Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.62 no.4 Porto Alegre Out./Dez. 2014
ORIGINAL / ORIGINAL
Treatment of anterior crossbite and its influence on gingival recession
Pulpotomia em molar decíduo com agregado trióxido mineral
Roberta Nascimento ANDRADEI; Flávia Ribeiro TÔRRESI; Rogério Frederico Alves FERREIRAI; Fernanda CATHARINOII
I Universidade Federal da Bahia, Faculdade de Odontologia, Departamento de Ortodontia. Av. Araújo Pinho, 62, 7º andar, Canela, 40110-150, Salvador, BA, Brasil
II Escola Bahiana de Medicina e Saúde Pública, Curso de Odontologia. Salvador, BA, Brasil
ABSTRACT
Several etiological factors for gingival recession have been discussed in the literature, and the vestibular region of the mandibular incisors is a critical anatomical area for the emergence of this condition. Anterior crossbite is an important factor, because the trauma from occlusion between the incisors generates an imbalance in the distribution of forces, causing changes in the periodontium and making the area more susceptible to mechanical trauma during brushing and to plaque formation. In view of these aspects, the objective of this paper was to demonstrate the influence of early treatment of anterior crossbite on the gingival margin level and risk of gingival recession in the region of the incisors. A case of anterior crossbite treated during the mixed dentition phase was used as an example. After orthodontic therapy with the use of a removable appliance with a finger spring, we noticed improvement in periodontal health and esthetics as the tooth was reattached at its base bone.
Indexing terms: Gingival recession. Malocclusion. Orthodontics. Periodontics.
RESUMO
Diversos medicamentos vêm sendo testados e utilizados na terapia pulpar conservadora de dentes decíduos, no entanto, o formocresol continua sendo o material de escolha nas pulpotomias, mesmo não atendendo às exigências de biocompatibilidade e promovendo a fixação do tecido pulpar vital e não o seu reparo. Com o surgimento do Agregado Trióxido Mineral como um material com propriedades físico-químicas que promovem o reparo tecidual, aliados a outras propriedades importantes, tais como a ação antimicrobiana e a biocompatibilidade aos tecidos pulpares surgiu uma nova alternativa de material na Odontologia. O objetivo deste estudo foi relatar o desempenho do Agregado Trióxido Mineral em uma pulpotomia em molar decíduo e seu acompanhamento por um período de 1 ano. Foi realizada a pulptomia com o uso do MTA no dente 85 de um paciente infantil cujos resultados obtidos foram bastante favoráveis, demonstrando sucesso clínico e radiográfico no período avaliado. Apesar do pouco tempo de acompanhamento do dente decíduo tratado, acredita-se que o MTA possa ter um grande potencial biológico e futuramente podendo transformar-se em uma opção de material para ser utilizado como rotina nas pulpotomias de dentes decíduos.
Termos de indexação: Dente decíduo. Cimentos dentários. Ortodontia. Pulpotomia.
INTRODUCTION
Anterior crossbite is an anterior-posterior malocclusion that is highly prevalent during the mixed dentition and is etiologically associated with a deviation of the eruption axis, causing esthetic, functional, and periodontal abnormalities. Due to its thinner buccal bone plate, the anterior region of the mandible is more susceptible to development of recession, particularly in the presence of occlusal overload due to tooth malposition. Proclination of the mandibular incisors may predispose to dehiscences and fenestrations, with consequent soft tissue injury1.
Gingival recession, a phenomenon that consists of apical migration of the gingival margin2, has several clinical consequences, including esthetic compromise, difficulty maintaining oral hygiene, dentin hypersensitivity, and increased risk of dental caries3. It may be classified into true recession (when there is root exposure) or pseudo-recession (when there is merely a difference in gingival margin level in a tooth in relation to its contralateral partner)4.
To Ustum1, localized gingival lesions may be symptomatic of occlusal trauma, delayed eruption of permanent teeth, and deficient oral hygiene. A form of traumatogenic occlusion may develop when the mandibular incisors erupt into an ectopic position, particularly in the labial direction. In these cases, usually a very narrow band of keratinized mucosa may be present. According to Lindhe et al.5, trauma from occlusion promotes adaptive alterations or changes in the periodontal tissue as a consequence of excessive masticatory forces. This phenomenon may occur in patients with anterior crossbite, which, due to its occurrence in an unfavorable anatomic region, can be a predisposing factor for bone loss and lead to gingival lesions.
Etiologic or predisposing factors for mucogingival problems in the region of the mandibular incisors may be classified as developmental or acquired. Developmental factors include: ectopic eruption; inadequate arch length, leading to crowding and torsiversion; proclination; bone fenestrations; muscle attachments; and abnormal frenal attachment. Among the acquired factors, the most important one is plaque buildup leading to chronic gingivitis. In the presence of malocclusion, these factors cause periodontal changes6.
The combination of deficient oral hygiene and inflammation, compounded by occlusal trauma, may predispose to more rapid development of bone absorption than would occur in the presence of gingival inflammation alone. Therefore, reduction of inflammation and plaque control are essential before, during, and after orthodontic treatment7.
Orthodontic correction may lead to spontaneous improvement of periodontal health, as repositioning of a tooth into its proper alveolar foundation allows better distribution of forces on the long axis, as well as bone remodeling. Eismann & Prusas8 evaluated patients with anterior crossbite and gingival recession, and found an increase in the gingival margin level of the mandibular incisors after 1 year of treatment.
According to Yared et al.3, the pathogenesis of mucogingival defects in proclined mandibular incisors includes the following factors: brushing trauma; thin gingival tissue and underlying alveolar bone; and apical migration of the gingival margin, the location of which is determined by the axial inclination and alignment of the tooth.
A judicious analysis of bone structure and keratinized gingiva width is a critical step of orthodontic treatment planning, particularly when proclination of mandibular incisors will be required. However, some authors claim that recession increases when there is proclination of the lower incisors, even in the presence of adequate keratinized gingiva width9. Conversely, other authors have found no correlation between these variables10.
According to Orrico et al.2, treatment of gingival recession may be curative or preventative. Curative methods are based on mucogingival surgery techniques, whereas preventative measures consist of elimination of etiologic factors by means of bacterial plaque control and orthodontic correction, among others. If gingival recession continues to progress despite conservative methods, surgical treatment may be indicated.
In view of the current literature, the present article seeks to demonstrate, by means of a clinical case report, the influence of dental repositioning on gingival recession by enabling improved distribution of occlusal forces, bone regeneration, and a pleasant gingival esthetic.
CASE REPORT
A 9-year-old girl sought care at Bahiana School of Medicine and Public Health with a chief complaint of unsatisfactory smile esthetics. The patient had good facial harmony, a slightly convex profile, and proportional facial thirds. Intraoral examination revealed crowding of the mandibular incisors; #11 was in crossbite relation to #41 both in centric occlusion and in centric relation, applying an anterior resultant force on the proclined antagonist. These factors, probably compounded by deficient oral hygiene, led to apical migration of the gingival margin of this tooth. In this case, the patient may be classified as having pseudorecession, as there was no root exposure. Nevertheless, pseudo-recession denotes a risk of developing true gingival recession unless causal and predisposing factors are addressed (Figure 1).

Diagnostic procedures (lateral cephalogram, panoramic radiograph, clinical photographs, and plaster study casts) confirmed the clinical examination findings of a harmonious sagittal relationship between the maxilla and mandible, a class I molar relationship, and absence of pathological changes.
Once a diagnosis of anterior crossbite had been confirmed, a treatment plan was developed, which combined orthodontic tooth movement and rigorous biofilm control by means of oral hygiene instructions. The patient was instructed to brush the area of the proclined incisor very carefully, using the modified Bass technique5.
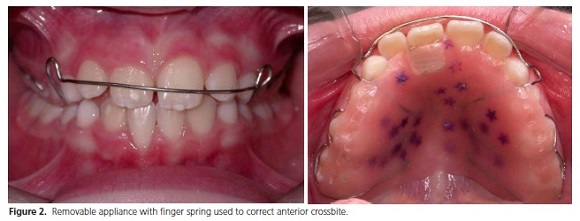
The orthodontic device employed was a removable appliance with a finger spring, activated every 21 days, kept in place for 3 months and removed only for meals. This appliance, which included an occlusal bite guard, served as a bite deprogrammer and prevented occlusal interferences during orthodontic tooth movement (Figure 2).
After correction of malocclusion, the patient's esthetic and periodontal condition improved, with enlargement of the free gingival margin, which suggests that adequate tooth positioning within the socket and the action of masticatory forces on the long axis of the tooth had a favorable effect on regeneration of bone and gingival tissue (Figure 3).
It bears stressing that the patient and her guardian were informed of the benefits and risks of the proposed treatment and provided written informed consent authorizing publication of the images included in this report.

DISCUSSION
Gingival recession occurs mainly in adults. It is relatively common in the mixed dentition and rarely reported in the deciduous phase. The most commonly affected area is that of the mandibular incisors, probably due to the anatomy of the region. Among the various factors predisposing to this condition, anterior crossbite warrants particular consideration, as incorrect dental position can lead to occlusal trauma and consequent periodontal changes.
In the present case, #11 and #41 were in crossbite, which led to proclination of the mandibular incisor. This displacement predisposed the tooth to development and progression of gingival recession as a result of various factors, such as brushing trauma or bone fenestrations and dehiscences.
As it affected an area considered anatomically unfavorable due to limited keratinized gingiva width, this malocclusion probably acted as a predisposing factor for apical migration of the gingival margin of #41. According to Borghetti11, a healthy periodontium with thin gingiva and narrow cortical bone offers little resistance to mechanical or bacterial insults, and is a morphological type that predisposes to recession.
Yared et al.3 believe that, among the various etiologies of gingival recession, marginal gingiva width plays an extremely important role, whereas the keratinized mucosa width is still a source of controversy in the literature. Closs et al.9 found no relationship between these variables: during lingual or labial movement of the crown, the authors observed an increase in gingival width even when little keratinized gingiva was present.
In our patient, correction of crossbite by proper axial repositioning of #11 and correction of the anteriorposterior arch relationship enabled the establishment of a gingival margin level at #41 close to that of the adjacent teeth. Furthermore, vertical alveolar growth in the region of the mandibular incisors also contributed to a more uniform marginal gingiva.
Several studies have pointed out the importance of the relationship between bacterial biofilm and periodontal attachment loss2-3,12-13. Plaque control plays an essential role in preventing gingival inflammation, which could trigger or accelerate progression of gingival recession. As our patient had deficient brushing habits, we provided oral hygiene instructions in an attempt to restore her gingival health.
Brushing instructions were tailored to avoid potential mechanical trauma, particularly to #41, which was in proclination. The constant, low-intensity trauma of brushing against probably thin gingival tissue would have induced chronic inflammation, with consequent tissue responses leading to bone destruction and attachment loss. The use of abrasive toothpastes and hard-bristled brushes should also be avoided.
Conservative treatment of gingival recession consists of eliminating likely etiological factors and controlling plaque by means of proper brushing, and it may stabilize recession14. Surgical treatment consists of gingival grafting, which may be performed before or after orthodontic therapy. Geiger6 noted that preventative surgical treatment of teeth with little attached gingiva or established recession is questionable in many cases, as grafting may prove unnecessary after orthodontic movement or, if still required, may be postponed until orthodontic treatment is complete.
In the case reported herein, the patient wore a removable appliance with finger spring for 3 months to achieve crossbite correction. Proper axial tooth position eliminated any trauma from occlusion and made possible an increase in marginal gingiva at #41, with a pleasant esthetic outcome (Figure 3). Early correction also simplified future treatment, as, according to Proffit15, recurrence of this type of malocclusion is unlikely in the absence of skeletal problems.
CONCLUSION
A combined approach of orthodontic therapy and biofilm control appears to improve the health of periodontal tissue, as the malpositioned tooth is gradually placed into its correct skeletal base, redirecting occlusal forces along its long axis and facilitating proper oral hygiene.
Colaborators
RN ANDRADE, FR TÔRRES, RFA FERREIRA AND F CATHARINO participated in all stages of preparation of the manuscript.
REFERENCES
1. Ustun K, Sari Z,Orucoglu H,Duran I,Hakki SS. Several Gingival recession caused by traumatic occlusion and mucogingival stress: a case report. Eur J Dent. 2008 apr;(2):127-133. [ Links ]
2. Orrico SRP, Cirelli CC, Rosa FP, Bacalhau JT. Recessão gengival na dentição decídua: relato de caso clínico. R Ci Med Biol. 2003 jul/ dez; 2(2):276-82.
3. Yared KFG, Zenobio EG, Pacheco W. A etiologia multifatorial da recessão periodontal. Rev Dental Press Ortodon Ortop Facial. 2006 nov/dez;11(6): 45-51.
4. Stoner JE, Mazdyasna S. Gingival recession in the lower incisor region of 15 year old subjects. J Periodontol. 1980 51(2): 74-76.
5. Lindhe J, Karring T, Lang NP. Tratado de periodontia clínica e implantologia oral. 4a ed. Rio de Janeiro: Guanabara Koogan; 2005.
6. Geiger MA. Mucogingival problems and movement of mandibular incisors: a clinical review. Am J Orthod. 1980 78(5):511-27.
7. Kessler M. Interrelationships between orthodontics and periodontics. Am J Orthod. 1976 70(2): 154-72.
8. Eisman D, Prusas R. Periodontal findings before and after orthodontic therapy in cases of incisor cross-bite. Eur J Orthod. 1990 12(3):281-83.
9. Closs LQ, Branco P, Rizzato SD, Raveli DB, Rösing CK. Gingival margin alterations and the pre-orthodontic treatment amount of keratinized gingiva. Braz Oral Res. 2007 21(1): 58-63.
10. Ruf S, Hansen K, Pancherz H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession? Am J Orthod Dentofacial Orthop. 1998 114(1): 100-6.
11. Borghetti A, Monnet-Corti V. Cirurgia plástica periodontal. Porto Alegre: Artmed; 2002.
12. Kornhauser S, Schwartz Z, Bimstein E. Changes in the gingival structure of maxillary permanent teeth related to the orthodontic correction of simple anterior crossbite. Am J Orthod Dentofacial Orthop. 1996 110(3):263-68.
13. Yared KFG, Zenobio EG, Pacheco W. Projeção ortodôntica de incisivos inferiores: um risco à recessão periodontal? Rev Dental Press Ortodon Ortop Facial. 2006 11(5):35-41.
14. Ottoni J, Magalhães L. Cirurgia plástica periodontal e periimplantar. São Paulo: Artes médicas; 2006.
15. Proffit WR, Fields HWJ, Sarver DM. Ortodontia Contemporânea. In: Proffit WR, Fields HWJ, Sarver DM. Tratamento dos problemas não-esqueléticos em crianças pré-adolescentes. 4a ed. Rio de Janeiro: Elsevier; 2007. p.403-60.
 Correspondence to:
Correspondence to:
F CATHARINO
e-mail: fcmfranco@bahiana.edu.br
Received on: 25/5/2010
Final version resubmitted on: 17/4/2011
Approved on: 28/4/2011













