Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.4 Porto Alegre Out./Dez. 2013
ORIGINAL / ORIGINAL
Biological exposure-related injuries in dental health-care workers
Prevalência de acidentes ocupacionais nos profissionais da Odontologia envolvendo instrumentos perfurocortantes
Cristina Dutra VIEIRAI; José Ivany dos SANTOSII; Magaly Maria CABRALII; Jacson Félix da SILVAI
I Polícia Militar de Minas Gerais, Comissão de Biossegurança do Centro Odontológico. Av. do Contorno, 3300, Santa Efigênia, 30110-080, Belo Horizonte, MG, Brasil.
II Polícia Militar de Minas Gerais, Centro de Referência e Controle e Tratamento de HIV/AIDS. Belo Horizonte, MG, Brasil.
ABSTRACT
Objective
This study was conducted during a 13-year period to analyze the number and profile of biological exposure-related injuries among dental health-care workers in a Public Health Service in Belo Horizonte, Brazil.
Methods
All occupational accidents involving dental staff, dentists, dental assistants, dental technicians (n=215), and those involved in processing environmental surfaces and waste collection (n=12), and body fluids associated with sharp instruments were recorded. Our data were collected from January 1999 to May 2011.
Results
A total of 41 exposures were reported. The majority of biological exposures occurred in females aged 26 to 35 years. The most frequently involved devices were syringe needles and the most frequently involved body fluid was blood. Despite the existence of an institutional guideline, it was observed that 12.2% of health-care workers did not follow the post-exposure recommendations. Additionally, 14.6% of the dental care workers did not receive hepatitis B vaccination.
Conclusion
Our results suggest that it is important to provide more safety training programs and information about occupational risks to all dental healthcare personnel.
Indexing terms: Accidents occupational. Accident prevention. Occupational risks.
RESUMO
Objetivo
Para conhecer o número e o perfil de acidentes ocupacionais envolvendo material perfurocortante, entre os profissionais da Odontologia de um Serviço de Saúde Pública, foram levantados dados no período de 1999 a 2011.
Métodos
Foram levantados os acidentes ocupacionais em uma instituição de assistência à saúde odontológica, pública e autárquica, na cidade de Belo Horizonte, em Minas Gerais. O quadro clínico é composto de 215 profissionais de saúde que oferecem consultas em diversas especialidades e 12 profissionais na equipe de serviços gerais. Foram colhidos dados de todos os acidentes com material perfurocortante, envolvendo material biológico, e que ocorreram no período de janeiro de 1999 a maio de 2011.
Resultados
Foi registrado um total de 41 (quarenta e um) acidentes e os profissionais que mais se acidentaram pertenciam ao gênero feminino e possuíam idade entre 26 e 35 anos. Um percentual de acidentados ainda não havia se vacinado contra o vírus da Hepatite B. O sangue foi a secreção mais frequentemente envolvida nos acidentes e as agulhas corresponderam à maioria das injúrias. Apesar da existência de um protocolo institucional, 12,2% dos profissionais acidentados não realizaram acompanhamento completo pós-exposição.
Conclusão
Os dados suscitam a necessidade de um maior conhecimento da equipe da Odontologia a respeito dos riscos e da prevenção dos acidentes ocupacionais envolvendo material perfurocortante e também do protocolo institucional.
Termos de indexação: Acidentes de trabalho. Prevenção de acidentes. Riscos ocupacionais.
INTRODUCTION
According to the Centers of Disease Control and Prevention (CDC)1, avoidance of occupational blood exposure is the primary way to prevent transmission of many infectious agents such as hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) in health-care settings. Occupational exposure can occur through percutaneous injuries with needle sticks or cuts from other sharps instruments with infected blood, other infected fluids, or even by contact of nose, eye, and mouth mucous, or skin with patients' blood2.
In the United States, the CDC3 reported that each year, 385,000 injuries with needle sticks and other sharp instruments occurred in hospital-based personnel, with an average of 1,000 injuries each day. This number does not take into account other health settings and, according to the CDC3, there are scientific evidences that indicate that more than 50% of health-care personnel do not report their occupational percutaneous injuries.
According to Sepkowitz and Eisenberg4, Occupational Safety and Health Administration (OSHA) data from 1992 to 2002 showed that a total of 67,363 workers died from occupational injuries in the United States. Among these were 28 health-care workers who died from complications associated with needles stick injuries.
The Brazilian law defines occupational accident as a "typical accident with Workplace Accident Communication (WAC), causing body injury or functional disorder leading to death, permanent or temporary loss or reduction of labor capability"5-6. According to the Brazilian Statistical Yearbook6, in 2006, the National Institute for Social Security (INSS) reported 503,900 work-related accidents. Social assistance and health-care workers represented 8.3% of all accidents.
This study aimed to report occupational accidents involving injuries from needle sticks and other sharp instruments, in a Dental Public Health-Care Service during a 13-year period (1999–2011), to evaluate their characteristics, and to determine the need for additional safety precautions and educational training.
METHODS
The present survey was performed in a Public Dental Health-Care Service in Belo Horizonte city, Brazil. The incidence and characteristics of the injuries with dental health-care personnel (dentists, dental assistants, and dental technicians) and those involved in processing environmental surfaces and waste collection were evaluated. The clinical staff was composed of 215 workers offering consultations in several dental specialties such as Endodontics, Oral and Maxillofacial Surgery, Orthodontics and Dentofacial Orthopedics, Pediatric Dentistry, Periodontics, Prosthodontics, Geriatric Dentistry, Stomatology, Dental Implants, Dental Emergencies, and Home Care. The average number of consultations was 7.418/month7. The team responsible for processing environmental surfaces and waste collection was composed of 12 members. The workers attended annual training programs on infection control, including the prevention of occupational risks. All data concerning biological exposure-related injuries from January 1999 to May 2011 were evaluated by a multidisciplinary team composed of a dentist, a nurse, a physician, and a health-care aide. The authors collected data from the Reference Center for Treatment and Control of HIV (CRCT-AIDS) records. Information regarding the known source/patient (name, gender, age, home address, and telephone number; source of the accident, HBV and HIV serology, and CD4 count), the injured worker (name, gender, age, marital status, place and time of the accident, and vaccination status against HBV) and the accident (injured body part, instrument and body fluid involved, and depth) were considered. Other data collected included the following: cleaning and local use of antiseptics; the result of patient and worker's blood tests; the necessity for and the proposed post-exposure chemoprophylaxis; the patient's signature and consent for medical followup during 180 days; blood exam results (HBV, HCV, and HIV). All data were confidential and were handled only by the authors. The worker and the patient involved in the accident received counseling before and after the exams. Ethics approval for the study was granted by the Military Hospital Ethics Committee (Protocol number 21). Data were analyzed by EPI InfoTM version 3.5.3, for Windows, CDC (USA) updated in January 26, 2011.
RESULTS
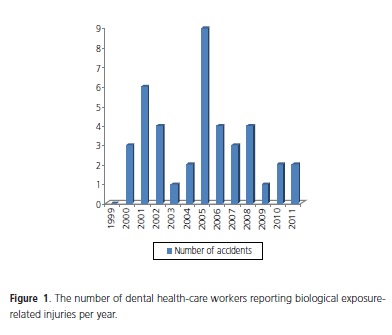
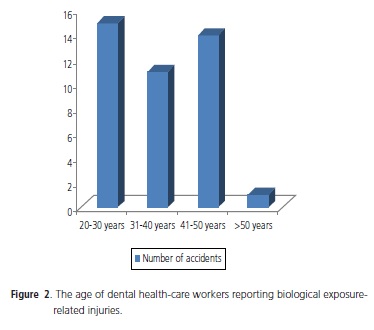
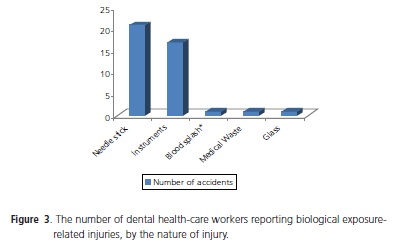
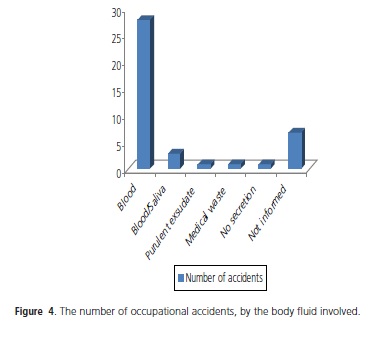
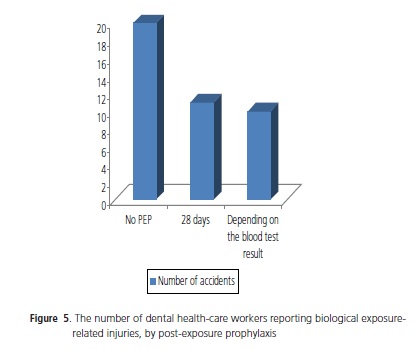
Figure 1 shows the number of injured workers, per year, from 1999 to 2011. There were 41 occupational accidents, involving 34 females (83%) and 7 males (17%). Forty members of the clinical staff (20 dentists and 20 dental assistants and dental technicians) and one environmental cleaning worker were registered. Sharp instruments and body fluids were involved in almost all accidents. Most workers belonged to the clinical staff group (97.6%) and 2.4% belonged to cleaning staff. The age of the injured personnel was between 23 and 58 years (mean: 35.8 years and median: 34.0 years) (Figure 2). Despite the literature recommending hepatitis B vaccination8, 14.6% of injured workers did not follow the advice and 26.8% was negative for hepatitis B surface antibody (anti-HBs). The instrument most frequently involved in occupational injuries was needle sticks (51.2%), followed by clinical instruments such as drills, endodontic files, dental explorers, periodontal scalers, and tips of periodontal ultrasonic scalers (Figure 3). Blood was the body fluid most commonly involved in the accidents (Figure 4). In 31.7% of accidents, it was impossible to identify the individual source of the accident. Institutional guidelines recommend performing blood tests immediately after the accident, on the injured employee and the individual source (when known). After consent, the patient's blood was tested for HIV (enzyme-linked immunosorbent assay [ELISA]), HBV (HBsAg), and HCV. One of the sources tested seropositive for HIV (2.4%) and all of them were negative for HBV and HCV. Beyond the mentioned examination for the individual source, the worker's blood was also quantitatively tested for anti-HBs levels. The results for HIV (ELISA) and HBV were negative for all employees and 75.6% exhibited anti-HBs levels of ≥10 mIU/mL. All unvaccinated and incompletely vaccinated workers had anti-HBs levels of <10 mIU/mL. Despite alleged vaccination, five members of the dental staff did not have a protective concentration of anti-HBs (<10 mIU/ mL). All unvaccinated and incompletely vaccinated workers received revaccination. After the procedure, one worker (2.4%) still did not have a protective concentration of anti- HBs (nonresponder) and should be considered susceptible to HBV infection. The majority of injured workers (97.6%) took care of the wound immediately after the accident, cleansing it thoroughly with soap and water and using a 70% alcohol solution when indicated. Only one employee (2.4%) did not take care of the wounded tissue. The guideline also recommended post-exposure prophylaxis (PEP) that should be taken for 28 days after the accident or a shorter period, depending on the individual source's blood test results (Figure 5). The treatment of choice is a combination of zidovudine (300 mg) and lamivudine (150 mg) (tradename Biovir), one tablet two times a day. PEP was recommended in 51.2% of the injuries and was taken for 28 days in 26.8%. Despite the institutional guideline and training, six workers (14.6%) did not follow postexposure recommendations.
DISCUSSION
Several studies published worldwide discuss the incidence of biological exposure-related injuries in healthcare settings, including dentistry. Similar to our findings where female was the predominant gender (83.9%), Donatelli9 recorded occupational accidents involving dental staff (dentists, dental assistants, and graduate and postgraduate students) from 2000 to 2004, and also found predominantly female workers (78%) associated with accidents. Shah et al.10 and Martins et al.11 studied the same group and also found that female was the prevalent gender (71% and 52.9%, respectively). Donatelli9 reported that 74.9% of the injuries occurred in workers aged between 20 to 29 years. In the present study, 74.9% of the accidents occurred in workers from 26- to 35-yearsold. The difference in age may be due to institutional characteristics.
A survey12 performed from January 1997 to December 2003 in a Brazilian hospital recorded 65 sharps injuries among health-care workers. Nursing assistants (47.7%) was the category most frequently involved in accidents, followed by physicians (18.47%) and cleaning assistants (13.85%). According to the authors, nursing assistants made up the largest group of hospital workers and, due to the characteristics of their activities, were more exposed to injuries with sharp instruments. From all accidents, 36.9% occurred during surgeries and administration of intravenous medication. Clinical and surgical dental procedures and the characteristics of dental instruments expose dentists and dental assistants equally to accidents, as shown in our survey (48.8% in each category).
Data13 from another Brazilian hospital reported 861 accidents from 2000 to 2001. The majority of accidents involved females (75.4%), those aged between 21 to 50 years (92.9%), and those who were married (51%). The age group most involved in the accidents was 31-40 years (39.7%). Despite being from different healthcare areas, similarity can be observed between the data from this study and our data if gender and age were taken into account. Nursing staff (56.2%) was the group that suffered the most injuries, followed by cleaning assistants (20.6%), other categories (administration, laboratory, technical support, and kitchen), and doctors/nurses (2.2%). The authors13 suggest that nursing staff are more representative in number in hospital settings and thus are more susceptible to sharps injuries and deal with more risks procedures during their workday.
Donatelli9 showed that needles were the instrument most frequently connected to accidents (44.6%); the percentage is similar to that of the present study (51.2%) and the study by Callan et al.14 (45%). The last authors collected data over a 2-year period to evaluate the incidence and possible patterns of injury occurring in a North American dental school. Shah et al.10 studied percutaneous injuries among dental professionals and found that most injuries involved a syringe needle (86%).
Blood was present in 72.6% of the accidents reported by Donatelli9 and in 56.3% of the injuries cited by Martins et al.11 In the present study, blood was found in 63.8% of accidents. If the association with blood and saliva is considered, the value rises to 75.6%.
Health-care workers do not al¬ways follow postexposure procedures proposed by operative protocols, as mentioned by Martins et al.14 The authors reported that 52.4% of injured workers allegedly ignored them. Oliveira et al.15 reported that 63.3% of the analyzed workers did not seek medical support and follow-up. Compared with these studies, the present study found a lower percentage (12.2%) of professionals who did not follow the protocols. Nevertheless, it is recommended that every injured employee should follow the post-exposure recommendations.
CONCLUSION
From January 1999 to May 2011, 41 occupational accidents associated with sharp instruments and biological fluids were reported in a dental public health service in Belo Horizonte, Brazil. These incidents could be underreported, considering the time recorded (13 years) and the characteristics of dental instruments.
Despite the literature recommending hepatitis B vaccination, a significant percentage of dental workers did not receive the vaccine. This finding suggests the necessity to improve the knowledge of dental staff on occupational risks and prevention beyond the commitment with standardized prevention procedures.
Quantitative anti-HBs levels were <10 mIU/mL for 24.4% of the injured workers who were allegedly vaccinated. This condition could be explained by misinformation when filling out the accident form or due to failure in the vaccination process. The data emphasize the importance of serologic testing in order to confirm hepatitis B immunization. The results suggest that, due to the high prevalence of blood and needle sticks in the accidents reported, the majority of injured workers received PEP.
The present data emphasize the need for more background on education and training for all dental staff, thus improving their understanding of institutional guidelines and preventing professional risks regarding occupational accidents. Additional research in this field is necessary to record and compare local data, register and analyze the accidents, and identify appropriate public health policies and preventive measures, in order to reduce accidents and review the guidelines.
Collaborators
CD VIEIRA, routing and guidance to professionals uneven, collection of data on file scanning and tabulation of the data, writing the paper, preparation of charts. JI Santos and Cabral MM, care, guidance and referral to injured professionals and writing of the article. JF SILVA, Professional guidance to injured workers collect data on file and writing the article.
REFERENCES
1. Centers for Diseases Control - CDC. Updated U.S. Public health service guidelines for the management of occupational exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR. 2001;50(RR-11):1-42. [ Links ]
2. Centers for Diseases Control - CDC. Exposure to blood: what healthcare personnel need to know. Atlanta: Centers for Diseases Control; 2003 [cited 2008 Feb 11]. Avaible from: <http://www.cdc.gov/HAI/pdfs/bbp/Exp_to_Blood.pdf>.
3. Centers for Diseases Control - CDC. Workbook for designing, implementing, and evaluating a sharps injury prevention program: overview: risks and prevention of sharps injuries in healthcare personnel. Atlanta: Centers for Diseases Control; 2004 [cited 2008 Feb 11]. Available from: <http://www.cdc.gov/
4. Sepkowitz KA, Eisenberg L. Occupational deaths among healthcare workers. Emerg Infect Diseases. 2005;11(7):1003-8. doi: 10.3201/eid1107.041038.
5. Brasil. Lei n. 8.213, de 24 de julho de 1991. Dispõe sobre os Planos de Benefícios da Previdência Social e dá outras providências. Diário Oficial da União, Brasília (DF); 1991 Ago 14 [citado 2008 Feb 11]. Disponível em: <http://www.planalto.gov. br/ccivil_03/leis/l8213cons.htm>.
6. Brasil. Ministério da Previdência Social. Anuário Estatístico (Boletim Estatístico) [cited 2008 Mar 18]. Disponível em: <http:// www.mpas.gov.br>.
7. Minas Gerais (Estado). Polícia Militar de Minas Gerais. Serviço de Arquivo e Estatística Odontológica - SAOE. Relatório bimestral de procedimentos realizados pelo Centro Odontológico da Polícia Militar de Minas Gerais. Belo Horizonte: Polícia Militar de Minas Gerais; 2010.
8. Brasil. Ministério da Saúde. Agência Nacional de Vigilância Sanitária. Serviços Odontológicos: prevenção e controle de riscos. Brasília: Agência Nacional de Vigilância Sanitária; 2006 [citado 2008 Mar 15]. Disponível em: <http://www.anvisa.gov. br/servicosaude/manuais/manual_odonto.pdf>.
9. Donatelli LJ. Acidentes ocupacionais envolvendo exposição a material biológico em profissionais da área odontológica de Bauru [dissertação]. São Paulo: Universidade Estadual Paulista Júlio de Mesquita Filho; 2007.
10. Shah SM, Merchant AT, Dosman, JA. Percutaneous injuries among dental professionals in Washington State. BMC Public Health. 2006; 6:269.
11. Martins AMEBL, Pereira RD, Ferreira, RC. Adesão a protocolo pós-exposição ocupacional de acidentes entre cirurgiões dentistas. Rev Saúde Pública. 2010;44(3):529-40.
12. Amaral SA, Souza AFS, Ribeiro SO, Oliveira MAN. Acidentes com material perfurocortante entre profissionais de saúde em hospital privado de Vitória da Conquista - BA. Sitientibus. 2005;(33):101-14.
13. Ruiz MT, Barboza DB, Soler ZASG. Acidentes de trabalho: um estudo sobre esta ocorrência em um hospital geral. Arq Ciênc Saúde. 2004;11(4):219-24.
14. Callan RS, Caughman F, Budd ML. Injury reports in a Dental School: a two-year overview. J Dent Educ. 2006;70(10):1089- 97.
15. Oliveira AC, Lopes ACS, Paiva MHRS. Acidentes ocupacionais por exposição a material biológico entre a equipe multiprofissional do atendimento pré-hospitalar. Rev Esc Enferm USP. 2009; 43(3):677-83.
 Endereço para correspondência:
Endereço para correspondência:
CD VIEIRA
e-mail: cristinadvieira@ig.com.br
Received on: 2/8/2011
Final version resubmitted on: 2/8/2011
Approved on: 7/12/2012













