Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.61 no.4 Porto Alegre Out./Dez. 2013
CLÍNICO / CLINICAL
Oral health status and bariatric surgery
Estado de saúde oral e cirurgia bariátrica
Juliana Sedrez Reis PATIÑOI; Emilia Addison Machado MOREIRAII; Fernanda BOESINGII; Erasmo Benício Santos de Moraes TRINDADEII
I Universidade Federal de Santa Catarina, Programa de Pós-Graduação em Odontologia. Florianópolis, SC, Brasil.
II Universidade Federal de Santa Catarina, Centro de Ciências da Saúde, Departamento de Nutrição. Campus Universitário, Trindade, 88040-970, Florianópolis, SC, Brasil.
ABSTRACT
Obesity is considered to be a chronic disease associated with early medical complications including: respiratory, cardiovascular, metabolic, psychological and social changes. Over recent decades, there has been a marked increase in the incidence of obesity among the population. Obesity has significant metabolic and systemic immune and inflammatory effects. Bariatric surgery has emerged as a treatment for morbid obesity. Oral changes following bariatric surgery were determined. One man and one woman, with initial Body Mass Indexes of 53-34 and 42-26 kg/m2 respectively, were followed for two years after undergoing Fobi Capella surgery. Dietary complications (frequent vomiting), nutrient deficiencies (iron, vitamin B12, calcium, folic acid and zinc) and xerostomia, sensitivity, and periodontitis were seen in both cases. Demineralization and infiltration of fillings evolved into erosion and an endodontic lesion (case 1) and mobility with consequent tooth loss (case 2). Problems with gingival bleeding, dental caries and dental mobility are directly related to compromising the absorptive area and/or the dietary behaviour of the individual after carrying out bariatric surgery.
Indexing terms: Bariatric surgery. Dental caries. Obesity. Tooth erosion.
RESUMO
A obesidade é considerada uma doença crônica associada a complicações médicas precoces como: alterações respiratórias, cardiovasculares, metabólicas, psíquicas e sociais. Nas últimas décadas, a obesidade tem apresentado um aumento considerável da sua incidência na população. A obesidade apresenta efeitos metabólicos e imunológicos e inflamatórios sistêmicos significativos. A cirurgia bariátrica tem sido visto como um tratamento para obesidade mórbida. Alterações bucais após cirurgia bariátrica foram avaliados. Um homem e uma mulher, com Índices de Massa Corporal iniciais de 53-34 e 42-26 kg/m2, respectivamente, foram acompanhados por dois anos após ser submetidos à cirurgia Fobi Capella. Seqüelas alimentares (vômito freqüente), deficiências de nutrientes (ferro, vitamina B12, cálcio, ácido fólico e zinco) e xerostomia, sensibilidade, e periodontite foram observados em ambos os casos. Desmineralização e infiltração de restaurações evoluíram para erosão e uma lesão endodôntico (caso 1), e mobilidade com conseqüente perda de dentes (caso 2). Problemas com sangramento gengival, cárie e mobilidade dentária são relacionados diretamente a uma diminuição na área para absorção e/ou o comportamento alimentar do indivíduo após cirurgia bariátrica.
Termos de indexação: Cirurgia bariátrica. Cárie dentária. Obesidade. Erosão dentária.
INTRODUCTION
Obesity has significant metabolic and systemic immune and inflammatory effects, which also may increase the host’s susceptibility to periodontal disease1. After bariatric surgery (Roux-en-Y), patients become vulnerable to decreased secretion of gastric acid, achlorhydria and malabsorption of proteins, iron, vitamin B12 and folic acid2. In addition, there are changes in the composition and production rate of the saliva, which has a low buffering capacity, and these changes can in turn affect the neutralization of acids, thereby contributing to the installation of processes of demineralization of the dental enamel in the form of dental caries and dental erosion3. The aim of this work was to determine oral changes following bariatric surgery.
CASE REPORTS
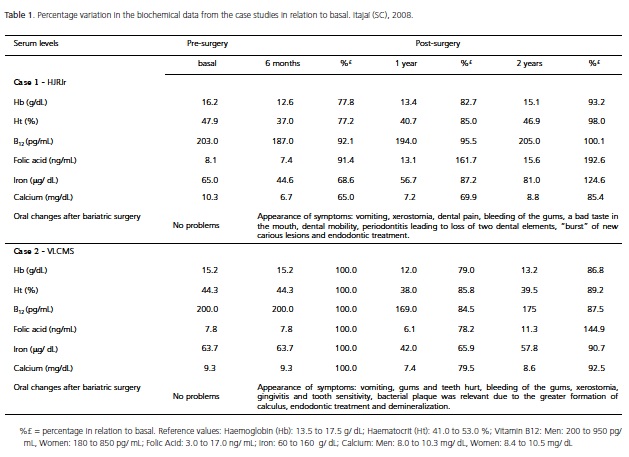
We analysed the cases of two patients, submitted to Roux-en-Y gastric bypass bariatric surgery (BS). Nutritional diagnosis was performed through the Body Mass Index (BMI)4. The haemogram blood analysis (haemoglobin and haematocrit) was carried out by a morphological examination. Vitamin B12 and folic acid were determined in the serum using a kit from Diagnostic Products Corporation (Los Angeles, California, USA). Iron was determined using a kit from Merck (São Paulo, Brazil), and an Ecoline E (Merck, São Paulo, Brazil) kit was used to measure calcium. Oral health was assessed according to the criteria of the World Health Organisation (WHO)5. The research protocol followed the guidelines of the World Medical Association and was approved by the Committee for Ethics in Research of the Universidade Federal de Santa Catarina. It was obtained the approval from patients and the signature of the Informed Consent Term.
CASE 1
HJRJr, a 29 year-old male white lawyer with a BMI of 53 kg/ m2. The incidence of caries in the patient was under control, and he undertook prophylaxis including the application of fluoride. There were no gingival problems. After surgery he complained that "my gums bleed easily, my teeth feel loose and some of them are painful" (sic). During the first fifteen days the diet was of a liquid consistency with no residue, evolving to a thick liquid. Solid food was begun after 45 days and during this adaptation phase the patient presented frequent vomiting when the size and volume of foods ingested exceeded those recommended (250 ml or g/ per meal/ every three hours). Medical visits during the first year occurred on a bi-monthly basis, and in the second year after surgery they were quarterly. Laboratory examinations at 6 months post-surgery revealed a deficiency in haematocrit, vitamin B12, serum iron and calcium even with the use of the Materna multivitamin (Wyeth, Itapevi, Brazil) from 15 days after surgery (Table 1). The first symptom reported by the patient was xerostomia. Four months after surgery, the patient sought dental treatment complaining of pain, bleeding of the gums, a bad taste in the mouth and dental mobility. The gingivitis rapidly evolved into periodontitis leading to mobility and consequently the loss of two dental elements. Despite the patient avoiding any kind of sugar, there was a "burst" of new carious lesions. The patient is undergoing periodontal treatment and the necessary extractions and fillings have been performed. In relation to the pain, infiltration of the fillings present was observed and the secondary caries evolved rapidly, causing widespread destruction of dental tissues requiring endodontic treatment in a dental element. At present the patient has a BMI of 34.25 kg/ m2 (Table 1).
CASE 2
VLCMS, a 42 year-old female white university lecturer with a BMI of 42 kg/ m2. The patient had no major problems concerning her oral cavity, and had a check-up every 6 months for the removal of calculus in the lingual region of the lower incisors and prophylaxis. After BS she complained that "my gums and teeth hurt. When I brush my gums bleed easily" (sic). With the objective of inhibiting frequent episodes of vomiting the patient was prescribed an antiemetic (Plasil, Sanofi Aventis, São Paulo, Brazil). Approximately one month after BS the patient began to eat solid food. During this adaptation phase she presented with approximately weekly vomiting for three months, despite continuing to take the antiemetic. During the first year, the patient received nutritional guidance every two months, changing to quarterly visits in the second year, and today she receives twice-yearly visits. One year after surgery there was a deficiency in haematocrit, serum iron and vitamin B12 (Table 1), even with the prescription of a vitamin supplement (Centrum®, Wyeth, Itapevi, Brazil). The first symptom reported by the patient concerning the oral cavity, soon after BS, was xerostomia. After two months the patient sought dental treatment complaining of pain and gingival bleeding, with a diagnosis of gingivitis and sensitivity in dental elements. The speed of formation and the increase in bacterial plaque were relevant due to the greater formation of calculus; even though the patient had an excellent oral hygiene routine, she was unable to remove the plaque. As a result several surgical interventions were necessary for the removal of dental calculus in the patient, who until then had only required preventive examinations. In spite of the resources employed, areas of infiltration were identified (secondary caries) in the majority of fillings, making endodontic treatment necessary in some dental elements. In the upper front elements small areas of demineralization were detected that had evolved and been characterised as erosion lesions, one year after BS. Today
DISCUSSION
The cases presented here confirm some of the consequences expected after bariatric surgery (BS). These findings are similar to those reported by Vargas-Ruiz et al.6 who found that even routine vitamin and mineral supplementation was not sufficient to prevent these deficiencies. A relevant finding identified in reviews of the literature is that vitamin deficiency may be found in overweight and obese individuals due to an unbalanced dietary intake or even as a result of a reduction in the bioavailability of micronutrients in these patients7-8. In relation to the consequences of BS for the oral health status of patients the "dry-mouth sensation" reported by them is worrying with regard to the quantity of saliva that is being produced by the salivary glands, since patients who exhibit a low salivary flow tend to present with more severe carious lesions9.
Greabu et al.10 have proposed that the saliva should be considered the first line of defence of the organism against oxidative stress and aggressive insults to the oral tissues. The saliva also has a significant influence on the processes of demineralization and remineralization with the participation of calcium, although the availability of the latter can be affected after gastric bypass due to a limitation in the area for absorption. In addition, the demineralization of the dental enamel can occur through the actions of bacterial (dental caries) or non-bacterial acids (dental erosion). In both cases presented here the patients showed the presence of dental caries. The episodes of vomiting and the nutritional deficiencies observed in both cases during the first year after BS may explain the occurrence of caries and gingivitis in these patients due to a change in the oral microbiota and pH.
Restorative dental intervention in the patients is still in progress. However, what the patient needs most is care and guidance, since it is uncertain for how long or how frequently the patient will present with episodes of vomiting.
CONCLUSION
In conclusion, this study identified oral problems (gingival bleeding, dental caries and dental mobility) that may result from a deficiency of nutrients after undergoing bariatric surgery.
Acknowledgements
EAMM is a recipient of a Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) fellowship.
Collaborators
JSR PATIÑO and EAM MOREIRA, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: JSR PATIÑO, EAM MOREIRA, EBSM TRINDADE Acquisition of data: JSR PATIÑO. Analysis and interpretation of data: JSR PATIÑO, F BOESING. Drafting of the manuscript: EAM MOREIRA, JSR PATIÑO, F BOESING and EBSM TRINDADE. Critical revision of the manuscript for important intellectual content: EAM Moreira, EBSM TRINDADE. Statistical analysis: F BOESING, EAM Moreira. Final approval of the version to be submitted: EAM MOREIRA, EBSM TRINDADE.
REFERENCES
1. Ritchie CS, Kinane DF. Nutrition, inflammation, and periodontal disease. Nutrition. 2003;19(5):475-6. doi: 10.1016/S0899- 9007(02)01043-2. [ Links ]
2. Parkes E. Nutritional management of patients after bariatric surgery. Am J Med Sci. 2006;331(4):207-13.
3. Touger-Decker R, Mobley CC, American Dietetic Association. Position of the American Dietetic Association: oral health and nutrition. J Am Diet Assoc. 2007;103(5):615-25. doi: 10.1053/ jada.2003.50130.
4. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity. Geneva: World Health Organization; 1998.
5. World Health Organization. Oral health surveys: basic methods. 4th ed. Geneva: World Health Organization; 1997.
6. Vargas-Ruiz AG, Hernández-Rivera G, Herrera MF. Prevalence of iron, folate, and vitamin B12 deficiency anemia after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2008;18(3):288-93. doi: 10.1007/s11695-007-9310-0.
7. Kaidar-Person O, Person B, Szomstein S, Rosenthal RJ. Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part A: vitamins. Obes Surg. 2008;18(7):870-6. doi: 10.1007/s11695-007-9349-y.
8. Kaidar-Person O, Person B, Szomstein S, Rosenthal RJ. Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part B: minerals. Obes Surg. 2008;18(8):1028- 34. doi: 10.1007/s11695-007-9350-5.
9. Hague AL, Baechle M. Advanced caries in a patient with a history of bariatric surgery. J Dent Hyg. 2008;82(2):22.
10. Greabu M, Battino M, Mohora M. Could saliva constitute the first line of defence against oxidative stress? Rom J Intern Med. 2007;45(2):209-13.
 Endereço para correspondência:
Endereço para correspondência:
EAM MOREIRA
e-mail: emilia.moreira@ufsc.br
Received on: 26/5/2010
Final version resubmitted on: 7/6/2010
Approved on: 26/11/2010













