Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.4 Porto Alegre Out./Dez. 2013
ORIGINAL / ORIGINAL
Silorane-based composite as repair material: a six-month randomized clinical trial
Resina composta à base de silorano como material de reparo: estudo clínico randomizado de seis meses
Daniela Araújo Veloso POPOFFI; Thalita Thyrza de Almeida SANTA ROSAII; Wallace de Freitas OLIVEIRAII; Isabella Pereira MARQUESII; Cláudia Silami de MAGALHÃESI; Allyson Nogueira MOREIRAI
I Universidade Federal de Minas Gerais, Faculdade de Odontologia. Av. Antônio Carlos, 6627, Pampulha, 31270-901, Belo Horizonte, MG, Brasil.
II Universidade Estadual de Montes Claros, Faculdade de Odontologia. Montes Claros, MG, Brasil.
ABSTRACT
Objective
This study investigated the clinical performance of a silorane-based composite resin when used for repairing conventional composite restorations.
Methods
Defective dimethacrylate-based composite resin restorations were randomly assigned to one of two treatment groups: Control group - Adper SE Plus + Filtek P60 (3M/ESPE, St. Paul, EUA) and Test Group - P90 Adhesive System + Filtek P90 (3M/ESPE, St. Paul, EUA). All repaired restorations were evaluated at baseline, and at six-month recall. The parameters examined were marginal adaptation, anatomic form, surface roughness, marginal discoloration, post-operative sensitivity and secondary caries. The restorations were classified according to modified USPHS criteria. Mann-Whitney and Wilcoxon tests were used to compare the groups.
Results
Of the 100 restorations repaired in this study, 93 were reexamined at baseline and 91 at 6-month recall. Drop-out was about 9%. No statistically significant differences were found between the materials for all clinical criteria, at baseline and at 6-month recall (p > 0.05). No statistically significant differences were registered (p > 0.05) for each material when compared for all clinical criteria, at baseline and at 6-month recall. The hypothesis tested in this randomized controlled clinical trial was accepted.
Conclusion
After the six-month evaluations, silorane-based composite exhibit a similar performance compared to dimethacrylate-based composite when used as repair material.
Indexing terms: Composite resins. Corrective maintenance. Dental restoration repair. Silorane resins.
RESUMO
Objetivo
Investigar o desempenho clínico de uma resina de baixa contração à base de silorano quando utilizada para reparar restaurações convencionais de resina composta.
Métodos
Restaurações defeituosas de resina composta à base de dimetacrilato foram aleatoriamente reparadas por um de dois grupos de tratamento: Grupo Controle - Adper SE Plus + Filtek P60 (3M/ESPE, St. Paul, EUA) e Grupo Teste - Sistema adesivo P90 + Filtek P90 (3M/ESPE, St. Paul, EUA). Todas as restaurações reparadas foram avaliadas em baseline e ao longo de 6 meses. Os parâmetros analisados foram a adaptação marginal, forma anatômica, rugosidade superficial, descoloração marginal, sensibilidade pós-operatória e lesões de cárie. As restaurações foram classificadas de acordo com os critérios do Serviço de Saúde Público dos Estados Unidos modificados. Os testes de Mann-Whitney e Wilcoxon foram utilizados para comparar os grupos.
Resultados
Das 100 restaurações reparadas neste estudo, 93 foram examinadas uma semana após terem sido reparadas - baseline e 91 após 6 meses. A perda foi de aproximadamente 9%. Nenhuma diferença estatisticamente significativa foi encontrada entre os materiais para todos os critérios clínicos, em baseline e ao longo de 6 meses (p> 0,05).
Conclusão
A hipótese testada neste ensaio clínico controlado randomizado foi aceita. Após 6 meses de avaliações, resinas compostas à base de silorano apresentaram desempenho clínico semelhante às resinas compostas à base de dimetacrilato quando utilizadas para reparar restaurações de resina composta à base de dimetacrilato.
Termos de indexação: Resinas compostas. Manutenção corretiva. Reparação de restauração dentária. Resinas de silorano.
INTRODUCTION
Composite resins are today's most widely used direct restorative material. Their main advantages are the adhesive capacity allowing for minimal cavity preparation and superior esthetics1. Since the introduction of dental resin-based composites, intense research has attempted to develop materials with acceptable mechanical and physical properties to significantly improve their longevity and aesthetic quality2.
Recently, in order to minimize the effects of shrinkage, an innovative monomer system was made available for dental restorations - silorane. Obtained from the reaction of oxirane and siloxane molecules, this material contains traditional filler particles, whereas the conventional resin is replaced by silorane monomers. While siloxanes are known for their hydrophobicity, oxiranes are known for their low shrinkage3-5.
Results from in vitro studies have shown that silorane-based composites demonstrate the lowest polymerization shrinkage as well as more ambient light stability. The new system also has the lowest sorption and water solubility and a lower diffusion coefficient than conventional monomers. Parameters such as tensile modulus, flexural strength and biocompatibility in toxicology tests are comparable to dimethacrylate-based composite3,6-9.
Despite extensive improvements in the mechanical properties of resin-based tooth-colored restorative materials, volumetric shrinkage and subsequent contraction stress arising during the polymerization reaction are still significant drawbacks10. Shrinkage may also cause microleakage, marginal staining, and gap formation, this one an important factor in the development of caries, because it may act as a retention groove4,11-12.
Reducing shrinkage and the stress generated by polymerization may positively influence marginal integrity. Imperfect margins result in marginal discoloration and secondary caries lesions, the most important cause for the replacement of defective restorations13.
However, according to the philosophy of ‘minimum intervention' operative dentistry, with the exception of conditions in which there is a fracture of the resin restoration, staining of the entire resin/tooth interface and secondary caries, defective restorations should be first evaluated for the possibility of repair, rather than being routinely replaced14. This approach allows preservation of sound tooth structure15-16 being considered a viable longterm clinical procedure for treatment of restorations17-19.
Clinical studies involving composite resin repairs have shown that, when properly planned, the repairs may increase the clinical longevity of restorations. Thus, once in vitro studies suggest that bonding of silorane-based composites to old dimethacrylate-based composites may be a viable clinical procedure20-22, it would be desirable to evaluate the clinical performance of this new system for making repairs. The hypothesis tested in this randomized controlled clinical trial was that low-shrinkage silorane-based composites exhibit a similar performance when compared to conventional dimethacrylate-based composites when used to repair composite resin restorations.
METHODS
Study design
This prospective randomized clinical trial had the repaired restorations like observation units. Patients aged 18 to 56 years with 100 defective composite resin restorations participated in this study. They were routinely assigned for treatment at the operative dentistry clinic, School of Dentistry, Federal University of Minas Gerais.
The inclusion criteria were: patients who were older than 18 years of age and signed a consent form approved by the Institutional Ethics Committee; patients with no contraindications for dental treatment; patients who had class I or class II composite resin restorations with occlusal defects and no diagnosis of caries according to clinical and bite-wing radiographic exams; patients who had restorations which scored at least Bravo according to Modified United States Public Health Service (USPHS) clinical criteria (Chart 1). The exclusion criteria were: patients with contraindications for regular dental treatment according to their medical history; patients with xerostomy, including those taking medications that are proven to significantly reduce salivary flow; patients with visible plaque index (VPI) > 30%; patients with defective restorations, unacceptable for repairs, that scored Charlie (Modified USPHS clinical criteria).
his clinical trial was conducted in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects (2000) and approved by the local Institutional Ethics Committee (ETIC 0546.0.203.000-09). 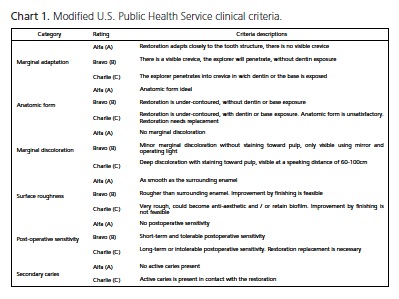
Study methods
The restorations were examined one week after they were repaired for baseline assessment, and at sixmonth. Two examiners independently evaluated all repaired restorations by direct observation, using a plane buccal mirror and a WHO model explorer. Calibration exercises revealed an inter-examiner agreement ratio ≥ 0.78. Since there was disagreement on the rating, the clinicians reexamined the repaired restoration together and arrived at a joint final decision. The clinical criteria examined were marginal adaptation, anatomic form, surface roughness, marginal discoloration, post-operative sensitivity and secondary caries. The examiners classified all restoration as Alpha, Bravo or Charlie, according to modified USPHS clinical criteria.
Treatment groups
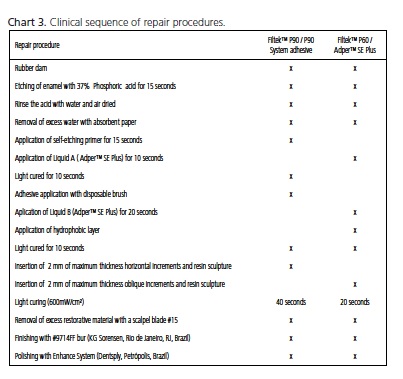
The same operator repaired all defective composite resin restorations in order to minimize preparation variability. Defective surfaces of the restorations were explored using high-speed spherical diamond burs (KG Sorensen, São Paulo, SP, Brazil) compatible with the size of the defect in a hand piece with air-water coolant, beginning with the removal of the restorative material in the area of the defect as well as any stained and soft tooth tissues. The restorations were randomly assigned to one of two treatment groups: Control group (n = 50): Repair with a self-etching primer (Adper SE Plus, 3M /ESPE, St. Paul, MN, USA) and a dimethacrylate-based composite (Filtek P60 Posterior Restorative, 3M/ESPE, St. Paul, MN, USA); Test group (n = 50): Repair with a self-etching primer (P90 System Adhesive Self-Etch Primer and Bond, 3M/ESPE, St. Paul, MN, USA) and a low-shrinking silorane-based composite (Filtek P90 Low Shrink Posterior Restorative, 3M/ESPE, St. Paul, MN, USA) (Chart 2).
Rubber dam isolation was used for the restorative procedures. The surfaces of restorations and enamel margins were etched with 37% phosphoric acid (Magic Acid Gel, VIGODENT/COLTENE, Rio de Janeiro, Brazil) before adhesive procedures, being the materials used according to manufacturer's recommendations (Chart 3). 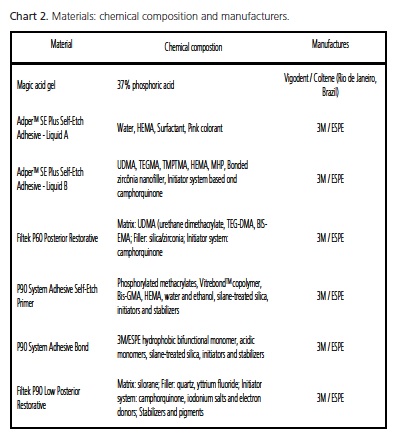
Outcome measurements and statistical analysis
At baseline and six-month recall, all restorations received a clinical rating like Alpha, Bravo or Charlie. The ordinal dependent variable was the percentage of Alpha, Bravo or Charlie ratings.
Data management and analysis were done using a statistical analysis system (SPSS 15.0.1 for Windows, SPSS, Chicago, IL, USA). Mann-Whitney test was used to assess differences between the materials tested and for all clinical criteria, at baseline and at 6-month recall examination (p = 0.05). Wilcoxon test was used to compare each composite resin for all clinical criteria at baseline examinations and at 6-month recall (p = 0.05).
RESULTS
Drop-out in this study was about 9%. Of the 100 repaired restorations, 93 (50 for Filtek P60 and 43 for Filtek P90) were examined at baseline and 91 at the 6-month recall (48 for Filtek P60 and 43 for Filtek P90). The main reasons for restorations being repaired were marginal defects (81%) and loss of anatomic form (19%).
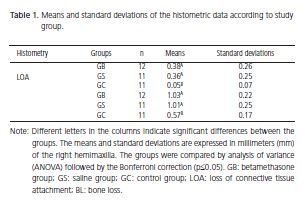
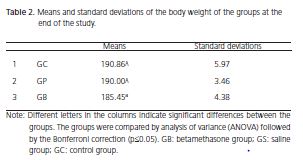
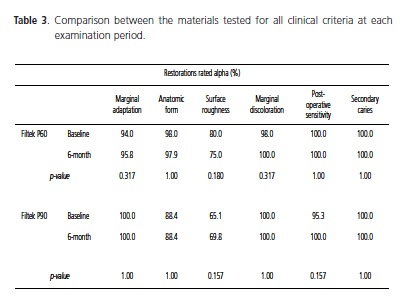
Table 1 summarizes the frequency of Alpha and Bravo ratings for restorations in both groups for each clinical criterion at baseline and at 6-month recall examination. No restoration received Charlie ratings. Table 2 shows the comparison between the materials tested for all clinical criteria, at baseline and at six-month recall examination. No statistically significant difference between the materials was found (p > 0.05). Table 3 shows the comparison between baseline and six-month recall examination for each material independently, for all clinical criteria. No statistically significant difference was found in any criteria between the examination periods (p > 0.05).
DISCUSSION
The low-shrinkage silorane-based composites exhibited a similar clinical performance to dimethacrylatebased composites when used for repairing dimethacrylatebased composite restorations after a six-month observation period, confirming, thus, the null hypothesis tested. Dropout in this study was about 9%. This response rate is in accordance with other similar clinical studies that had rates of 0% to 15% for the first year recall4,17,19,23-24.
In general, approximately 50% of resin-based composite restorations are replaced after seven years of service, and the main reasons are secondary caries, marginal defects, discoloration, degradation/wear and loss of anatomic form17-19. For many years, despite the subjectivity of restoration removal criteria, total replacement has been the most common treatment in general dental practice19,25. Nevertheless, it is known that when a restoration is replaced, there is a loss of healthy dental tissue, including areas away from localized defects17. Repairs are alternative treatments that can increase the longevity of restorations, and several studies have shown a positive impact after first, second and third year observation periods17-19,26. Thus, this longitudinal prospective study aimed to discuss the effectiveness of a new low-shrinkage composite - silorane - as a repair material
Silorane is a nonmethacrylate-based resin that has been introduced in order to control polymerization shrinkage. The new monomer is obtained from the reaction of oxirane and siloxane molecules and was developed with the primary purpose of overcoming some drawbacks related to polymerization of dimethacrylatebased composites, such as radical oxygen inhibition, polymerization shrinkage, polymerization stress, water sorption and instability of conventional monomers in aqueous systems. As a result, silorane has the ability to compensate shrinkage by opening the oxirane ring during polymerization, reducing volume shrinkage to 1% from 1.7- 3.5% in dimethacrylate-based materials. Due to the presence of siloxane species, the hydrophobicity is also increased3-4.
Silorane-based composites have been thoroughly investigated by in vitro tests, and promising results have been obtained regarding biocompatibility and mechanical characteristics, including reduced polymerization shrinkage3,5. However, in vitro studies are limited in predicting short- and long-term clinical conditions, and laboratory findings should be substantiated by clinical investigations.
In the present study, the main reasons for repairing restorations were marginal defects and loss of anatomical form. Six modified USPHS criteria - marginal adaptation, anatomic form, surface roughness, marginal discoloration, post-operative sensitivity and secondary caries - were used to verify the clinical performance of repairs performed on failed dimethacrylate-based composite restorations. No statistically significant differences between the groups were found for all clinical parameters tested at each time interval (p > 0.05). The frequency of no change in ratings from six-month recall examinations compared to baseline was much higher than the frequency of downgrades from an Alpha to Bravo rating.
It is a consensus that the information provided by USPHS criteria is too broad and may also lead to a misinterpretation as a good clinical performance since any changes over time are not easily detected by the limited sensitivity in short-term clinical investigation17. Despite these considerations, it is the most widely used method for clinical evaluations of restorations worldwide, and the main reason for adopting it relies on the fact that it can be compared to previous studies. In addition, this criteria involves visual inspection as well as the use of a dental explorer17.
Laboratory studies have shown lower values of polymerization shrinkage related to silorane-based composites, but it is difficult to show the effects in clinical studies, mainly because in short-term six-month evaluations, many factors may not still influenced the final result3. In the current study, no statistically significant differences between the materials tested were found for marginal adaptation for the entire six-month follow-up. There are no results from clinical trials that have tested silorane-based composite as repair material available for comparison. However, a recent study investigated marginal adaptation of a low-shrinkage silorane-based composite and compared it with a dimethacrylate-based composite material across one-year interval4. Even though such study had outcomes related to total-replaced restorations, their results from one-year investigations are in accordance with the findings from the present study.
No statistically significant differences have been found between the materials tested for secondary caries, which are usually associated with marginal integrity and marginal adaptation is usually associated with reduced polymerization shrinkage. Favourable results were, thus, expected for a low-shrinkage resin-based composite5. Furthermore, within six months, the patients in the study did not develop carious lesions, most likely because patients with inadequate oral hygiene (VPI > 30%) and decreased salivary flow were excluded.
When each composite resin was evaluated independently at baseline and after six months no statistically, no difference was found too. In general, restorations remained stable and unchanged over the six-month observation period. Previous studies that have investigated the longevity of dimethacrylate-based restoration by minimal intervention have found the same good performance when dimethacrylate-based composites were used as repair materials17-19.
Again, no statistically significant difference between the materials was found for surface roughness at any recall examination. This result is in agreement with studies investigating the longevity of dimethacrylate-based composite restorations by minimal interventions17-19. These studies found that surface roughness returned to their original values from the defective restoration values after only a three-year recall examination.
In a recent study related to the repair potential of composite resin materials, the highest bond strength when a dimethacrylate-based composite was used as substrate was when Filtek P90 was used as the repair material and the P90 System as the adhesive. Although it is customarily assumed that the bond between old and new composite is micromechanical, data from when Filtek P90 was the substrate suggest that there is a possibility of chemical bonding, most likely because products that contain a silane coupling agent have improved wetability of the substrate surface in addition to higher binding of siloxane to inorganic filler particles. In Filtek P90, these are silanated ceramics22. It may explain the results from marginal discoloration, when no statistically significant difference between the two materials was found at recall examinations.
At baseline examination, the low incidence of restorations that received Bravo rating for post-operative sensitivity can be explained by the use of a self-etching bonding system in both treatment groups. These systems make the smear layers part of the hybrid layer, providing better penetration of the monomers onto the collagen fibers of the demineralized dentin. At follow-up, the same good performance was observed for all composites, likely because resin-based agents may provide pulp protection as long as the dentin is sealed by hydrophilic resins23. Initial post-operative sensitivity has been reported in clinical studies with resin-based composites, but the sensitivity generally decreases during the first weeks after placement of restorations23.
CONCLUSION
Thus, after six months, this clinical trial shows that low-shrinkage silorane-based composites exhibited a similar performance to the conventional dimethacrylatebased composites when used to repair composite resin restorations. The reduced polymerization shrinkage assigned to silorane-based composites did not establish better clinical performance, indicating that laboratory findings should be substantiated by clinical investigations.
Collaborators
DAV POPOFF, responsible for the literature review, performance of the operative procedures, final writing of the manuscript and data statistical analysis. TTA SANTA ROSA, IP MARQUES and CS MAGALHÃES, responsible for evaluation of the operative procedures and writing of the manuscript. WF OLIVEIRA and AN MOREIRA, responsible for the literature review and partial performance of the operative procedures.
REFERENCES
1. Min SH, Ferracane J, Lee IB. Effect of shrinkage strain, modulus, and instrument compliance on polymerization shrinkage stress of light-cured composites during the initial curing stage. Dent Mater. 2010;26(10):1024-33. doi: 10.1016/j.dental.2010.07.002. [ Links ]
2. Leprince J, Palin WM, Mullier T, Devaux J, Vreven J, Leloup G (2010). Investigating filler morphology and mechanical properties of new low-shrinkage resin composite types. J Oral Rehabil. 2010;37(5):364-76. doi: 10.1111/j.1365-2842.2010.02066.x.
3. Weinmann W, Thalacker C, Guggenberger R. Siloranes in dental composites. Dent Mater. 2010;21(1):68-74. doi: 10.1016/j. dental.2004.10.007.
4. Schmidt M, Kirkevang LL, Hǿrsted-Bindslev P, Poulsen S. Marginal adaptation of a low-shrinkage silorane-based composite: 1-year randomized clinical trial. Clin Oral Invest. 2011;15(2):291-5. doi: 10.1007/s00784-010-0446-2.
5. Ilie N, Hickel R. Macro- micro- and nano-mechanical investigations o silorane and methacrylate-based composites. Dent Mater. 2009;25(6): 810-9. doi: 10.1016/j.dental.2009.02.005.
6. Eick D, Kotha SP, Chappelow CC, Kilway KV, Giese G, Glaros AG, Pinzino CS. Properties of silorane-based dental resins and composites containing a stress-reducing monomer. Dent Mater. 2007;23(8):1011-7. doi: 10.1016/j.dental.2006.09.002.
7. Condon JR, Ferracane JL. Assessing the effect of composite formulation on polymerization stress. J Am Dent Assoc. 2000;131(4):497-503.
8. Palin WM, Fleming GJP, Burke FJT, Marquis PM, Randall RC. The influence of short and medium term water immersion on the hydrolytic stability of novel low shrink dental composites. Dent Mater. 2005;21(9):852-63. doi: 10.1016/j.dental.2005.01.004.
9. Soh MS, Yap AUJ, Sellinger A. Physicomechanical evaluation of low-shrinkage dental nanocomposites based on silsesquioxane cores. Eur J Oral Sci. 2007;115(3):230-8. doi: 10.1111/j.1600- 0722.2007.00449.x.
10. Marchesi G, Breschi L, Antoniolli F, DiLenarda R, Ferracane J, Cadenaro M. Contraction stress of low-shrinkage composite materials assessed with different testing systems. Dent Mater. 2007;26(10): 947-953. doi: doi: 10.1016/j.dental.2010.05.007.
11. Giachetti L, Scaminaci Russo D, Bambi C, Grandini R. A review of polymerization shrinkage stress: current techniques for posterior direct resin restorations. J Contemp Dent Pract. 2007;7(4):79- 88.
12. Totiam P, Gonzalez-Cabezas C, Fontana MR, Zero DT. A new in vitro model to study the relationship of gap size and secondary caries. Caries Res. 2007;41(6):467-73. doi: 10.1159/000107934.
13. Rodriguez GDR, Pereira SNA. Current trends and evolution on dental composites. Acta Odontol Venez. 2008;46:1-18.
14. Tyas MJ, Anusavice KJ, Frencken JE, Mount GJ. Minimal intervention dentistry: a review. Int Dent J. 2000;50(1):1-12.
15. Mjör IA, Reep RL, Kubilis PS, Mondragon BE. Change in size of replaced amalgam restorations: a methodological study. Oper Dent. 1998;23(5):272-7.
16. Popoff DAV, Gonçalves FS, Ferreira RC, Magalhães CS, Moreira AN, Mjör IA. Repair of amalgam restorations with conventional and bonded amalgam: an in vitro study. Rev Odonto Ciênc. 2010;25(2):154-8. doi: 10.1590/S1980-65232010000200009.
17. Gordan VV, Shen C, Riley J, Mjor IA. Two-Year clinical evaluation of repair versus replacement of composite restorations. J Esthet Dent. 2006;18(3):144-54. doi: 10.1111/j.1708- 8240.2006.00007.x.
18. Moncada G, Fernández E, Martin J, Arancibia C, Mjor I, Gordan VV. Increasing the longevity of restorations by minimal intervention: a two-year clinical trial. Oper Dent. 2008;33(3):258- 64. doi: 10.2341/07-113.
19. Moncada G, Martin J, Fernández E, Hampel MC, Mjör IA, Gordan VV. Sealing, refurbishment and repair of class I and class II defective restorations: A three-year clinical trial. J Am Dent Assoc. 2009;140(4):425-32.
20 Lührs AK, Görmann B, Jaker-Guhr S, Geurtsen W (2011). Repairability of dental siloranes in vitro. Dent Mater. 2011;27(2):144-9. doi: 10.1016/j.dental.2010.09.009.
21. Ivanovas S, Hickel R, Ilie N. How to repair fillings made by silorane-based composites. Clin Oral Invest. 2010;15(6):915-22. doi: 10.1007/s00784-010-0473-z.
22. Mannenut C, Sakoolnamarka R, Tyas MJ. The repair potential of resin composite materials. Dent Mater. 2011;27(2):20-7. doi: 10.1016/j.dental.2010.09.006.
23. Gordan VV, Shen C, Watson RE, Mjor IA. Four-year clinical evaluation of self-etching primer and resin-based restorative material. Am J Dent. 2005;18(1):45-9.
24. Gordan VV, Mondragon E, Watson RE, Garvan C, Mjör IA. A clinical evaluation of a self-etching primer and giomer restorative material. J Am Dent Assoc. 2007;138(5):621-7.
25. Çehreli SB, Arhun N, Celik C. Amalgam repair: quantitative evaluation of amalgam-resin and resin-tooth interfaces with different surface treatments. Oper Dent. 2010;35(3):337-44. doi: 10.2341/09-135-L.
26. Christensen GJ. When and how to repair a failing restoration. J Am Dent Assoc. 138:1605-7.
27. Ilie N, Hickel R. Silorane-based dental composite: behavior and abilities. Dent Mater J. 2006;25(3):445-54. doi: 10.4012/ dmj.25.445.
28. Eick JD, Smith RE, Pinzino CS, Kostoryz EL. Stability of silorane dental monomers in aqueous systems. J Dent. 2006;34(6):405- 10. doi: 10.1016/j.jdent.2005.09.004.
29. Papadogiannis D, Kakaboura A, Palaghias G, Eliades G (2010). Setting characteristics and cavity adaptation of low-shrinking resin composites. Dent Mater. 25(12):1509-16. doi: doi: 10.1016/j.dental.2009.
30. Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Science Committee Project 2/98-- FDI World Dental Federation study design (Part I) and criteria for evaluation (Part II) of direct and indirect restorations including onlays and partial crowns. J Adhes Dent. 2007;9(Suppl):121-47.
 Endereço para correspondência:
Endereço para correspondência:
DAV POPOFF
e-mail: danielavelloso@yahoo.com.br
Received on: 21/3/2012
Final version resubmitted on: 4/6/2012
Approved on: 1/10/2012













