Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.4 Porto Alegre Out./Dez. 2013
ORIGINAL / ORIGINAL
Non-surgical periodontal therapy for the treatment of chronic periodontitis
Terapia periodontal não-cirúrgica no tratamento da periodontite crônica
Mari Raquel Botlender TROJAHNI; Robert Carvalho da SILVAII; Júlio César JOLYII
I Faculdade São Leopoldo Mandic, Curso de Odontologia, Programa de Pós-Graduação em Periodontia. Rua José Rocha Junqueira, 13, Swift, 13045-755. Campinas, SP, Brazil.
II Universidade Estadual de Campinas, Faculdade de Odontologia. Piracicaba, SP, Brazil.
ABSTRACT
Objective
The aim of this split-mouth controlled study was to compare the clinical benefits of administering subgingival 10% Doxycycline (test group) with a placebo gel (control group), as an adjunct to mechanical therapy in the treatment of chronic periodontitis.
Methods
Fifteen patients with moderate to severe chronic periodontitis, with at least 2 pairs of comparable contralateral defects (pocket depth ≥6 mm), were selected. The subjects were submitted to initial periodontal treatment, which included oral hygiene advice and supra-gingival ultrasonic instrumentation at least one month before starting the experiments. Clinical attachment level (CAL), probing depth (PD) and gingival margin level (GML) were assessed at baseline, and after 3 and 6 months, using a manual probe (PCP-15, Hu Friedy). Plaque index was less than 20% throughout the study period.
Results
Comparison between groups indicated a PD reduction and CAL gain greater in the test group than in the control group at 3 and 6 months; however, no significant difference was shown (p>0,05).
Conclusion
The findings suggest that 10% Doxycycline hyclate applied subgingivally as an adjunct to conventional periodontal treatment, did not promote additional benefit when compared to scaling and root planing with a placebo gel in patients with moderate to severe chronic periodontitis.
Indexing terms: Chronic periodontitis. Dental scaling. Doxycycline.
RESUMO
Objetivo
Comparar os benefícios clínicos da administração de gel composto de hiclato de doxiciclina a 10% (grupo teste) em relação ao gel placebo (grupo controle) associado à terapia mecânica no tratamento da periodontite crônica.
Métodos
Foram selecionados 15 pacientes com periodontite crônica moderada a severa, e um mínimo de 2 pares de defeitos contralaterais comparáveis (profundidade de sondagem ≥ 6mm). Os pacientes foram submetidos ao tratamento periodontal inicial, que incluiu instrução de higiene oral, instrumentação ultra-sônica pelo menos um mês antes do início do experimento. Os parâmetros clínicos: nível clínico de inserção (NCI), profundidade de sondagem (PS), e nível da margem gengival (NG) foram aferidos no início, após 3 e 6 meses utilizando uma sonda periodontal manual (PCP-15, Hu Friedy). O índice de placa se manteve inferior a 20% durante todo o estudo.
Resultados
As comparações entre os grupos indicaram que redução na PS e ganho no NCI foi maior no grupo teste do que no grupo controle aos 3 e 6 meses, porém, não houve diferença estatisticamente significante (p>0,05).
Conclusão
Esses achados sugerem que a aplicação subgengival de hiclato de doxiciclina gel a 10%, como adjunto ao tratamento periodontal convencional não promoveu benefício adicional ao tratamento com raspagem e alisamento radicular com aplicação de gel placebo, em pacientes com periodontite crônica moderada a severa.
Termos de indexação: Periodontite crônica. Raspagem dentária. Doxiciclina.
INTRODUCTION
The objective of conventional periodontal therapy is to eliminate the subgingival biofilm at sites affected by periodontal disease, which may be associated to progressive destruction of supportive periodontal tissue1. Scaling and root planing alter the composition of the subgingival flora, however, factors such as probe depth, bifurcation areas, and the presence of microorganisms within the cement limit the effectiveness of instrumentation2-4.
The idea of using locally applied medications in periodontal pockets as a treatment method has been studied for more than 20 years. The clinical efficacy is derived from the capacity of the material to maintain its concentration within the periodontal pocket for a given time period. Antimicrobial medications have been most studied. The majority of the medications have been tested in association with scaling and root planing, although some have also been studied as monotherapies5-6.
A slow sustained-release antimicrobial permits the application of medication at the affected site by means of a biodegradable system; therefore adequate drug levels are achieved without the need for daily application and removal. Direct application also allows the use of small quantities, therefore minimizing systemic absorption of the active ingredient7.
Studies using the application of Doxycycline gel associated with scaling and root planing have demonstrated a significant reduction in probe depth and improvements in clinical parameters8-10. These studies, therefore, highlight the importance of longitudinal studies to confirm the advantages of drug therapy in association with periodontal instrumentation.
METHODS
Fifteen patients were selected from the dental clinic at the Center for Dental Research, São Leopoldo Mandic University. Four male and 11 healthy female patients aged between 25 and 68 years with moderate to severe chronic periodontitis and a minimum of 20 teeth, were selected. Smokers, patients with known systemic diseases, and those using medications that may interfere with tissue repair, such as anticoagulants or corticosteroids, were excluded from the study. Teeth with pulpal pathology were also excluded.
Four sites from different teeth in the same dental arch, with two in each hemi-arch at a probe depth of ≥6mm, were selected. For the test group, the sites in each hemiarch were randomly treated with non-surgical periodontal instrumentation, followed by application of 10% Doxycycline gel containing Methocel (-6-(hydroxymethyl)- 5-methoxy-2-[4,5,6-trimethoxy-2-(methoxymethyl)oxan- 3-yl]oxyoxane-3,4-diol-nomenclature IUPAC-) and 10% Doxycycline hyclate (MASE Chemical and Pharmaceutical Products Ltda., Cambuci, São Paulo, Brazil). The control group was treated in the same way, however, after scaling and root planing a placebo gel (Methocel) only was applied. This formula has already been used in other split-mouth double-blind randomized control studies11-13.
The patients underwent initial periodontal treatment consisting of supragingival ultrasonic debridement and oral hygiene advice at least one month before starting the experiment. This procedure allowed the clinician to perform scaling and root planing therapy in a single session so that the medication could be applied. In addition, it provided the opportunity to level out the individuals, as this was a small group study. During the initial examination, which was performed immediately prior to the experimental procedures, dichotomous plaque and bleeding indices, as well as the biometric parameters of probing depth (distance between the gingival margin and the base of the pocket), level of gingival margin (distance between the cemento-enamel junction and the gingival margin) and clinical attachment level (the sum of the probing depth to the gingival level), using a manual periodontal probe (PCP-15, Hu Friedy), to the nearest millimeter10.
Six sites around each tooth, posterior or anterior, were measured, however, only the deepest site was considered. All clinical parameters were collected again at 3 and 6 months. Professional prophylaxis and patient motivation were performed during these periods, with the plaque index maintained at below 20% throughout the study. Probing guides were not performed in this study, however, the researcher aimed to use the same probe tip and angulation, based on photographic evaluation. The researcher calibrated the force applied during probing prior to the start of the experiment. The same operator performed each stage of the study.
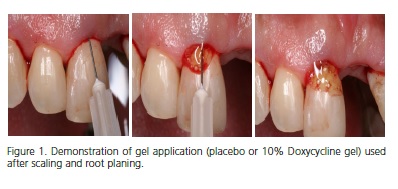
2% Lidocaine with epinephrine, 1:100.000 (ALPHACAINE-DFL) was administered before periodontal instrumentation. The experimental procedure consisted of non-surgical periodontal instrumentation using specific manual curettes (Hu Friedy) for the treated surfaces, followed by 10% Doxycycline hyclate or placebo gel application. All of the curettes used were sufficiently sharpened before each procedure, and instrumentation efficacy was subjectively evaluated clinically by obtaining a hard, smooth and polished surface, using a manual scaled probe (PCP-15, Hu Friedy). The pockets were rigorously irrigated with physiological saline solution to remove clots and debris. The sites were randomly treated using syringes containing the test drug or placebo, which were coded A and B by the researcher responsible (RCS). This study was double-blinded, with the coding kept confidential during the entire experimental period, and neither the operator nor the patients knew which drug was being applied to which side. The gel was applied to the deepest part of the pocket until spillover at the gingival margin, as shown in Figure 1. The same operator treated the test and control group sites on the same day.
This study adhered to the principals of ethics as per the Declaration of Helsinki (2000), as well as the specific legislations of Brazil (CEP n 06/198).
RESULTS
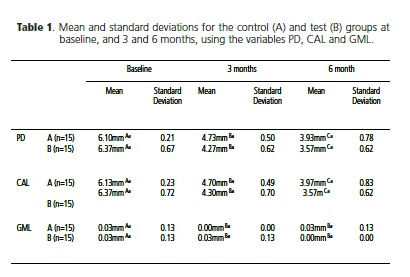
The mean values of the clinical parameters for the patients with moderate to severe chronic periodontitis treated with scaling and root planing, and application of either the placebo or the Doxycycline gel, are shown in Table 1.
The Gingival Margin Level (GML) did not reveal a significant difference between the groups at the specified time intervals, nor within the same group at different time periods. Only one patient had a gingival margin measurement of more than zero, with the remaining patients demonstrating a GML, which coincided with the cemento-enamel junction.
The values for probing depth (PD) revealed no significant difference between the groups at baseline. However, using repeated measures Analysis of Variance, complemented by the Tukey multiple comparisons test at a significance level of 5%, a significant difference was demonstrated between group and time, both for the control and test groups, with baseline being significantly higher than all other time intervals. In terms of PD, when comparing the group treated with Doxycycline gel (test group) to the group treated using the placebo gel (control group) at 3 and 6 months, means of 4.27 mm versus 4.73 mm (difference = 0.46 mm) and 3.57 mm versus 3.93 mm (difference 0.36 mm), respectively, were demonstrated. The mean at 3 months was also significantly higher than at 6 months. There was no significant difference in terms of test and control group mean at all time intervals, therefore the test group did not present a significant gain in probing depth compared to the control group (p>0.05). At 3 months, p=0.098 suggests a trend towards significance between the treatments used.
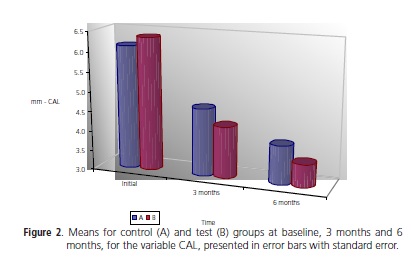
The variations in the Clinical Attachment Level (CAL) did not demonstrate a significant difference between the study groups at baseline. Comparing the CAL of the test and control groups at 3 and 6 months, the means were 4.30 versus 4.70 mm (difference = 0.40 mm) and 3.57 versus 3.97 mm (difference = 0.40 mm), respectively. Using repeated measures Analysis of Variance complemented by the Tukey multiple comparisons test at a significance level of 5%, a significant interaction within each group with regards to time was shown, both in the control and test groups, with the mean at baseline being significantly higher than at all other time periods. The mean at 3 months was also significantly higher than at 6 months. At all time periods, no significant difference was shown with regards to the mean of the groups (p>0.005).
DISCUSSION
There are different rationales for the topical application of subgingival antimicrobials in clinical periodontology, namely the persistence of active sites following surgical and non-surgical treatment, or a recurrence during periodontal support therapy14. The advantage of this procedure is that it is less aggressive towards the periodontal hard tissue and causes less dentinal sensitivity, which is a common occurrence after conventional scaling.
In pharmacokinetic analysis of Doxycycline in the Gingival Crevicular Fluid (GCF), saliva and blood, the antimicrobial effect was shown to be limited to the sites where the drug was applied. Doxycycline gel possesses clinical and pharmacokinetic properties that effectively release and maintain antimicrobial levels within the periodontal pocket for at least a week, without the need for greater drug retention within the periodontal tissues15.
In this study, a split-mouth approach was used, in which both treatments were applied in the same patient. Multiple studies with the same design have been published evaluating the local release of these agents16-19.
The present study was designed to evaluate the benefits of the use of Doxycycline gel as an adjunct to conventional periodontal scaling and root planing in patients with moderate to severe chronic periodontitis. The combined therapy used demonstrated favorable results in terms of improvements in the evaluated clinical parameters. The same results were seen in the study, which evaluated the clinical and microbiological effects on the controlled local application of Doxycycline as an adjunct to mechanical treatment for periodontitis. The clinical parameters were measured at baseline, 3 months, and 1, 2 and 3 years. Gingival biofilm samples were collected at each time interval and evaluated. Significant reductions in bleeding on probing, probing depth and clinical attachment level were only observed for the test group, which received scaling and Doxycycline gel, at 3 months and for a minority of bacterial species at 2 years. Despite the short-term results in favor of the use of Doxycycline gel, annual applications have not shown better clinical or microbiological results when compared with results following mechanical treatment only20.
Therapy association has been the aim of many studies. A clinical study used the following treatments: Scaling and root planing + Doxycycline gel application (test group), and scaling and root planing only (control group). The gains in clinical attachment level were greater in the test group. Concluding that the use of Doxycycline could be an important adjunct in the treatment of severe periodontitis in smokers14. The clinical effect of topical Doxycycline gel application with non-surgical periodontal therapy was also evaluated. The test group presented significantly improved probing depth and clinical attachment levels after 6 months, when compared to the control group. Another 6-month study indicated that subgingival instrumentation combined with local Doxycycline application at deep periodontal sites justified it as a treatment for chronic periodontitis15.
Both groups evaluated in this study presented a reduced probing depth within the evaluated time periods, in addition to a gain in clinical attachment level after 3 and 6 months; however, no significant difference was shown at the same time period between the groups. These results corroborate other studies, which suggest that subgingival application of Doxycycline gel results in an additional clinical improvement in periodontal therapy in patients with Type I Diabetes, with a significant difference between the study groups noted only after 12 months16. The combined use of Doxycycline gel and scaling and root planing to suppress odontopathogens was also evaluated. The sites that received both scaling and root planing in association with subgingival Doxycycline gel application, as well as those sites that received scaling only, showed similar levels of periodontopathogens before and after treatment, demonstrating that there was no significant difference with the use of Doxycycline gel. In accordance with the findings of the present study, studies which compared the use of Doxycycline gel with scaling and root planing resulted in very similar clinical changes at all times in both studies. The mean gain of clinical attachment level was practically the same for both groups during the research.
The likely explanations for not observing a significant difference between the groups could be associated to the sample and time intervals evaluated. It is known that the larger the number of sites, the lower the numeric difference to reach significance. In addition, the sites that received Doxycycline could show more stability in the long-term, and the control group sites could begin to lose attachment over a longer follow-up, whilst those of the test group could be maintained. The results of the present study demonstrated that the deeper sites (≥7mm) of the test group obtained greater attachment gain (≥2mm).
Although clinical studies that compared different drugs to treat periodontitis have shown that patients treated with Doxycycline gel obtained a significant increase in clinical attachment gain when compared to patients receiving other drugs, the use of all drugs has shown satisfactory clinical gain21-24. When tested as an adjunct to conventional periodontal therapy, beneficial results were reported25-27.
Many drugs have been used as a single treatment system, therefore, without the use of scaling and root planing. Some authors have shown that monotherapy has its benefits in the treatment of chronic periodontitis. Controlled clinical studies have concluded that the application of Doxycycline gel was superior to sanguinarine chloride hydrate and the vehicle control at reducing probing depth at all evaluated time periods. The results suggested that Doxycycline gel in a biodegradable system was an effective way to reduce clinical signs of chronic periodontitis, with a safe and benign profile28. The aim of the present study was to perform manual instrumentation prior to the application of Doxycycline to disorganize the biofilm, favoring drug action. In monotherapies, this preceding disorganization does not exist.
In this study, the experimental sites received scaling and root planing followed by the application of 10% Doxycycline gel, with no patient loss throughout the study. The patients demonstrated effective biofilm control during the research, maintaining indices lower than 20%.
The results revealed changes in PD and CAL of 2.5 mm or more in the experimental group, which was higher than that of the control group.
The primary indication for Doxycycline gel, in addition to all other locally applied antimicrobials, is its use as an adjunct to conventional scaling and root planing treatment29. Studies have shown significant improvements in the evaluated clinical parameters, which suggest the use of 10% Doxycycline hyclate gel to treat subgingival periodontitis, producing an additional favorable clinical result to conventional periodontal therapy in patients with chronic periodontitis. Every case, however, should be evaluated individually, and it should be used when a significant clinical result is anticipated30.
CONCLUSION
From the results obtained in this 6-month study, it can be concluded that no significant difference was shown between the groups at the time intervals studied. In accordance with the results, subgingival application of 10% Doxycyline hyclate gel as an adjunct to conventional periodontal treatment did not promote any additional benefit when compared to scaling and root planing with the application of a placebo gel in patients with moderate to severe chronic periodontitis.
Collaborators
MRB TROJAHN was responsible for the research and writing the article. RC SILVA participated in the research, interpretation of results and writing the article. JC JOLY participated in analysis and interpretation of the results, and writing the article.
REFERENCES
1. Garret S, Johnson L, Drisko CH, Adams DF, Bandt C, Beiswanger B. Two multi-center studies evaluating locally delivered doxycycline hyclate, placebo control, oral hygiene, and scaling and root planing in the treatment of periodontitis. J Periodontol. 1999;70(5):490-503. doi: 10.1902/jop.1999.70.5.490. [ Links ]
2. Rosenberg ES, Evian CI, Listgarden MA. The composition of the subgingival microbiota after periodontal therapy. J Periodontol. 1981;52(8):435-441. doi: 10.1902/jop.1981.52.8.435.
3. Loos B, Claffey N, Egelberg J. Clinical and microbiological effects of root debridement in periodontal furcation pockets. J Clin Periodontol. 1988;15(7):453-63. doi: doi: 10.1111/j.1600- 051X.1988.tb01600.x.
4. Fleischer HC, Mellonig JT, Brayer WK, Gray JL, Barnnet JD. Scaling and root planing efficacy in multirooted teeth. J Periodontol. 1989;60(7):402-9. doi: 10.1902/jop.1989.60.7.402.
5. Finkelmann RD, Williams RC. Local delivery of chemotherapeutic agents inperiodontal therapy: Has its time arrived? J Clin Periodontol. 1998;25(11 Pt 2):943-6. doi: 10.1111/j.1600- 051X.1998.tb02395.x.
6. Killoy WJ. The clinical significance of local chemoterapies. J Clin Periodontol. 2002;29:22-9.
7. Kormann KS. Controlled-release local delivery antimicrobials in periodontics: prospects for the future. J Periodontol. 1993;64(8 Suppl):782-91. doi: 10.1902/jop.1993.64.8s.782.
8. Polson AM, Southard GL, Dunn RL, Yewev GL, Godowski KC, Polson AP, et al. Periodontal pocket treatment in beagle dogs using subgingival doxycycline from a biodegradable system. I. Initial clinical responses. J Periodontol. 1996;67(11):1176-84. doi 10.1902/jop.1996.67.11.1176.
9. Polson AM, Garret S, Stoller NH, Bandt CL, Hanes PJ, Killoy WJ, et al. Multi-center comparative evaluation of subgingivally delivered sanguinarine and doxycycline in the treatment of periodontitis.II. Clinical results. J Periodontol. 1997;68(2):119- 126. doi: 10.1902/jop.1997.68.2.119.
10. O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972;43(1):38. doi: 10.1902/jop.1972.43.1.38.
11. Machion L, Andia DC, Benatti BB, Carvalho MD, Nogueira-Filho GR Casati M, et al. Locally delivered doxycycline as an adjunctive therapy to scaling and root planing in the treatment of smokers: a clinical study. J Periodontol. 2004;77(4):606-13. doi:10.1902/ jop.2006.050087.
12. Wennstrom JL, Newman HN, MacNeill SR, Killoy WJ, Griffiths GS, Gillam DG, et al. Utilisation of locally delivered doxycycline in non-surgical treatment of chronic periodontitis. A comparative multi-centre trial of 2 treatment approaches. J Clin Periodontol. 2001;28(8):753-61. doi: 10.1034/j.1600-051X.2001.280806.x.
13. De Lima MAF, Cury CC, Palioto DB, Duro AM, Da Silva RC, Wolf LF. Therapy with adjuntive doxycycline local delivery in pacients with Type 1 diabetes mellitus and periodontitis. J Clin Periodontol. 2004;31(8):648-53. doi: 10.1111/j.0303- 6979.2004.00576.x.
14. Eickholz P, Kim TS, Schacher B, Reitmeir P, Burklin T, Ratka- Kruger P. Subgingival topical doxycycline versus mechanical debridement for supportive periodontal therapy: a single blind randomized controlled two-center study. Am J Dent. 2005;18(6):341-6.
15. Kim TS, Bürklin T, Schacher B, Ratka-Krüger P, Schaecken MT, Rengggli HH, et al. Pharmacokinetic profile of a locally administered doxycycline gel in crevicular fluid, blood, end saliva. J Periodontol. 2002;73(11):1285-91. doi: 10.1902/ jop.2002.73.11.1285.
16. Stabholz A, Nicholas AA, Zimmerman GJ, Wikesjo UM. Clinical and antimicrobial effects of a single episode of subgingival irrigation with tetracycline HCI or chlorhexidine in deep periodontal pockets. J Clin Periodontol. 1998;25(10):794-800. doi: 10.1111/j.1600-051X.1998.tb02372.x.
17. Ciancio SG, Charles MC, Leung M. Tissue concentration and localization of tetracycline following site-specific tetracycline fiber therapy. J Periodontol. 1992;63(10):849-53. doi: 10.1902/ jop.1992.63.10.849.
18. Fine JB, Harper DS, Gordon JM, Hovliaras CA, Charles CH. Shortterm microbiological and clinical effects of subgingival irrigation with an antimicrobial mouthrinse. J Periodontol. 1994;65(1):30- 6. doi: 10.1902/jop.1994.65.1.30.
19. Wong MY, Lu CL, Liu CM, Hou LT. Microbiological response of localized sites with recurrent periodontitis in maintenance patients treated with tetracycline fibers. J Periodontol. 1999;70(8):861-8. doi:10.1902/jop.1999.70.8.861.2005;18(6):341-6.
20. Bogren A, Teles RP, Torresyap G, Haffajee AD, Socransky S, Wennstrom J. Locally delivered doxycycline during supportive periodontal therapy: a 3 - year study. J Periodontol. 2008;79(5):827-35. doi: 10.1902/jop.2008.070515.
21. Jorgensen MG, Safarian A, Daneshmand N, Keim RJ, Slots J. Initial antimicrobial effect of controlled-release doxycycline in subgingival sites. J Periodontol. 2004;39(5):315-9. doi: 10.1111/j.1600-0765.2004.00742.x.
22. Salvi GE, Mombelli A, Mayfield I, Rutar A, Suvan J, Garret S, et al. Local antimicrobial therapy after initial periodontal treatment. J Clin Periodontol. 2002;29(6):540-50. doi: 10.1034/j.1600- 051X.2002.290611.x.
23. Breault LG, Spadaro SE. Local chemotherpeutics as an adjunct to scaling and root planing. Dental Assistant. 200473(6):20-4.
24. Killoy WJ. The use of locally-delivered chlorhexidine in the treatment of periodontitis. Clinical results. J Clin Periodontol. 1998;25(11 Pt 2):953-8. doi: 10.1111/j.1600-051X.1998. tb02397.x.
25. Rodrigues IFG, Machion L, Casati MZ, Notici Junior FH, De Toledo S, Sallum AW, et al. Clinical evaluation of the use of locally delivered chlorhexidine in periodontal maintenance therapy. J Periodontol. 2007;78(4):624-8. doi: 10.1902/jop.2007.060317.
26. Paolantonio MP, D'Angelo M, Grassi RF, Perinetti G, Piccolomini R, Pizzo G, et al. Clinical and microbiologic effects of subgingival contolled-release delivevery of chlorhexidine chip in the treatment of periodontitis: a multicenter study. J Periodontol. 2008;79(2):271-82. doi: 10.1902/jop.2008.070308.
27. Cosyn J, Wyn I, Rouck T, Sabzevar MM. Subgingival chlorhexidine varnish administration as an adjunte to same-day full-mouth root planing. I. Clinical observations. J Periodontol. 2007;78(3):430- 7. doi: doi:10.1902/jop.2007.060221.
28. Grisi DC, Salvador SL, Figueiredo LC, Souza SLS, Novaes Junior SB, Grisi MFM. Effect of controlled-release chlorhexidine chip on clinical and microbilological parameters síndrome. J Clin Periodontol. 2002;29(10);875-81. doi: 10.1034/j.1600- 051X.2002.291001.x.
29. John V, Philips G. Locally delivered antimicrobials in periodontal treatment. J Indiana Dent Assoc. 2002;81(2):10-4.
30. Lotufo R, Kantorski K, Zimmermann G. Antibióticos de liberação local e controlada em periodontia: minociclina e doxiciclina. RGO - Rev Gaúcha Odontol. 2003;51(5):395-7.
 Endereço para correspondência:
Endereço para correspondência:
MRB TROJAHN
e-mail: marirbt@yahoo.com.br
Received on: 13/7/2009
Final version resubmitted on: 22/3/2010
Approved on: 31/3/2010













