Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.3 Porto Alegre Jul./Set. 2013
ORIGINAL / ORIGINAL
Shear bond strength of a feldspathic ceramic cemented to a composite resin
Resistência ao cisalhamento de uma porcelana feldspática cimentada a uma resina composta
Luiz Fernando WINCKLERI; Karina Andrea Novaes OLIVIERII; Milton Edson MIRANDAI
I Faculdade São Leopoldo Mandic, Curso de Odontologia, Programa de Pós-Graduação em Prótese Dentária. Rua José Rocha Junqueira, 13, Swift, 13045- 755, Campinas, SP, Brasil.
ABSTRACT
Objective
To evaluate the shear bond strength of a feldspathic ceramic cemented to a composite resin using a resin-based cement, following different treatments to the ceramic surface.
Methods
30 ceramic samples were prepared and divided into 3 groups according to surface treatment: group 1 - control, group 2 - 10% hydrofluoric acid etching for 2 minutes, rinsing under running water and air-drying, group 3 - 10% hydrofluoric acid for 2 minutes, rinsing under running water, air-drying followed by silane. Subsequently, composite resin discs were cemented onto the ceramic specimens using a resin cement and light-curing for 40 seconds. Shear bond strength test was performed on an Emic DL2000 testing machine.
Results
Statistical analysis revealed the following results: there was a significant increase in bond strength in the group etched with hydrofluoric acid when compared with the control, whilst no significance was found in the group treated with silane after etching.
Conclusion
The assessment of failure types under light microscopy revealed a predominance of adhesive failures in the control group and cohesive failures in the remaining groups.
Indexing terms: Composite resins. Dental porcelain. Resin cements. Shear strength.
RESUMO
Objetivo
Avaliar a resistência ao cisalhamento de uma porcelana feldspática, submetida à diferentes tratamentos superficiais, cimentada a uma resina composta, utilizando-se um cimento resinoso.
Métodos
Foram confeccionadas 30 amostras de porcelana, divididas em 3 grupos e receberam os seguintes tratamentos de superfície: Grupo1 - grupo controle; Grupo2 - tratada com ácido fluorídrico 10% por 2 minutos, lavada em água corrente e secada com jatos de ar; Grupo3 - tratada com ácido fluorídrico a 10% por 2 minutos, lavada em água corrente, secada com jatos de ar e silanizada. Na seqüência foi realizada a cimentação dos discos de resina composta na porcelana, com cimento resinoso e fotopolimerizado por 40 segundos. O teste de cisalhamento foi realizado numa máquina Emic DL2000.
Resultados
Após análise estatística chegou-se aos seguintes resultados: houve um aumento significativo na resistência adesiva nos grupos que sofreram condicionamento da superfície da porcelana, em relação ao grupo controle. A aplicação do silano nas porcelanas condicionadas pelo ácido fluorídrico, não foi significante.
Conclusão
Na análise das falhas em microscópio ótico, predominaram as adesivas no grupo controle, e as coesivas nos demais grupos.
Termos de indexação: Resinas compostas. Porcelana dentária. Cimentos de resina. Resistência ao cisalhamento.
INTRODUCTION
Technical and scientific advances in esthetic restorative dentistry combined with the esthetic demands of the modern dental patient constitute a huge challenge for clinicians1. Patients who seek dental treatment often complain of esthetic issues, which can be resolved using prosthodontics. Amongst the esthetic indirect dental materials available, dental ceramics are the most suitable to replace lost tooth structure, due to their optical properties being similar to those of natural teeth. Ceramic inlays and onlays are a type of esthetic restoration that can be bonded to the tooth, thus strengthening the remaining structure and allow conservative tooth preparation. Such restorations require non-retentive contours and, therefore, the inner retentive edges of the prepared tooth must be eliminated, preferably using direct composite resin2. Restorations made with feldspathic ceramics without the addition of a reinforcement material require surface treatment prior to fitting, in order to allow direct bonding to the prepared tooth, thus creating a structural unit and increasing its longevity3-4. Generally speaking, ceramic etching with 10% hydrofluoric acid prior to cementation has shown good clinical results5-6.
The use of silane for cementation of ceramic inlay and onlay has a solid basis in the literature, supported by full ceramic crowns mostly fitted using resin-based cements, which show superior properties to traditional materials, especially in terms of adhesion, low solubility and high resistance4,7-8. Nowadays, a variety of products with proven efficacy are available for such purpose. For feldspathic ceramics without a metal copping, the recommendation is to treat the ceramic surface prior to applying the cement. The aim of the present study was to test the shear bond strength of a feldspathic ceramic bonded to a composite resin using a resin-based cement following different methods of ceramic surface treatment.
METHODS
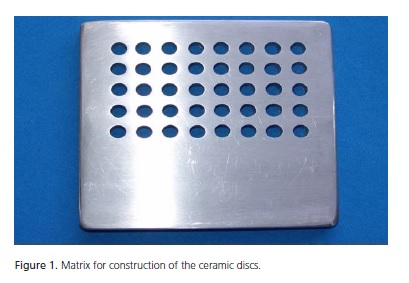
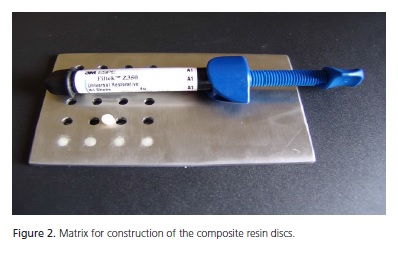
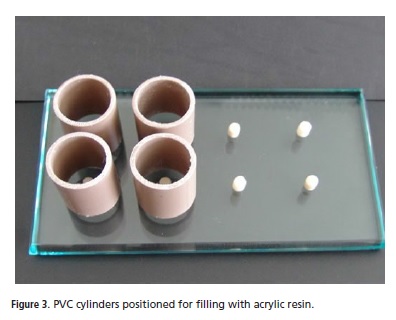
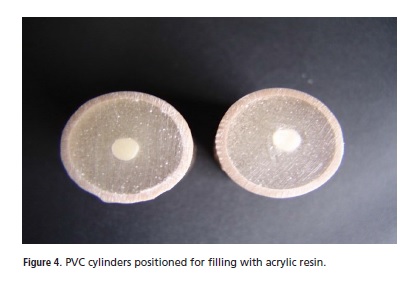
Thirty feldspathic ceramic discs of 5 mm in diameter and 7.5 mm in height9 (Duceram, Dentsply), as well as 30 discs of composite resin (Z350, 3M of Brazil, Sumaré, Brazil) measuring 4 mm in diameter and 5 mm in height were used. The ceramic samples were made from a stainless steel matrix (Figure 1) at the Itamar Dental Prosthetics Lab, situated in the town of Chapecó (SC). The composite resin specimens were made at a private dental practice in Chapecó (SC), using stainless steel matrices (Figure 2). One side of the ceramic discs was glued to a glass plate using an instant universal adhesive. Thirty sections of PVC pipe (Tigre, Sao Paulo, Brazil) were prepared, measuring 2.5 cm in diameter and 3 cm in height, and positioned over each sample (Figure 3) and stabilized onto a glass plate using utility wax. Acrylic resin was prepared according to the manufacturers instructions, mixing powder and liquid in a glass receptacle using a spatula until complete homogenization. The mixture was then poured into the PVC tubes until full. Complete polymerization was achieved within 10 minutes. The entire test set was removed from the glass plate and filed down using sandpaper (3M, Sumaré, Brasil) in order to reduce abrasiveness. Initially, a 400-grade sandpaper was used to remove excess acrylic resin from the ceramic surface, followed by 600 to obtain a flat, smooth surface (Figure 4). The cylinders were rinsed under running water to remove the remaining particles of powder and then analyzed using a magnifying glass (4x magnification), to confirm cleanliness of the ceramic.
Surface treatment of the ceramic
Group 1 did not receive any surface treatment. Group 2 was etchd with 10% hydrofluoric acid for 2 minutes, rinsed under running water and dried with blasts of air. Group 3 was treated with 10% hydrofluoric acid for 2 minutes, rinsed under running water, dried with blasts of air and then underwent application of silane.
Surface treatment of the composite resin
In order to reduce abrasiveness, the composite resin discs were filed using 400 and 600 grades of sandpaper (3M, Sumaré, Brazil). They were then roughened 3 times in both the horizontal and vertical planes using a 4138 diamond burr (KG Sorensen), brushed, rinsed under running water and dried with blasts of air.
Construction of the test specimens
RelyX U-100 cement was individually applied to the surface of the ceramic samples with a spatula, as per the manufacturer's instructions. The resin discs were then fitted over the cement, using light manual pressure assisted by a universal testing machine programmed and calibrated to ensure a cement thickness of 50 μm. The excesses were removed and light-cured individually for 40 seconds.
Shear Bond Strength test
The shear bond strength test was performed on a universal EMIC DL2000 machine, using a chiselled Trd 23 cell at a speed of 0.5 mm/min and a compression of 200 kgf. The test specimens were fixed to the machine so that the cylinders remained at a right angle with the force applied by the mono-angled chisel (Figure 5).
The testing machine was linked to a computer, allowing the test to be monitored by the TESC Software, version 3.1, which demonstrated the relationship between the load applied and the displacement at the time of failure. This was represented graphically via a curve of maximum tension force at the abscissa point and deformity on the ordinate axis. At the point of rupture, the movement ceased and the data were processed for analysis.
The present study (no: 07/303) adhered to the principles of ethics as per the Declaration of Helsinki (2000), in addition to specific Brazilian legislation.
RESULTS
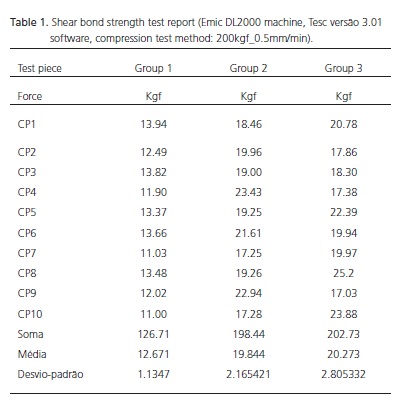
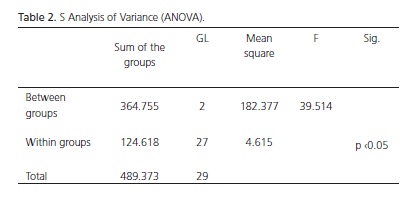
TThe results obtained for each sample, automatically processed and saved as maximum force values, expressed in Kilogram force (Kgf), were analyzed using ANOVA (p <0.05) (Table 1 and 2).
There was no significant difference within each group. A significant difference was observed for groups 2 and 3, when compared to the control group, which demonstrated the effectiveness of the surface treatments. There was no significant difference between group 2 and 3.
DISCUSSION
Single tooth restorations with feldspathic ceramic are often chosen because its optical properties, chemical inertia, shade and shape stability. The development of bonding techniques between the ceramic and the adhesive system has minimized the problem with fractures. It is based on hydrofluoric acid etching of the ceramic (to create mechanical retention), and the use of silane, which bonds the silica (within the porcelain) to the organic matrix (from the adhesive system) by means of siloxane bonds4,10-11.
Adhesive ceramic restorations strengthen the remaining tooth structure and allow for more conservative preparations. Nonetheless, such restorations require non-retentive wall contours, i.e., the elimination of inner retentive areas, which can be preferably achieved using composite resin12.
The results from the shear bond strength test revealed a significant difference in groups 2 and 3 when compared to the control group, thus highlighting the importance of the mechanical and chemical bonds between the resin cement and the ceramic13, however between groups 2 and 3 the difference did not reach significance, which is a similar outcome as obtained by Sorensen et al.14 and Suliman et al.15, who tested different surface treatments and concluded that the combination of hydrofluoric acid and silane created an optimal bond strength, yet only slightly better that obtained using hydrofluoric acid alone. Roulet et al.16 identified mechanical retention as the most important factor in the bond strength between ceramic and resin cement when investigating different surface treatments.
Senda et al.17 and Kupiec et al.18 reported that hydrofluoric acid is effective as a ceramic etchant, as it creates satisfactory mechanical retentions, which has been confirmed in the present study.
According to Kina et al.4, resin cements are adhesive, have low solubility and high resistance, so when used in combination with adhesive systems, they yield predictable bonding between the tooth structure and several types of materials, as long as their surfaces are treated adequately in order to promote mechanical retentions. For feldspathic ceramics, the treatment of choice should be hydrofluoric acid etching.
Tylka & Stewart19, in a comparative study using scanning electron microscopy, observed the roughness created by hydrofluoric acid on the ceramic surface, in which the resin cement penetrated and promoted strong mechanical retention. This may explain the type of failures observed in this study, i.e., cohesive failures in the groups etched with hydrofluoric acid.
This study has demonstrated the importance of ceramic surface etching with hydrofluoric acid to promote mechanical retention. Furthermore, the use of silane did not significantly increase the shear bond strength.
Silane promotes a chemical bond between resin cement and feldspathic ceramic. Although no significant increase in bond strength was observed in this study using such method, its use should not be discouraged. Specific studies on the use of silane, its properties and its role on the longevity of such type of bonding should be performed to verify, for instance, whether the chemical bond promoted by silane would contribute towards minimizing microleakage and delay the discoloration occasionally observed in the interface ceramic/resin cement20.
The advent of novel ceramics based on alumina, zirconia, or those inforced with Yttrium, amongst others, is currently seen. Literature reports advocate that the use of some type of surface treatment and/or silane increase the bond strength between ceramic and resin cement21-24.
Literature reports revealed that despite a vast diversity of commercial brands a certain level of standardization of materials and methodology existed, which was what inspired this investigation.
CONCLUSION
It is possible to conclude that the results obtained in this study have shown a significant increase in bond strength in the ceramic groups that underwent surface treatment. Furthermore, silane application following hydrofluoric acid etching was not significant. Light microscopy (Bioval, USA) revealed a predominance of adhesive failures in the control group and cohesive failures in the remaining groups.
Collaborators
LF WINCKLER, KAN OLIVIERI and ME MIRANDA participated in all stages of collating this manuscript.
REFERENCES
1. Fradeani M. Esthetic analysis: a systematic aproach prosthetic treatment. Milão: Quintessence Publishing; 2006. [ Links ]
2. Pacheco JFM, Goes MF. Influência do tratamento de superfície na resistência a tração da colagem do Artglass. Rev ABO Nac. 2001;8(6):337-42.
3. Bottino MA, Quintas AF, Myashita E. Reabilitação oral: metal free. São Paulo: Artes Médicas; 2002.
4. Kina S, Bruguera A, Romanini JC. Restaurações estéticas cerâmicas. Maringá: Dental Press Editora; 2007.
5. Lu R, Harcourt JK, Tyas MJ, Alexander B. An investigation of the composite resin/porcelain interface. Aust Dent J. 1992;37(1):12- 9. doi: 10.1111/j.1834-7819.1992.tb00827.x.
6. Stangel I, Nathanson D, Hsu CS. Shear strength of the composite bond to etched porcelain. J Dent Res. 1987;66(9):1460-5. doi: 10.1177/00220345870660091001.
7. Begazo CC, de Boer HD, Kleverlaan CJ, van Waas MA, Feilzer AJ. Shear bond strength of different types of luting cements to an aluminum oxide-reinforced glass ceramic core material. Dent Mater. 2004;20(10):901-7.
8. Franco EB, Ferreira EGP. Avaliação da resistência de união entre porcelana e resina composta, em função de diferentes tratamentos superficiais. JBD Rev Ibero-Am Odontol. 2005;4(14);160-5.
9. Goyatá FR. Avaliação da resistência ao cisalhamento de uma porcelana feldspática cimentada a um cerômero submetido a diferentes tratamentos de superfície [dissertação]. Campinas: Faculdade São Leopoldo Mandic; 2006.
10. Bowen RL. Adhesive bonding of various materials to hard tooth tissues: lV. Bonding to dentin, enamel and fluorapatite improved by the use of a surface-active comonomer. J Dent Res. 1965;44(5):906-11.
11. Buonocore MGA. Simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34(6):849-53.
12. Aida M, Hayakawa T, Mizukawa K. Adhesion of composite to porcelain with various surface conditions. J Prosthet Dent. 1995;73(5):464-70. doi: 10.1016/S0022-3913(05)80076-9.
13. Soares CJ, Soares PV, Pereira JC, Fonseca RB. Surface treatment protocols in the cementation process of ceramic and laboratoryprocessed composite restorations: a literature review. J Esthet Restor Dent. 2005;17(4):224-35.
14. Sorensen JA, Engelman MJ, Torres TJ, Avera SP. Shear bond strength of composite resin to porcelain. Int J Prosthodont. 1991;4(1):17-23.
15. Suliman AA, Swigt EJ, Perdigão J. Effects of surface treatment and bonding agents on bond strength of composite resin to porcelain. J Prosthet Dent. 1993;70(2):118-20.
16. Roulet JF, Soderholm KJM, Longmate J. Effects of treatment and storage conditions on ceramic/composite bond strength. J Dent Res. 74(1):381-7. doi: 10.1177/00220345950740011501.
17. Senda A, Suzuki M, Jordan RE. The effect of florides and hydrofloric acids on porcelain surfaces. J Dent Res. 1989;68:236.
18. Kupiec KA, Wuertz KM, Barkmeier WW, Wilwerding TM. Evaluation of porcelain surface treatments and agents for composite-toporcelain repair. J Prosthet Dent. 1996;76(2):119- 24. doi: 10.1016/S0022-3913(96)90294-2.
19. Tylka DF, Stewart GP. Comparison of acidulated phosphate fluorite gel and hidrofloric acid etchants for porcelain-composite repair. J Prosthet Dent. 1994;72(2):121-7. doi: 10.1016/0022- 3913(94)90067-1.
20. Lacy IM, Laluz J, Watanabe G, Dellinges I. Effect of porcelain surface treatment on the bond composite. J Prosthet Dent. 1988;60(3):288-91.
21. Cavalcanti AN, Foxton RM, Watson TF, Oliveira MT, Giannini M, Marchi GM. Bond strength of resin cements to a zirconia ceramic with different surface treatments. Oper Dent. 2009;34(3):280-7. doi: 10.2341/08-80.
22. Fabianelli A, Pollington S, Papacchini F, Goracci C, Cantoro A, Ferrari M, et al. The effect of different surface treatments on bond strength between leucite reinforced feldspathic ceramic and composite resin. J Dent. 2010;38(1):39-43. doi: 10.1016/j. jdent.2009.08.010.
23. Re D, Augusti D, Sailer I, Spreafico D, Cerutti A. The effect of surface treatment on the adhesion of resin cements to Y-TZP. Eur J Esthet Dent. 2008;3(2):186-96.
24. Blatz MB, Phark JH, Ozer F, Mante FK, Saleh N, Bergler M, et al. In vitro comparative bond strength of contemporary selfadhesive resin cements to zirconium oxide ceramic with and without air-particle abrasion. Clin Oral Investig. 2010;14(2):187- 92. doi: 10.1007/s00784-009-0278-0.
 Endereço para correspondência:
Endereço para correspondência:
LF WINCKLER
e-mail: fernandowinckler@desbrava.com.br
Received on: 6/7/2010
Final version resubmitted on: 31/1/2011
Approved on: 26/4/2011













