Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.62 no.3 Porto Alegre Out./Dez. 2014
ORIGINAL / ORIGINAL
Efficacy of casein derivate CPP-ACPI
Eficácia clínica do complexo de caseína CPP-ACPI
Renata Faria PEREIRAI; Soraya Coelho LEALII
I Artigo elaborado a partir da dissertação de PEREIRA RF, intitulada "O papel do CPP-ACP no processo de remineralização dentária"; 2012; Universidade de Brasília
II Universidade de Brasília, Faculdade de Ciências da Saúde, Departamento de Odontologia. Campus Darcy Ribeiro, Asa Norte, 70910-500, Brasília, DF. Brasil
ABSTRACT
Objective
A literature review of systematic reviews and in situ and in vivo randomized controlled trials was conducted in order to assess the role of casein phosphopeptide - amorphous calcium phosphate in providing caries-preventive effect superior to any intervention or placebo.
Methods
Initially, Pubmed database was searched for systematic reviews. Two systematic reviews were identified, which concluded that the quantity and quality of randomized controlled trials were insufficient to recommend the clinical use of the product. After this, Pubmed database was searched for in situ and in vivo randomized controlled trials that were not included in the reviews identified. In vivo and in situ studies yielded mixed results.
Results
In situ studies indicated greater efficacy of casein phosphopeptide - amorphous calcium phosphate in comparison with placebo. Whereas, in vivo studies demonstrated different findings.
Conclusion
Casein phosphopeptide - amorphous calcium phosphate had a performance equivalent to or greater efficacy than placebo; fluoride was more effective than the casein complex; casein phosphopeptide - amorphous calcium phosphate associated with fluoride showed better or equivalent performance to that of placebo. In view of available evidence, it was not possible to generalize the indication of casein phosphopeptide - amorphous calcium phosphate for preventing dental caries. Further studies on the preventive effect and longer treatment applications are recommended.
Indexing terms: Phosphopeptides. Sodium fluoride. Tooth remineralization.
RESUMO
Objetivo
Foi conduzida revisão da literatura em busca de ensaios clínicos randomizados in situ e in vivo que avaliassem o papel do complexo de fosfopeptídeo de caseína - fosfato de cálcio amorfo na prevenção de lesões de cárie.
Métodos
Inicialmente, buscou-se identificar na base Pubmed revisões sistemáticas sobre o tema. Foram identificadas duas revisões sistemáticas, que concluíram que a quantidade e qualidade dos ensaios clínicos randomizados são insuficientes para recomendação do uso clínico do produto. Posteriormente, pesquisaram-se ensaios clínicos randomizados in situ e in vivo que não tivessem sido incluídos nas revisões identificadas.
Resultados
Os estudos in vivo e in situ tiveram resultados contraditórios. Os estudos in situ indicaram uma maior eficácia do complexo de fosfopeptídeo de caseína - fosfato de cálcio amorfo em relação ao placebo. Já os estudos in vivo demonstraram diferentes.
Conclusão
Complexo de fosfopeptídeo de caseína - fosfato de cálcio amorfo apresentou desempenho ora superior, ora equivalente ao placebo; o flúor demonstrou maior eficácia que o complexo de caseína; o complexo de fosfopeptídeo de caseína - fosfato de cálcio amorfo associado ao flúor se mostrou ora melhor, ora equivalente ao placebo. Diante da evidência científica disponível, não se pode generalizar a indicação do complexo de fosfopeptídeo de caseína - fosfato de cálcio amorfo para prevenção de lesões cariosas.
Termos de indexação: Fosfopeptídeo. Fluoreto de sódio. Remineralização dentária.
INTRODUCTION
Caries: processes of dental remineralization and demineralization
According to the World Health Organization (WHO), in 2003, caries diseases was the major public health problems in the majority of industrialized countries. It affects 60 to 90% of children of school-going age, and the large majority of adults1.
Caries is known to be a multifactorial disease. The development of caries lesions depends on interaction between the tooth structure, cariogenic microorganisms (particularly Streptococcus mutans,) and presence of fermentable carbohydrates. Therefore, preventive and therapeutic approach must consider the set of these factors.
Cariogenic microorganisms colonize the tooth surface and form dental biofilm. In physiologic conditions, the oral fluids (saliva and biofilm) present a higher concentration of calcium (Ca) and phosphate (P) in the medium outside of the tooth (supersaturation) than in hydroxyapatite (HA), which is the primary constituent of the enamel structure (crystallized form of calcium phosphate). These ions are continually deposited on the tooth surfaces and in areas in which demineralization processes occur. This process is known as the "natural defense phenomenon" promoted by saliva to promote the mineral preservation of tooth enamel2.
The loss (demineralization) and gain (remineralization) of minerals on the enamel surface is a dynamic physical-chemical process, which occurs when the bacteria present in dental biofilm are exposed to a diet composed of fermentable carbohydrates, particularly sucrose. Whenever sugar penetrates into cariogenic biofilm, it is converted into acid and the biofilm fluid becomes saturated in comparison with the mineral component of enamel. In this situation, pH has a low critical value, at which demineralization of enamel occurs. However, after a certain period, the physiological value of pH is restored when sugar consumption ceases, and the conditions of supersaturation are re-established. At this time,, reposition of a certain quantity of lost mineral occurs, in a process denominated dental remineralization. This reposition of lost mineral occurs by means of Ca and P ions present in biofilm fluid and saliva, right after dental biofilm removal by brushing. The quantity of Ca and P replaced is lower than the amount lost, so that small mineral losses occur2.
If the factors responsible for disease (biofilm and frequent exposure to sugar) are not controlled, with the passage of time, mineral loss cannot be impeded. Therefore, events of mineral dissolution will repeatedly occur, and may lead to a degree of demineralization greater than that of the remineralizing capacity of the oral fluids. Therefore, an imbalance in these processes of demineralization and remineralization may result in small mineral losses, only observed by electronic or optical microscopy; mineral losses observed clinically (white spots), up to the formation of cavities on the tooth surface, in which it will be necessary to perform invasive interventions. Moreover, it is important to point out that caries disease progresses in a different manner among individuals, as it is a disease in which individual susceptibility is also an important factor for its progression.
Fluoride
At present, it is known that the action of fluoride (F) in interfering in the profess of caries lesion formation is not systemic, but local. For this purpose, fluoride must be present in the biofilm and saliva at the time in which the biofilm is exposed to sugar, or after its removal during tooth brushing2.
It is noted that fluoride, even in low concentrations, interferes in the process of caries development. Hydroxyapatite (HA) dissolves at a pH of around 5.5, while fluorapatite (FA: crystallized form of F, Ca and P) dissolve at a pH close to 4.5. When the oral pH remains between 4.5 and 5.5, the process of HA demineralization occurs, in which there is release of Ca, P and hydroxyls in the oral environment. If there is fluoride present, these ions react with it and fluorapatite is formed which, saturated at this pH, is deposited on the tooth surface. This compensates the mineral loss occurring at pH between 4.5 and 5.53. However, this mineral reposition occurring by means of fluorapatite formation is not considered remineralization, in fact. but rather as an inhibition of demineralization, because the mineral component deposited differs from the one lost. Furthermore, fluorapatite is deposited on the tooth surface, while the Ha is dissolved in the subsuperficial region of the tooth2.
As previously stated, caries is essentially a disease related to tooth demineralization. A considerable body of literature has established the use of fluoride as being an important agent in dental remineralization. The interaction between the ions of Ca and fluoride, which form fluorapatite, is greater between the ions of Ca and OH, which forms HA. This gives fluorapatite greater stability and lower solubility. Therefore, fluoride is the main component of dentifrices and mouth washes4.
The indirect effect of fluoride on the reduction of dental demineralization, when pH falls, is complemented by the natural effect of fluoride on dental remineralization, when the pH rises, promoting the reposition of Ca and P ions present in biofilm fluid. If the demineralized surface is submitted to tooth brushing, the saliva is capable of promoting remineralization. However, if there is presence of fluoride, this process is potentiated2.
Dentifrices and fluoridated oral solutions have been demonstrated to diminish the activity of caries in controlled randomized clinical trials. The efficacy of these products arises from their ability to incorporate fluoride ions in the plaque and tooth enamel5. However, the toxicological potential of fluoridated compounds must be pointed out. There is risk of acute intoxication occurring when a large quantity of fluoride is ingested. There may also be chronic intoxication when there is consumption of a concentration of fluoride in excess of the adequate amount for a longer period of time.
METHODS
In view of the cariogenic challenges to which dental structures are usually submitted, one notes that there has been an endeavor to develop methods for the diagnosis of caries lesions in the initial stages, in order to prevent their progression, and consequently, the need for restorative intervention. In addition, different preventive therapies have been studied, with the potential to increase the degree of remineralization, reduce the process of demineralization and therefore, promote reduction in the incidence of active caries lesions6.
Recently, many studies have centered their evaluations on the concentration of Ca and P present in the teeth. These ions are the main dental components and are intimately related to the process of demineralization. Therefore, many efforts have been concentrated on analysis of the deposition of these minerals on the dental structure, and on agents that may promote the availability of these ions in the oral environment6.
There have been demonstrations that the complex of casein phosphopetide (CPP) - amorphous calcium phosphate (ACP) has an anticariogenic activity in laboratory experiments in animals and humans. The potential of CPP-ACP to inhibit demineralization and to stimulate remineralization is based on the ability of CPP to stabilize ACP, and later formation of CPP-ACP. This complex acts as a reservoir of Ca and P that bonds to the plaque and tooth surface. In the face of an acid medium CPP-ACP releases Ca and P ions, so that mineral supersaturation is maintained in the environment outside of the tooth, and consequently, reduction in the demineralization process and stimulation of remineralization is achieved7-8.
Furthermore, the nanocomplex of CPP-ACP has been shown to have a synergic effect on fluoridated compounds. This synergic effect must be attributed to the formation of nano-agglomerates of Ca, F and P ions (CPP-ACP/F), which results in greater incorporation of fluoride ions into plaque, together with the increase in the concentration of bioavailable Ca and P ions5.
The intervention based on CPP-ACP most commonly used in in vivo studies occurs by means of chewing gums. Other CPP-ACP vehicles include mouth washes and topical cream, denominated Tooth MousseTM (Europe and Australia) or MI PasteTM (United States of America and Japan).
METHODS
The review of the literature was conducted with the aim of verifying the clinical efficacy of CPP-ACP in inhibiting the formation of caries lesions.
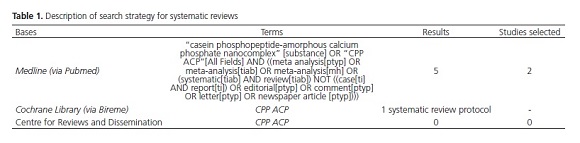
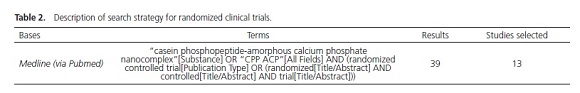
Initially, a search was conducted in the electronic databases of Pubmed, The Cochrane Library and Centre for Reviews and Dissemination (CRD) for systematic reviews (SR), with or without meta-analyses, which evaluated the efficacy of CPP-ACP (Table 1).
In addition, as the articles published in the year 2012 were still in the process of indexation by Pubmed, a more sensitive search was conducted by means of using the terms "casein phosphopeptide-amorphous calcium phosphate nanocomplex"[Substance] OR "CPP ACP"[All Fields], for the year 2012. Nine publications were found, and 2 in situ20 study was selected, in accordance with the above-mentioned inclusion criteria.
RESULTS
Systematic reviews
Initially, 2 systematic reviews were identified. The first of these, conducted by Azarpazhooh et al.7, reunited randomized and quasi randomized clinical studies, published up to October 2007, which tested the efficacy of casein derivatives (among them CPP-ACP) in the diverse forms of dental application. In this review, 12 studies were selected, which tested the efficacy of casein derivatives in dental clinical practice. These studies were selected by means of the inclusion criterion, and measurement of the force and quality of the studies, in accordance with the System of Classification of Evidence, developed by the Canadian Task Force for preventive treatments. The outcomes of interest were as follows: prevention of caries (10 studies), treatment of dentinal hypersensitivity (1 study) and treatment of xerostomia (1 study).
Of the ten studies that had prevention of caries as the outcome, eight were in situ and two were in vivo studies. Among the latter studies mentioned, one of them were related to the regression of white spot lesion9. The other in vivo study evaluated the regression or progression or root caries lesions with the use of a mouth wash solution based on casein derivatives associated with calcium phosphate (CDCP), in comparison with the use of a fluoride-based solution, in individuals with salivary gland dysfunctions10 (Table 3).
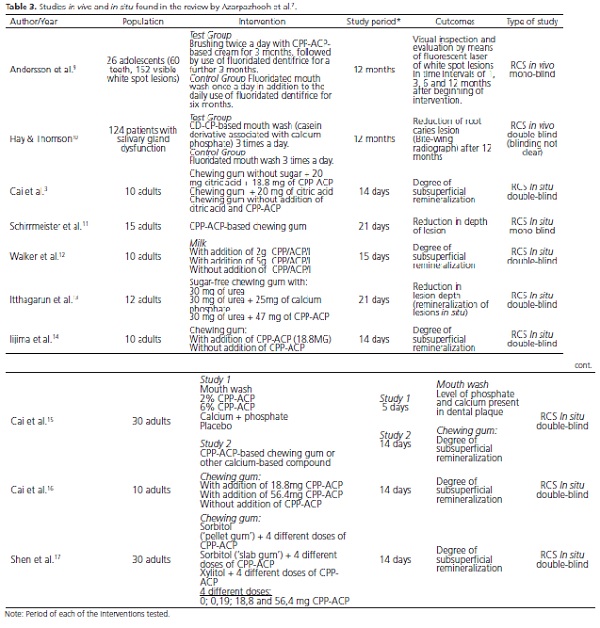
With regard to in situ studies, the patients used an acrylic device that covered the palate from the first premolar to the last tooth in the dental arch, into which fragments of human teeth were fitted, which had demineralized subsuperficial lesions, in 7 of the 8 in situ studies identified. Only in the study of Schirrmeister et al.11 was a fragment of bovine tooth used in the acrylic devices fitted to the mandible.
With regard to the conclusions of these studies, only the study of Schirrmeister et al.11 did not observe a higher rate of demineralization in the subsuperficial lesions evaluated. All the other seven in situ studies observed a significant increase in the degree of remineralization of the lesions treated with casein compounds.
Only one in vivo9 study was identified, which tested the efficacy of CPP-ACP compounds in the process of caries lesions, in comparison with fluoridated compounds. Visual inspection and evaluation by means of fluorescent laser were performed in time intervals of 1, 3, 6 and 12 months after beginning of intervention. There was only statistical significance that benefitted CPP-ACP (63%) in the reduction of white spots in comparison with fluoridated compounds (25%) in the evaluation that used visual inspection performed 12 months after the beginning of treatment. Whereas, the method that used fluorescent laser was not capable of identifying any difference between the treatments9.
The review of Azarpazhooh et al.7 concluded that the quality and quantity of articles reviewed were insufficient to generate conclusive evidence of the long term effectiveness of casein derivative compounds, especially CPP-ACP.
The other review found was associated with a metaanalysis. In this study, Yengopal & Mickenautsch8 included clinical studies (in situ and in vivo) and systematic reviews, published up to August 2008, which evaluated the efficacy of CPP-ACP-based compounds. In order to be selected, the studies needed to make information available with respect to sample size, loss of follow-up of patients and about the follow-up period of the study. Eleven studies and one systematic review6 were selected. All of the 11 studies selected presented Score A, on a scale of evaluation, with regard to randomization, confidentiality in allocation and blinding. Only two studies presented Score B for the parameter confidentiality in allocation. Of these 11 studies, 5 participated in the metaanalysis, as they were the only one with characteristics that allowed statistical analysis of their results in conjunction; that is, they were clinically and methodologically homogeneous, and presented similar outcomes.
All of the five3,14,16-18studies included in the metaanalysis were of the in situ type, with a short duration of follow-up (7 to 21 days), and the intervention used was chewing gum containing CPP-ACP. The result of this analysis showed higher rates of tooth remineralization in favor of the use of CPP-ACP-based chewing gums, in comparison with the use of chewing gum without the addition of CPP-ACP, or in comparison with no intervention. Among the other 6 studies not included in the meta-analysis, 412-13,15 were in situ studies, and all of them showed a higher rate of remineralization with the use of CPP-ACP. However, it is worth emphasizing that one of these studies4 compared CPP-ACP added to fluoride in comparison with CPP-ACP alone and with fluoride alone, As a result, CPP-ACP associated with fluoride was observed to be the intervention that showed the best performance, while the intervention based on CPP-ACP only had a similar performance to that of fluoride alone.
The other two studies not included in the metaanalysis were in vivo. One of them was the study that was included in the systematic review of Azarpazhooh et al.7, which was that of Anderson et al.,9. The other study refers to that of Morgan et al.19, in which 2,720 children used chewing gum with or without the addition of CPPACP. The follow-up period of the study was 24 months, and regression of caries lesions was observed by means of bite-wing radiographs that allowed visualization of the interproximal dental regions.
It was observed that of the ninein situ studies found in the review of Yengopal & Mickenautsch8, seven studies3,12,17 coincided with those already selected by the review of Azarpazhooh et al.7; the other two studies found only in the more recent review were published after the period of search conducted by Azarpazhooh et al.7. As follows below, there is information about these two new in situ studies and the new in vivo study found by Yengopal & Mickenautsch8 (Table 4).
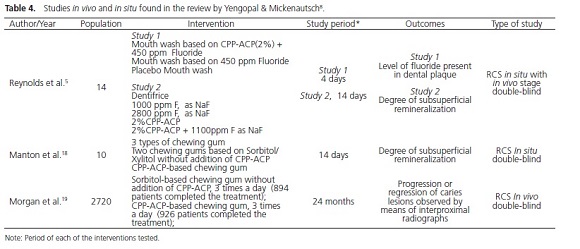
Yengopal & Mickenautsch8 observed that in spite of the meta-analysis having been conducted only for in situ studies that presented a short period of exposure to this complex, the promising results of the in vivo studies, one of them with a large sample size19 and both9,19 with a longer time of exposure to the CPP-ACP complex (12 to 24 months), suggested the remineralizing effect of the CPP-ACP complex, in studies with long follow-up periods. It is suggested that further randomized in vivo studies, with adequate methodology and longer followup periods should be conducted.
Studies in vitro and in vivo
In addition to the systematic reviews cited, as mentioned in the item Methodology, a new search was conducted in the Pubmed database in May 2012, in order to identify in situ and in vivo randomized clinical trials that evaluated the remineralizing potential of CPP-ACP, published after the search conducted by the last systematic review published about the subject (after the month of August 2008). Six in situ and 7 in vivo studies were identified (Table 5)
With regard to the conclusion of the 6 in situ studies, all of them showed a higher rate of remineralization with the use of CPP-ACP alone or associated with F. However, it is important to point tout that four of these studies compared CPP-ACP with a placebo, while two studies21,23 compared interventions of CPP-ACP associated with fluoride, in comparison with CPP-ACP alone. In only one of them21 was the comparison with fluoride alone, the results of which demonstrated that the intervention based on CPP-ACP associated with fluoride was the one that obtained the best results, followed by CPP-ACP alone, which in turn showed a better performance than that of fluoride alone.
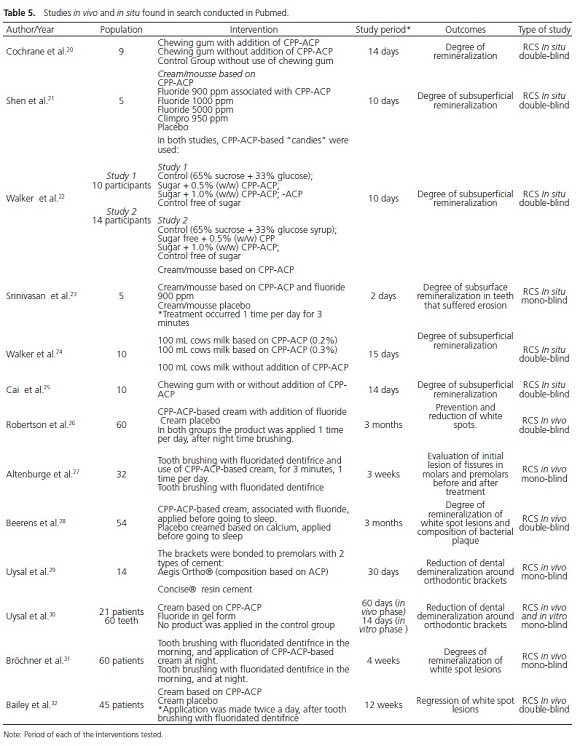
Among the 7 in vivo studies, 2 of them26,28 evaluated the use of CPP-ACP associated with fluoride, which was shown to be more effective than the placebo in only one of the studies26. In the study of Beerens et al.28 there was no significant difference between the interventions.
Of the other 5 in vivo articles27,29-32, in only one of them30 was an intervention used in comparison with one based on F, which was shown to be as effective as CPP- ACP. Among the four remaining studies, in which the placebo was used for comparison, in three of these27,29,32 CPP-ACP demonstrated a higher remineralization potential. However, in one of these studies27 the greater efficacy of CPP-ACP was observed only when some evaluations were made by means of fluorescent laser. Nevertheless, there was no significant difference between the treatments when visual evaluation was made. In the remaining study31, CPPACP showed the same performance as the placebo.
DISCUSSION
The process of enamel remineralization has been studied for over 100 years. It has been suggested that non invasive treatment of initial caries lesions occurring by means of processes that stimulate remineralization, has been one of the major advances in control of the disease.
Therefore, the appearance of products that have the potential to promote dental remineralization are welcome, however, they need to be evaluated with caution, by means of analysis of the best scientific evidence available.
CPP-ACP has been extensively studied recently. In order to better evaluate its remineralizing potential, this literature review was conducted with the goal of seeking clinical results of the efficacy of this complex in the prevention of caries lesion formation.
Both meta-analyses identified, suggested that further in vivo studies with long follow-up periods should be conducted in order to reduce the uncertainty about the clinical efficacy of CPP-ACP, particularly in comparison with fluoridated compounds.
As regards the in situ studies found, CPP-ACC demonstrated greater efficacy than the placebo in the majority of publications. The greater efficacy of CP-ACP associated with fluoride in comparison with CPP-ACP alone was also demonstrated. In only one study was the superiority of the casein complex verified in comparison with fluoride, considered the standard therapy in the process of dental remineralization.
Whereas, with reference to the in vivo studies, findings with a higher level of scientific evidence, the results were contradictory: CPP-ACP associated with fluoride was at times shown to be more effective, and at times was shown to be similar to the placebo. CPP-ACP alone at times demonstrated greater efficacy, at time demonstrated similarity to placebo, and when compared with F, obtained an equivalent performance.
In view of the data presented, up to the moment, it has not been conclusively demonstrated that CPP-ACP (alone or in association with fluoride) has advantages in comparison with fluoride in the promotion of dental remineralization. Indeed, there are also data that demonstrate clinical similarity of the casein complex in comparison with the placebo.
Moreover, the posology of CPP-ACP was noted to be variable. The best form and frequency of application were not established. This fact strongly influences the comparison of the results found in the studies, which used different polsologies of the product.
In spite of the majority of studies comparing CPPACP with a placebo, it is very important for the substance used for comparison to be standard therapy, in this case, fluoridated compounds. Because, in spite of noting the appearance of new products with remineralizing potential, it is not always possible to prove clinical advantages of the new in comparison with existent therapies.
CONCLUSION
A cautious approach is needed when making a general recommendation about the use of CPP-ACP in the prevention of caries, considering that there is no uniformity in the results of studies with a higher level of evidence, with respect to the remineralizing role of the casein complex in clinical practice.
It is suggested that the results of further in vivo studies, with long follow-up be awaited, in order to be able to generalize the benefit demonstrated by CPP-ACP in some patients.
Collaborators
RF PEREIRA conducted the bibliographic review for preparing the introductory part, under the supervision of the author SC LEAL. RF PEREIRA and SC LEAL were involved in developing the search strategies, selection of articles and interpretation of their results. Afterwards, discussions were held about the findings, and the article presented was written.
REFERENCES
1. Petersen PE, Lennon MA. Effective use of fluorides for the prevention of dental caries in the 21st century: the WHO approach. Community Dent Oral Epidemiol. 2004;32:319-21 [ Links ]
2. Cury JA, Tenuta LM. Enamel remineralization: controlling the caries disease or treating early caries lesions? Braz Oral Res. 2009;23(Suppl 1):23-30. doi: 10.1590/S1806- 83242009000500005
3. Burt BA. The changing patterns of systemic fluoride intake. J Dent Res. 1992 71:1228-37. doi: 10.1177/00220345920710051601
4. Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, et al. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2008;87(4):344-8. doi: 10.1177/154405910808700420
5. Pulido MT, Wefel JS, Hernandez MM, Denehy GE, Guzman- Armstrong S, Chalmers JM, et al. The inhibitory effect of mi paste, fluoride and a combination of both on the progression of artificial caries-like lesions in enamel. Oper Dent. 2008;33(5):550- 5. doi: 10.2341/07-136.
6. Azarpazhooh A, Limeback H. Clinical efficacy of casein derivatives: a systematic review of the literature. J Am Dent Assoc. 2008;139(7):915-24. doi: 10.14219/jada.archive.2008.0278
7. Yengopal V, Mickenautsch S. Caries preventive effect of casein phosphopeptide-amorphous calcium phosphate (CPP-ACP): a meta-analysis. Acta Odontol Scand. 2009;67(6):1-12. doi: 10.1080/00016350903160563.
8. Andersson A, Sköld-Larsson K, Hallgren A, Petersson LG, Twetman S. Effect of a dental cream containing amorphous creamphosphate complexes on white spot lesion regression assessed by laser fluorescence. Oral Health Prev Dent. 2007;5(3):229-33.
9. Hay KD, Thomson WM. A clinical trial of the anticaries efficacy of casein derivatives complexed with calcium phosphate in patients with salivary gland dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(3):271-5. doi: 10.1067/ moe.2002.120521
10. Cai F, Manton DJ, Shen P, Walker GD, Cross KJ, Yuan Y, et al. Effect of addition of citric acid and casein phosphopeptideamorphous calcium phosphate to a sugar-free chewing gum on enamel remineralization in situ. Caries Res. 2007;41(5):377-83. doi:10.1159/000104796
11. Schirrmeister JF, Seger RK, Altenburger MJ, Lussi A, Hellwig E. Effects of various forms of calcium added to chewing gum on initial enamel carious lesions in situ. Caries Res. 2007;41(2):108- 14. doi:10.1159/000098043
12. Walker G, Cai F, Shen P, Reynolds C, Ward B, Fone C, et al. Increased remineralization of tooth enamel by milk containing added casein phosphopeptide-amorphous calcium phosphate. J Dairy Res. 2006;73(1):74-8.
13. Itthagarun A, King NM, Yiu C, Dawes C. The effect of chewing gums containing calcium phosphates on the remineralization of artificial caries-like lesions in situ. Caries Res. 2005;39(3):251-4. doi: 10.1159/000084806
14. Iijima Y, Cai F, Shen P, Walker G, Reynolds C, Reynolds EC. Acid resistance of enamel subsurface lesions remineralized by a sugar-free chewing gum containing casein phosphopeptideamorphous calcium phosphate. Caries Res. 2004;38(6):551-6. doi: 10.1159/000080585
15. Cai F, Shen P, Morgan MV, Reynolds EC. Retention in plaque and remineralization of enamel lesions by various forms of calcium in a mouthrinse or sugar-free chewing gum. J Dent Res. 2003;82(3):206-11. doi: 10.1177/154405910308200311
16. Cai F, Shen P, Morgan MV, Reynolds EC. Remineralization of enamel subsurface lesions in situ by sugar-free lozenges containing casein phosphopeptide-amorphous calcium phosphate. Aust Dent J. 2003;48(4):240-3. doi: 10.1111/j.1834-7819.2003.tb00037.x
17. Shen P, Cai F, Nowicki A, Vincent J, Reynolds EC. Remineralization of enamel subsurface lesions by sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2001;80(12):2066-70. doi: 10.1177/00220345010800120801
18. Manton DJ, Walker GD, Cai F, Cochrane NJ, Shen P, Reynolds EC. Remineralization of enamel subsurface lesions in situ by the use of three commercially available sugar-free gums. Int J Paediatr Dent. 2008;18(4):284-90. doi: 10.1111/j.1365- 263X.2008.00920.x
19. Morgan MV, Adams GG, Bailey DL, Tsao CE, Fischman SL, Reynolds EC. The anticariogenic effect of sugar-free gum containing CPP-ACP nanocomplexes on approximal caries determined using digital bitewing radiography. Caries Res. 2008;42(3):171-84. doi: 10.1159/000128561
20. Cochrane NJ, Shen P, Byrne SJ, Walker GD, Adams GG, Yuan Y, et al. Remineralisation by chewing sugar-free gums in a randomised, controlled in situ trial including dietary intake and gauze to promote plaque formation. Caries Res. 2012;46(2):147- 55. doi: 10.1159/000337240
21. Shen P, Manton DJ, Cochrane NJ, Walker GD, Yuan Y, Reynolds C, et al. Effect of added calcium phosphate on enamel remineralization by fluoride in a randomized controlled in situ trial. J Dent. 2011;39(7):518-25. doi: 10.1016/j. jdent.2011.05.002
22. Walker GD, Cai F, Shen P, Adams GG, Reynolds C, Reynolds EC. Casein phosphopeptide-amorphous calcium phosphate incorporated into sugar confections inhibits the progression of enamel subsurface lesions in situ. Caries Res. 2010;44(1):33-40. doi: 10.1159/000275572
23. Srinivasan N, Kavitha M, Loganathan SC. Comparison of the remineralization potential of CPP-ACP and CPP-ACP with 900 ppm fluoride on eroded human enamel: An in situ study. Arch Oral Biol. 2010;55(7):541-4. doi: 10.1016/j.archoralbio.2010.05.002
24. Walker GD, Cai F, Shen P, Bailey DL, Yuan Y, Cochrane NJ, et al. Consumption of milk with added casein phosphopeptideamorphous calcium phosphate remineralizes enamel subsurface lesions in situ. Aust Dent J. 2009;54(3):245-9. doi: 10.1111/j.1834-7819.2009.01127.x
25. Cai F, Shen P, Walker GD, Reynolds C, Yuan Y, Reynolds EC. Remineralization of enamel subsurface lesions by chewing gum with added calcium. J Dent. 2009;37(10):763-8. doi: 10.1016/j. jdent.2009.06.003.
26. Robertson MA, Kau CH, English JD, Lee RP, Powers J, Nguyen JT. MI Paste Plus to prevent demineralization in orthodontic patients: a prospective randomized controlled trial. Am J Orthod Dentofacial Orthop. 2011;140(5):660-8. doi: 10.1016/j. ajodo.2010.10.025
27. Altenburger MJ, Gmeiner B, Hellwig E, Wrbas KT, Schirrmeister JF. The evaluation of fluorescence changes after application of casein phosphopeptides (CPP) and amorphous calcium phosphate (ACP) on early carious lesions. Am J Dent. 2010;23(4):188-92.
28. Beerens MW, van der Veen MH, van Beek H, ten Cate JM. Effects of casein hosphopeptide amorphous calcium fluoride phosphate paste on white spot lesions and dental plaque after orthodontic treatment: a 3-month follow-up. Eur J Oral Sci. 2010;118(6):610-7. doi: 10.1111/j.1600-0722.2010.00780.x
29. Uysal T, Amasyali M, Ozcan S, Koyuturk AE, Akyol M, Sagdic D. In vivo effects of amorphous calcium phosphate-containing orthodontic composite on enamel demineralization around orthodontic brackets. Aust Dent J. 2010;55(3):285-91. doi: 10.1111/j.1834-7819.2010.01236.x
30. Uysal T, Amasyali M, Koyuturk AE, Ozcan S. Effects of different topical agents on enamel demineralization around orthodontic brackets: an in vivo and in vitro study. Aust Dent J. 2010;55(3):268-74. doi: 10.1111/j.1834-7819.2010.01233.x
31. Bröchner A, Christensen C, Kristensen B, Tranæus S, Karlsson L, Sonnesen L, et al. Treatment of post-orthodontic white spot lesions with casein phosphopeptide-stabilised amorphous calcium phosphate. Clin Oral Investig. 2011;15(3):369-73. doi: 10.1007/s00784-010-0401-2
32. Bailey DL, Adams GG, Tsao CE, Hyslop A, Escobar K, Manton DJ, et al. Regression of post-orthodontic lesions by a remineralizing cream. J Dent Res. 2009;88(12):1148-53. doi: 10.1177/0022034509347168.
 Correspondence to:
Correspondence to:
SC LEAL
e-mail: sorayaodt@yahoo.com
Received on: 6/6/2012
Final version resubmitted on: 19/6/2012
Approved on: 19/3/2013













