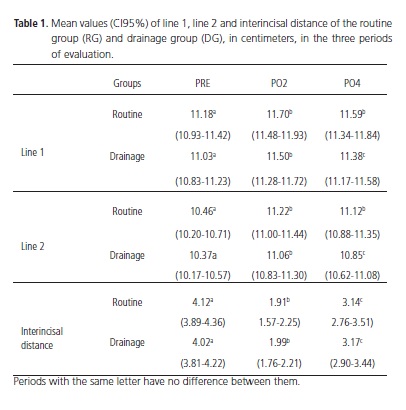
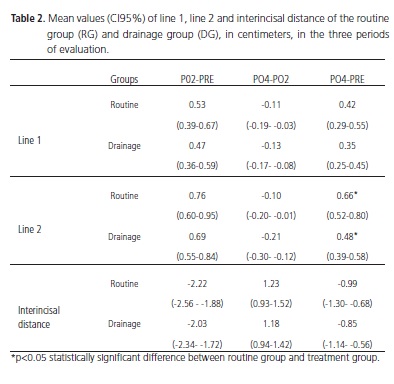
Data collection and patient treatments were conducted between January and September 2009. The study was completed when the sample enabled the statistical analysis. Mean values of facial dimensions (Table 1) regarding lines 1 and 2 and the comparison between periods (Table 2) demonstrated a reduction in facial edema between PRE and PO2, and PRE and PO4 in routine group.
In drainage group, significant reduction was observed from PRE to PO2, PRE to PO4 and also from PO2 to PO4. Overall, a significant reduction in facial edema was observed in drainage group compared to routine group. Evaluation of the interincisal distance revealed an increase in this measurement between PRE and PO2, PRE and PO4 and PO2 and PO4 in both groups.
Regarding pain analog scale, mean values from routine group were 3.0 on PO1, 4.0 on PO2, 2.0 on PO3 and 0 on PO4. Drainage group values were 3.0 on PO1, 2.0 on PO2; 0 on PO3 and PO4. Significant difference between routine group and routine group were observed on PO2 and PO3 (Figure 2).
According to the questions applied to drainage group about pain relief, when patients were asked if the pain had been reduced after the proposed therapy (Question 1), all patients (100%) responded positively on the three days evaluated. The mean improvement of pain scores after therapy (Question 1a) was 8.65±1.94 on PO2, 8.96±2.06 on PO3 and 9.4±2.01 on PO4. Score 10, which corresponded to the maximum improvement of pain, was reported by 39.13% of patients on PO2, 52.17% on PO3 and 80% on PO4. Patients reporting score 9, nearly maximum, were 30.43% on PO2, 34.78% on PO3 and 15% on PO4. Question 2 evaluated how much pain patients were still feeling immediately after manual lymphatic drainage. The values revealed statistical difference in pain analog scale before and after manual lymphatic drainage on PO2 and PO3 (Table 3).
On PO2, 82.61% of patients complained of pain before therapy, and this value was reduced to 56.53% after manual lymphatic drainage. The same was observed on PO3, when 52.18% reported pain before and only 30.44% after therapy. On PO4, 15% reported pain before and only 10% complained of pain after therapy. On the third question, all patients reported feeling more relaxed after manual lymphatic drainage in the three study periods. Concerning the score assigned to the relaxation (Question 3a), the mean values were 8.70±1.64 on PO2, 9.41±1.01 on PO3 and 9.15±1.59 on the PO4. The maximum relaxation during therapy (score 10) was reported by 43.47% of patients on PO2; 65.21% on PO3; and 60% on PO4. A total of 26.08% on PO2; 17.39% on PO3; and 25% on PO4 assigned score 9, i.e., nearly maximum. Finally, question 4 evaluated the effect of manual lymphatic drainage to facilitate sleep induction during therapy. On PO2, 43.47% of the patients slept during therapy, 47.82% "nearly slept" and 8.69% did not sleep. On PO3, 56.52% slept, 34.78% "nearly slept" and 8.69% did not sleep. On PO4, 55% slept, 40% "nearly slept" and 5% did not sleep.
DISCUSSION
Differences observed in the values of lines 1 and 2, between the second and fourth days postoperatively, demonstrated that the therapy proposed in the drainage group was effective in reducing facial dimensions in the postoperative period. Concerning the measurements in the routine group, there was no difference between PO2 and PO4, indicating that patients in this group did not present a significant reduction in facial edema during hospitalization (Table 1). Comparison between groups showed that the proposed treatment was effective in reducing facial edema compared to the routine treatment. This data was evidenced by the mean values observed when comparing PO4 with PRE, in line 2 (Table 2).
No studies have addressed the application of manual lymphatic drainage in the postoperative period of alveolar bone grafting in patients with cleft lip and palate, yet some authors have demonstrated the effectiveness of lymphatic drainage after surgery for head and neck cancer, with reduction in facial dimensions10-12,13. In these studies, a significant reduction in facial edema was reported, assessed by facial measurements or by ultrasound, after manual lymphatic drainage sessions11. After bilateral extraction of third molars, researchers have observed a reduction of edema on the hemiface submitted to manual lymphatic drainage compared to the contralateral side, assessed by facial measurements14. As in the present study, most investigations use a tape measure to evaluate the edema10-11,13-14, because of its easy application and low cost. These authors used the mandibular angle as one facial point; however, edema at this site on the postoperative period of alveolar bone grafting does not allow the repetition of measurements when this point is taken as parameter. With regard to active exercises, the literature demonstrates that muscular contraction aids the lymph flow, thus exercises should be part of programs for rehabilitation and edema reduction. However, the aforementioned papers regarding the application of manual lymphatic drainage on the face do not report the utilization of facial mimic exercises.
Considering mouth opening, both groups presented similar results in the analysis of maximum active interincisal distance. Data revealed that the values observed on PO4 did not return to the mean value of the preoperative period; however, after the onset of manual lymphatic drainage on PO2, there was an increase in this measurement in both groups. This finding further evidences the effectiveness of manual lymphatic drainage on the recovery of individuals with cleft lip and palate. Godoy et al.21 reported an evident enhancement in mouth opening in patient presenting edema and fibrosis after laryngectomy. These authors reported, in another study, reduction in facial and tongue edema and improvement of pain and overall discomfort after application of cervical stimulation22.
Data from visual analog scale demonstrated that pain was reduced in both groups after the onset of manual lymphatic drainage, although patients from drainage group reported absence of pain on PO3 while routine group patients only on PO4. This result suggests that the proposed manual lymphatic drainage provided a more effective pain reduction. Szolnoky et al.14 reported pain reduction assessed by pain visual analog scale after the onset of manual lymphatic drainage, evidencing the significant improvement in the quality of life, and regular photographs of the patients were used to evaluate the effectiveness of manual lymphatic drainage, demonstrating an important improvement in the quality of life12.
In the present study, the four questions applied to the patients in the drainage group evidenced that, in addition to the reduction of facial edema demonstrated by the measurements, the suggested manual lymphatic drainage reduced the pain, induced relaxation, and facilitated sleep induction. In Question 1, the mean scores of pain reduction after therapy increased at each day of treatment. Question 2 revealed that the percentage of patients complaining of pain before therapy was reduced after the attendance, so that on PO4 only 10% complained of pain after manual lymphatic drainage. Differences between values before and after manual lymphatic drainage therapy on PO2 and PO3 once again demonstrate the reduction of pain in drainage group. Question 3 revealed that the reduction of pain is the most important factor influencing patient relaxation, and the success of the suggested therapy is confirmed by the scores assigned for relaxation by the patients.
Woods reported that daily application of manual lymphatic drainage induced a sensation of quietude and relaxation for the patients and physical changes in edema9 while Piso et al.10 showed that edema remission promoted a considerable reduction in the tension on the face and enhanced speech and swallowing. The emotional impact caused by facial edema may psychologically influence the self-esteem and treatment compliance, impairing the recovery. Cobo et al.11 stated that facial edema triggered an important negative emotional reaction on the patients. Question 4 evidenced the success of the suggested therapy, because the reduction in pain and increased relaxation induced the patient to sleep. Moreover, these data confirm the perfect interaction between patient and professional, once patients are only induced to sleep when they feel safe, comfortable and reliant on the treatment and professional.
Williams et al.23 demonstrated that the therapy enhanced the emotional status, reducing the concern, irritability, stress and depression, improving the dyspnea and sleep disorders. According to Bernas et al.24, patients are frequently induced to sleep by the tender rhythm of manual lymphatic drainage techniques. In other study, effectiveness of manual lymphatic drainage was assessed in palliative care patients with lymphoedema in advanced stages of cancer. It was observed that manual lymphatic drainage was well tolerated in 92% patients and 94% patients showed a clinically relevant improvement in pain25.
The proposed manual lymphatic drainage technique aimed at stimulating a large number of lymph nodes on the face and neck to allow a faster lymph flow26. Warszowski27 concluded that visualization of drainage routes in unexpected regions allows the effectiveness of techniques to stimulate useful accessory ways for resorption of the lymphedema27.
In other study, authors demonstrated that nearinfrared fluorescence imaging provides a mapping of functional lymph vessels for direction of efficient manual lymphatic drainage therapy in the head and neck area28.
Accomplishment of the proposed procedures in drainage group on both hemifaces, by a single professional, using techniques that intensify the lymph drainage, may be the most probable explanation for edema reduction accelerating patient recovery. Additional studies addressing reports of subjective sensations as reduction of pain and stress and relief of tensions, as well as questions on sleep induction and quality, will be helpful to confirm and elucidate the means by which the lymphatic system contributes to the reported results. New fields of investigation have been analyzing the lymphatic drainage in cases of multiple sclerosis, correlating the probable action of lymph nodes with immunological parameters29.
For utilization in the daily clinic, in cases of large facial edemas or in other body regions, if a trained professional is not available to perform the manual lymphatic drainage therapy every day, the patients should be trained, encouraged and followed when performing the manual lymphatic drainage by themselves. The physical therapist should always check the movements and pressure of the hands, as well as if the treatment is achieving the expected results.
Considering all aforementioned aspects, the considerable improvement in the reduction of facial edema promoted an increase in self-esteem, especially by reducing the undesirable anti-esthetic effects. The manual lymphatic drainage reduces the pain and utilization of drugs and may anticipate the hospital discharge.
CONCLUSION
The proposed manual lymphatic drainage procedure promoted a significant reduction in facial edema, in pain, and increased interincisal distance. Therefore, this procedure represents an important contribution for the recovery of patients with cleft lip and palate submitted to alveolar bone grafting surgery.
Acknowledgments
The proposed manual lymphatic drainage procedure promoted a significant reduction in facial edema, in pain, and increased interincisal distance. Therefore, this procedure represents an important contribution for the recovery of patients with cleft lip and palate submitted to alveolar bone grafting surgery.
Collaborators
TRR FERREIRA conceived the research and participated in the writing of the article. MZ SABATELLA and AS TRINDADE JUNIOR guided the research and participated in the writing of the article. TMS SILVA and IK TRINDADE-SUEDAM participated in the writing of the article. JRP LAURIS was responsible for planning and statistical analysis and writing of the article.
REFERENCES
1. Silva Filho OG, Ozawa TO, Carvalho RM. Enxerto ósseo alveolar. In: Trindade IEK, Silva Filho OG. Fissuras labiopalatinas: uma abordagem interdisciplinar. São Paulo: Editora Santos; 2007. [ Links ]
2. Ten Cate AR. Embryology of the head, face, and oral cavity. In: Ten Cate AR. Oral histology: development, structure, and function. 7th ed: St. Louis: Elsevier; 2008. p. 32-56.
3. Trindade IK, Mazzottini R, Silva Filho OG, Trindade IE, Deboni MC. Long-term radiographic assessment of secondary alveolar bone grafting outcomes in patients with alveolar cleft. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(3):271-7.
4. Guirro E, Guirro R. Fisioterapia dermato-funcional. 3ª ed. São Paulo: Manole; 2004.
5. Evrard-Bras M, Coupé M, Laroche J, Janbon C. Drainage lymphatique manuel. Rev Prat. 2000;50(11):1199-203.
6. Mayall ACDG, Mayall MR, Cunha JBM, Serva M, Mayall RC. Drenagem manual linfática. Rev Angiol Cir Vasc. 2004;1(3):65- 7.
7. Bose KS, Aggithaya GM. An integrative treatment for lower limb lymphoedema in India. Br J Community Nurs. 2011;16(10):22-7.
8. Korpan MI, Crevenna R, Fialka-Moser V. Lymphedema: a therapeutic approach in the treatment and rehabilitation of cancer patients. Am J Phys Med Rehabil. 2011;90(5 Suppl 1):69- 75. doi: 10.1097/PHM.0b013e31820be160.
9. Woods M. The experience of manual lymph drainage as aspect of treatment for lymphoedema. Int J Palliat Nurs. 2003;9(8):336- 42.
10. Piso DU, Eckardt A, Liebermann A, Gutenbrunner C, Schafer P, Gehrke A. Early rehabilitation of head-neck edema alter curative surgery for orofacial tumors. Am J Phys Med Rehabil. 2001;80(4):261-9.
11. Cobo PC, Díaz PLM, Molina DR, García EV, Vázquez AS, Vega VF. Drenaje linfático manual en el linfoedema facial. Rehabilitación. 2003;37(5):291-3.
12. Szolnoky G, Mohos G, Dobozy A, Kemeny L. Manual lymph drainage reduces trapdoor effect in subcutaneous island pedicle flaps. Int J Dermatol. 2006;45(12):1468-70. doi: 10.1111/j.1365- 4632.2006.03165.x.
13. Arieiro EG, Machado KS, Lima VP, Tacani RE, Diz AM. A eficácia da drenagem linfática manual no pós-operatório de câncer de cabeça e pescoço. Rev Bras Cir Cabeça Pescoço. 2007;36(1):43- 6.
14. Szolnoky G, Szendi-Horváth K, Seres L, Boda K, Kemény L. Manual lymph drainage efficiently reduces postoperative facial swelling and discomfort after removal of impacted third molars. Lymphology. 2007;40(3):138-42.
15. Mottura AA. Face lift postoperative recovery. Aesthetic Plast Surg. 2002;26(3):172-80.
16. Kasseroller RG. The Vodder School: the Vodder method. American Cancer Society lymphedema Workshop Cancer. Cancer. 1998;83(12 Suppl American):2840-2. doi: 10.1002/(SICI)1097- 0142(19981215)83:12B+<2840::AID-CNCR37>3.0.CO;2-5.
17. Leduc A, Leduc O. Drenagem linfática: teoria e prática. 2a ed. São Paulo: Manole; 2000.
18. Barros MH. Fisioterapia: drenagem linfática manual. São Paulo: Robe; 2001.
19. Rubin A, Hoefflin SM, Rubin M. Treatment of postoperative bruising and edema with external ultrasound and manual lymphatic drainage. Plast Reconstr Surg. 2002;109(4):1469-71.
20. Borges FS. Drenagem linfática. In: Borges FS. Dermato-funcional: modalidades terapêuticas nas disfunções estéticas. São Paulo: Phorte; 2006. p. 343-80.
21. Godoy JMP, Godoy MFP, Braile DM. Drenagem linfática e qualidade de vida em paciente com laringectomia. Rev Port ORL. 2000;38(1):47-9.
22. Godoy JMP, Godoy MFG, Meza MC. Godoy & Godoy technique of cervical stimulation in the reduction of edema of the face after cancer treatment. QJM. 2008;101(4):325-6.
23. Williams AF, Vadgama A, Franks PJ, Mortimer PS. A randomized controlled crossover study of manual lymphatic drainage therapy in women with breast cancer-related lymphoedema. Eur J Cancer Care. 2002;11(4):254-61. doi: 10.1046/j.1365- 2354.2002.00312.x.
24. Bernas M, Witte M, Kriederman B, Summers P, Witte C. Massage therapy in the treatment of lymphedema. IEEE Eng Med Biol Mag. 2005;24(2):58-68.
25. Clemens KE, Jaspers B, Klaschik E, Nieland P. Evaluation of the clinical effectiveness of physiotherapeutic management of lymphoedema in palliative care patients. Jpn J Clin Oncol. 2010;40(11):1068-72. doi: 10.1093/jjco/hyq093.
26. Ferrandez JC, Laroche JP, Serin D, Felix-Faure C, Vinot JM. Aspects lymphoscintigraphiques des effets du drainage lymphatique manuel. J Mal Vasc. 1996;21(5):283-9.
27. Warszawski G. Estúdio linfografico de los vasos contralaterales del drenaje de la glabela. Rev Argent Dermatol. 1999;80(1):38- 42.
28. Maus EA, Tan IC, Rasmussen JC, Marshall MV, Fife CE, Smith LA, et al. Near-infrared fluorescence imaging of lymphatics in head and neck lymphedema. Head Neck. 2012;34(3):448-53. doi: 10.1002/hed.21538.
29. Weller RO, Galea I, Carare RO, Minagar A. Pathophysiology of the lymphatic drainage of the central nervous system: Implications for pathogenesis and therapy of multiple sclerosis. Pathophysiology. 2010;17(4):295-306. doi: 10.1016/j. pathophys.2009.10.007.
 Endereço para correspondência:
Endereço para correspondência:
IK TRINDADE SUEDSM
e-mail: ivysuedam@fob.usp.br
Received on: 9/11/2011
Final version resubmitted on: 26/4/2012
Approved on: 5/6/2012













