Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.63 no.1 Porto Alegre Jan./Mar. 2015
REVISÃO / REVIEW
Clinical application of adhesive systems - a critical review: biomimetic approach
Revisão crítica da aplicação clínica dos sistemas adesivos: abordagem biomimética
Weber Adad RICCII; Camila de Paula Telles Pires LUCASII; Ana Cláudia Gabrielli PIVETAII; Maurício Meirelles NAGLEI; Andréia Affonso Barretto MONTANDONI
I Universidade Estadual Paulista Júlio de Mesquita Filho, Faculdade de Odontologia, Departamento de Odontologia Social. Rua Humaitá, 1680, Centro, 14801-903, Araraquara, SP, Brasil
II Universidade Estadual Paulista Júlio de Mesquita Filho, Faculdade de Odontologia. Araraquara, SP, Brasil
ABSTRACT
The various functions and clinical applications of adhesive systems have become a fundamental part of restorative treatment. The biggest challenge for such systems is to provide adequate adhesion to the different tissues, which can be very diverse in nature. When choosing the appropriate adhesive system, the dentist should be familiar with the origin, composition, action mechanism and method of application of each system. The commercially available products and their high technical status have made it possible for the clinician to develop a philosophy of maximum tissue preservation, optimized esthetics, up-to-date concepts and procedures and full function of the restored element, compatible with biomimetic theory. The literature describes the superior qualities of results obtained with three-step total etching adhesives and the use of chlorhexidine as a factor to increase longevity. Future perspectives include the use of ethanol, inactivating agents of enzymes released in the adhesive process and the action of agents that act upon the dentin matrix.
Indexing terms: Biomimetics. Dentin-bonding agents. Longevity.
RESUMO
As diversas funções e aplicabilidades clínicas dos sistemas adesivos os tornaram parte fundamental da terapêutica restauradora. O desafio maior destes sistemas está em prover qualificada adesão aos diferentes tecidos uma vez que estes são muito distintos em sua constituição. Para que essa escolha seja feita corretamente o dentista deve conhecer a origem, composição, mecanismo de ação e modo de aplicação de cada sistema. Os produtos disponíveis e o estado técnico, alcançados atualmente, tem possibilitado aos clínicos o desenvolvimento de uma filosofia de máxima conservação tecidual, estética otimizada, atualização de condutas e conceitos bem como função plena do elemento dental restaurado compatíveis com uma filosofia biomimética. A literatura vigente apresenta superioridade de resultados com adesivos de condicionamento total de três etapas, uso de clorexidina como fator de aumento da longevidade e perspectivas futuras que incluem trabalhos com o uso de etanol, agentes inativadores enzimas liberadas no processo adesivo e a ação de agentes que atuem na malha dentinária.
Termos de indexação: Biomimética. Adesivos dentinários. Longevidade.
INTRODUCTION
Biomimetic philosophy aims to imitate nature in the conception of prosthetic rehabilitation solutions1. Aspects such as preservation, integration, function and aesthetics must be implicit in current restoration techniques.
The increasing demand for aesthetic restorations by today's society has rendered adhesive systems essential in dental practice. Their various clinical functions and applicability make them a fundamental part of restoration therapy. No matter what the aim of the adhesive procedure, the systems are, by definition, "the materials responsible for promoting a bond between the dental substrates and the restoration, thus acting as an intermediate material"2-3. With this in mind they should, ideally, be easy to use, have a simple technique, promoting good bonding to the various substrates that make up the dental element.
The major challenge of these systems lies in providing appropriate bonding to the different tissues as these have very different compositions4-5. If, on the one hand, the bonding to enamel can be satisfactorily achieved using the acid-etch technique, on the other hand, bonding to dentin is more complicated due to its tubular structure being humid; the properties of permeability and also the organic composition of its substrate4-7. Accordingly, the success of any technique depends on the proper selection of adhesive system and, therefore, choosing one for daily use has been regarded as a big challenge for professionals. For this choice to be properly made, the dentist has to understand the origins, composition, action mechanism and mode of application of each system8.
In recent years, a tendency to develop simplified, adhesive systems has been observed5,9 as they afford a smaller technical sensitivity on application7. However this is not tantamount to being a maxim that enables us to assert that the systems most recently developed or classified as being state-of-the-art, are clinically the ones that produce the best results. Thus it is appropriate to find out more about the different systems and their respective limitations.
Add to the above the fact that new paths are being explored to obtain longevity of bonding to dentin10. Several clinical parameters are already entrenched while others require clinical investigation to establish proof11.
The objective of this study was to analyze, through a review of the literature, the bonding strategies offered by the various adhesive systems, bringing up-to-date the concepts for the correct selection of these bonding agents and presenting fresh perspectives on scientific studies.
REVIEW OF THE LITERATURE
The observations of the diverse researchers, associated with the accumulated understanding over the last 50 years, have given rise to the development of Adhesive Dentistry.
In 1955, Buonocore12 introduced the use of the technique of acid etching of enamel, creating a fresh perspective on restoration procedures, kicking off the "Adhesive Era". In 1967, Gwinnett & Matsui demonstrated the intimate relationship between adhesives and the demineralized enamel substrate13. The technique that uses prior acid-etching was, for a while, called the "total-etch technique". However the application of this concept is not suited to the original acid-etching technique, as this technique was subsequently described by Fusayama et al.14, in 1979, as being the technique for the simultaneous etching of the enamel and dentin, when the etching of dentin and the use of stronger acids was not yet recommended, as described by Retief et al. in their 1974 study15. In 1982, Nakabayashi et al.16 reported that, to achieve a bond with the dentin substrate, it is necessary to perform acid etching so that the dentin's surface layer has its mineral phase partially or totally removed. This region, which was previously occupied by mineral, is then replaced by the adhesive solution. The bonding agent has to infiltrate this structure of collagen fibrils and polymerize in situ, forming what is known as the "hybrid layer"16.
After the dentin has been demineralized, the use of a wet-bonding technique is recommended to avoid the collapse of the collagen fibril structure, which could make it difficult to infiltrate the resin monomers. This study was performed by Kanca in 199217. Three years after the study by Kanca, Nakajima et al.18 reported that the bond strength results depend not only on the adhesive system used but also the type of dentin. Also in 1995, Yoshiyama et al.19 in their study concluded that for total-etch systems (this term should be understood as "simultaneous etching of the dentin and the enamel in a different step to the use of the adhesive system"), the depth of the dentin obtained in the cavity preparation alters the bond strength. Besides the dentin depth, the data obtained in this study suggest that this bond strength may also be influenced by the drying time of the primer used prior to the adhesive for two-bottle formulations.
In the same year, Sano et al. proposed the use of the term "nano-infiltration" as a result of observations under the microscope of alterations to the basal layer of the hybrid layer, even with the absence of restorative cracks at the adhesive interface20.
In 1996, Ikemura et al.21-22 presented their study on systems based on self-etching primers (this should be understood as "etching of the substrate promoted by its own adhesive system"). The possibility of the formation of hybrid layers using these systems was demonstrated.
In 1997, Perdigão et al.23 studied the bond strength of these self-etching primers to the enamel and found very low results for this category of adhesive.
The following year, Yoshiyama et al.24 corroborated the results of this low bond-strength to enamel. Pereira et al.7 supplied a further item of information about adhesive systems: bond strength can vary according to the dental substrate, region and type of adhesive system being used. In the same year, Rosales et al. presented their results on the contact angle of adhesive systems, demonstrating that with deep dentin and dehydrated dentin, the penetration of the systems is made more difficult. Then in 1999, Sano et al.25 published results of one year in vivo studies monitoring self-etching adhesives asseverating the viability of their clinical use.
Magne & Douglas26 introduced the concept of the biomimetic approach with restoration procedures, emphasizing the importance of bonding in this process. They described the use of adhering restorations as the pinnacle of results for both clinic and patient.
In 2001, Bouillaguet et al.27 presented the results of their micro-tensile tests on eight separate adhesive systems. Their study demonstrated superior results for two-bottle adhesives used in the three-step procedure.
As for Urabe et al.28, they obtained results in their research showing that the prevailing bonding systems could reproduce the biological adherence of the enamel to the dentin, in terms of tensile strength.
The same year, Bouillaguet et al.29 concluded that the ability of dentists to correctly manipulate adhesive systems varied greatly. However, if a dentist has sufficient experience and receives adequate training, any of the adhesive systems may culminate in satisfactory results. Also in 2001, Mak et al.30, in checking the bond strength between adhesive systems and resin cements, stated that the transudation of fluids through the adhesive would produce an accumulation of water at the interface between the adhesive and the cement, causing significant reductions in this bond and adversely affecting the adequate polymerization of the layer of cement in contact with the adhesive. In 2002, Tay et al.31, using transmission electron microscopy, concluded that the presence of silver nitrate in the adhesive layer represented sites with structural defects in the material itself and that this process also occurred with self-etching adhesives32.
In 2003, the same author demonstrated that the area of demineralized dentin not infiltrated by the resin was porous, permeable to external fluids, thereby permitting the occurrence of the so-called "nano-infiltration". This author defined simplified adhesives as "permeable membranes"31,33.
For Jacobsen et al.34-35, operator technique is more important to clinical success than the choice of material. Perdigão et al.36 reported that post-operative sensitivity could depend on the restoration technique and not the type of dentin adhesive used. Reis et al.8 concluded, in their research study, that each adhesive system possesses a different spectrum of humidity which must be observed in clinical operations so that greater adhesive forces may be obtained. Van Meerbeek et al.37 stated that, although there is a tendency to produce and use adhesive systems that are simplified in technique, scientific data originating from numerous laboratory and clinical studies show that the conventional three-step adhesive systems are the ones that demonstrate more favorable performance and the greatest credibility in the long run.
Carrilho et al.38 found that significant reductions in bond strength occurred after longitudinal storage in water whereas, when stored in oil, bond strength was preserved.
In the same year, Reis et al.39 demonstrated there was a relationship between dentin humidity after acid etching and the dentin bond strength of adhesives with different solvents. Bond durability and quality were related to the correct control over humidity in the dentin substrate.
Also in 2004, Pashley et al.40presented the concept of "host enzymes" in which products of the collagen matrix itself would likely be responsible for its degradation over time.
Carvalho et al.41, in their studies, showed that significant reductions in the bond strength to enamel occur in a short period of time when simplified, selfetching adhesives are used and that these affect the bond in dual cure resin cements, concomitant usage being incompatible. In another study conducted in 2005, the same author showed the presence of demineralized zones not infiltrated by adhesive monomers with various singlestep self-etching systems42.
The duration of the acid etching was assessed by Wang & Spencer43 suggesting that the application should be passive, for 15 seconds on the dentin with the Adper Single Bond (3M ESPE, St. Paul, MN, USA) adhesive system.
De Munck et al.44 concluded that the resin-dentin interface, created using the total-etch technique, has a propensity to degrade through water. In this technique, hydrolytic degradation is more critical for two-stage adhesives when compared to the three-step adhesive systems.
Bayne45, in 2005, carried out a study which provided morphological evidence that the discrepancies between the demineralization depth and infiltration depth of the adhesive resin can also occur when self-etching adhesive systems are employed.
Carrilho et al.46 published a study demonstrating the potential harmful effects of the storage media on the mechanical properties of resinous materials. They discussed the possibility of a reduction in adhesive quality due to this factor.
Aguilar-Mendonza et al.3 concluded that the wettability of the substrate is similar between self-etching and total-etch adhesives. The smear layer has little effect on the wettability of self-etching adhesives. They did emphasize, however, that the adhesive force of totaletch adhesives is greater than that obtained with the selfetching variety.
In 2010, Sadek et al.11 produced a study evaluating adhesive strength of specimens treated with chlorhexidine and with ethanol. Their study demonstrated that the adhesive potential endured for nine months when using chlorhexidine and 18 months when using alcohol.
The same year, Marshall et al.47 presented a conceptual review of the literature on adhesive systems. They concentrated on aspects such as dentin surface treatment, creation of a micromechanical interface through the formation of the hybrid layer and on its stability over time. They proposed that the researchers should be stricter in their evaluation of characteristics such as angle of contact and determination of surface energy also using atomic force microscopy for more detailed analyses.
Liu et al.10, the following year, discussed the limitations of bonding to dentin. Their review presented various strategies for promoting long-lasting adhesion. Techniques such as the use of chlorhexidine, ethanol and agents that promote alteration in the demineralized substrate were described.
Cardoso et al.48 performed a review of the literature on adhesive systems highlighting a number of areas of great importance to clinical procedure. They questioned, in longitudinal analyses, the gain in clinical time when using simplified adhesives to the detriment of bond quality. They argued for the three-step technique for two-bottle adhesives as the most viable on account of the stability of the adhesive interface. As far as the self-etching adhesives are concerned, they found that the most reliable were most likely those that are commercially presented in the form of two bottles.
Also in 2011, Brackett et al.1, after presenting in the introduction to the paper a review of the line of research in adhesive procedures, discussed an experiment to evaluate the effectiveness of chlorhexidine in vivo as a metalloproteinase inhibitor and which, consequently, would retain adhesive potential over time. They also presented the concept of biomimetic remineralization as a fresh alternative. The results were favorable for both procedures when compared to the control group, where the conventional adhesive procedure was carried out. After 12 months in vivo, chlorhexidine demonstrated its effectiveness in maintaining adhesive strength.
DISCUSSION
Contemporary dentistry has firm foundations in the adhesive process which enables the bonding of artificial materials to the hard tissue of teeth. This process creates hybrid structures in its final make-up, with the ability to have a beneficial effect on the processes that involve dental elements2. The bond between two structures favors the dissipation and distribution of load. In restorative procedures, this biomechanical behavior is of the utmost importance to the creation of final structures that behave in a similar way to intact teeth28. The creation of an interface47 between the tooth and the restorative material, described in the literature as a hybrid zone or layer16, is made possible through the modification of the structure of tissue that makes up the dental element and their impregnation by means of resinous materials13,16. The base procedure is promoted by the action of acidic substances interacting mainly with mineral compounds. The decalcification of the dentin and enamel is an essential prerequisite for this type of procedure12-13,37. Through the dissolving of hydroxyapatite crystals on the enamel and dentin mineral zones, spaces are created in which the resin system can be employed in liquid form and subsequently solidified. In a historical evaluation of this procedure we found that pioneering research did not succeed in promoting viable adhesive force when the acid treatment of the substrate was not effective due to its low concentration or due to it being contraindicated for dentin tissue15. The fear that the pulp could suffer irreversible injury due to the application of acid substances on the dentin, has meant that the procedure has developed more quickly with enamel but has achieved only slow progress on dentin. When more promising studies began to find evidence of improvements in the results of bonding to dentin, due to acid etching and noting that significant alterations were not found in the pulp tissue, a new obstacle came along for researchers in this area: the technical sensitivity of this procedure4-5. Unlike with enamel, several factors have to be checked in detail to obtain correct adhesion to dentin: Analysis of the depth of the cavity and proximity to the pulp7,19, duration of acid etching43, maintaining adequate humidity after etching2,17, length of time required to apply the adhesive materials19,34-35, chemical attributes of these materials4-5,36 and adequate polymerization10 are just some of the factors that can significantly influence bonding to dentin. The advances made in adhesive system research have sought to simplify as much as possible the clinical steps which could be influenced by the operator. Over the years, simplified systems have emerged to address this need24-25,35-36. Another positive for the development of these systems has been the reduction in the procedure's clinical time36. Thus the procedure carried out in three steps was reduced to two steps, followed by a further reduction, to just one step, and recently composite resins have appeared in the marketplace which even do away with the use of adhesive systems as they are designed to be self-etching (e.g. Dyad, Kerr, Orange, CA, USA). Several classifications have been proposed for adhesive systems9,45. One of the more commonly used is the classification by generation9. This standard does not appear to be the most viable as it implies the notion that the state-of-the-art adhesives have superior performance over adhesives of prior generations. Other classification methods are described via (a) methodology of usage and (b) the number of bottles of which the system is comprised45,48. The combination of these last two classifications coherently creates a more didactic concept for the selection of systems in everyday clinical applications. Thus we get the division shown in Table 1 for composite classification:
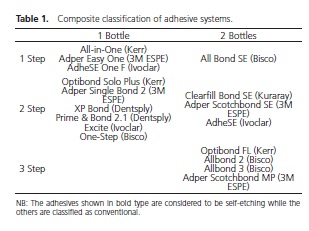
The steps may be represented by the following stages: 1) direct application of the product for self-etching adhesives or etching with phosphoric acid for conventional adhesives; 2) application of primers; 3) application of the adhesive.
As previously mentioned, the application of phosphoric acid as the initial stage of the adhesive procedure has been used for decades with effective results, particularly on enamel12-13,37. This composite promotes the adaptation of the substrate for subsequent impregnation of the adhesive system and consequent formation of a hybrid zone in which the in situ portion of the substrate interacts intimately with the artificial part of the adhesive systems. With dentin, the technique is seen to be more sensitive due to the control of humidity being intimately linked to adhesive potential17,39. The excessive retention of water prevents adequate penetration of the monomers and the reverse situation, the drying up of the dentin, promotes a collapse of the fibers reducing adhesive force17,38-39,46. Dentin's own characteristics result in the use of hydrophilic agents which should be used separately in the case of twobottle adhesives, the so-called primers, or in more complex, one-bottle composites where these substances are found in conjunction with solvents and monomers2,6-7,17,27,34.
Another factor to be considered is the potential inability of the adhesive system to penetrate the whole area which has been demineralized, thereby leaving behind non-impregnated collagen fibers40. This situation is clinically translated into post-operative sensitivity and nano-infiltration20,36. These were the main factors that led researchers to develop systems which could impregnate the substrate with monomers at the same time as they would promote demineralization of the tissue. These compounds, known as self-etching, were initially presented in two bottles whereby an acid primer was applied and subsequently a hydrophobic acid would perform the hybridization21-22. In this way, decalcified, non-mineralized zones would cease to occur, significantly reducing post-operative sensitivity. However in vivo studies have not supported this theory36. Subsequently, a new simplification was made through the introduction of self-etching systems using just one bottle, known as the all-in-one system. More detailed studies, however, have revealed a number of deficiencies with both systems: a) deficient bonding to enamel, and b) less durability of the adhesive interface31-32. Another relevant factor was their lack of compatibility with dualcure adhesive cements30,41. The simultaneous use of these materials does not allow the complete polymerization of the cement, thus promoting deficient bonding. Recently, bonding durability has been widely investigated. At the beginning of the evaluation, the results of adhesion force are very effective, but decrease with time for specimens stored in water38. The current literature points to two factors that contribute to this situation: the degradation promoted by the water on the bonding agent (silane) and the action of host enzymes present in the collagen fibers, which are released by the action of the acid used in the procedure10,40. Studies have concentrated on the correction of these factors by means of the total removal of water during the adhesive procedure and the use of chemical substances to promote the inactivation of the host enzymes1. Encouraging results have been obtained by using alcoholic substances (ethanol) to rinse the cavity prior to the impregnation of the substrate with the adhesive system, in an attempt to reduce the water in the interstice of the exposed fibrils10-11 and chlorhexidinebased compounds. The latter has permitted good results in the act of inactivating enzymes released by the collagen fibers in response to acid etching10, being a viable clinical procedure, already being used in practice, as a promoter of greater longevity for the adhesive interface with the dentin4,10-11. An in vivo analysis over a period of 12 months has shown the effectiveness of using chlorhexidine after the acid-etch phase1.
In longitudinal in vitro analyses4,10,40,42 and rare works on in vivo evaluations45 the three-step adhesives have proved themselves to be superior to the others in terms of performance10,45. These, however, are more sensitive in terms of technical performance. Studies have shown evidence of the low quality of results obtained with the use of adhesive systems when used by operators without due technical proficiency29,35. Consequently, after training, these bond strength values improve up to fourfold35. Despite the greater technical sensitivity, it is down to the professional to keep abreast of knowledge in the area in order to fully benefit from the three-step systems. The longer clinical time that these systems require (approximately 4 minutes) should not represent an obstacle in the quest for excellence of results for the patient with regard to the increased useful life of the restorations37.
In biomechanics, adhering means optimizing, providing better load transduction in the dissipation of forces by the dentin and consequently mimicking the natural model (biomimetic approach), i.e. the intact tooth26, where the different substrates are intimately imbricated by the enamel-dentin junction28 shaping an "intelligent design". Adhesives and the technical status they have currently achieved, have made it possible for clinics to develop a clinical philosophy in which maximum tissue conservation 47, optimized aesthetics, updating of procedures and concepts as well as the full function of the restored dental element predominate.
FINAL CONSIDERATIONS
The various adhesive systems currently available, as well as their different application techniques, foster the need to keep correct usage concepts up-to-date in the pursuit of maximum performance. The maximum understanding and benefit extracted from this procedure permit activity within a biomimetic philosophy. The reviewed literature revealed superiority of usage with three-step total-etch adhesives in spite of the longer clinical time taken. The use of chlorhexidine after acid etching is a viable procedure for obtaining greater longevity of the hybrid layer in dentin. Future perspectives include studies into the complete removal of water through the use of ethanol, the search for new substances that can inactivate the enzymes released in the adhesive process and the action of agents that act upon the demineralized dentin matrix by affording it better mechanical properties and longevity. There is a need for longitudinal clinical studies, rarely found in the existing literature, to confirm these procedures.
Collaborators
WA RICCI contributed to the conception and the composition of the article, the merits analysis for the articles appraised in the literature and to the final review. CPTP LUCAS contributed to the bibliographical survey in order to examine the prospects for studies of new adhesive procedures, formulated the initial structure of the scientific text and took part in the entire process, from the conception to the finalization of the article. ACG PIVETA and MM NAGLE contributed to the review of the literature. AAB MONTANDON directed the schematization of the topics to be covered in the introduction and the discussion, and took part in the composition of the article.
REFERENCES
1. Brackett MG, Li N, Brackett WW, Sword RJ, Qi YP, Niu LN, et al. The critical barrier to progress in dentine bonding with the etchand- rinse technique. J Dent. 2011;39(3):238-48. doi:10.1016/j. jdent.2010.12.009 [ Links ]
2. Latta MA, Barkmeier WW. Dental adhesives in contemporary restorative dentistry. Dent Clin North Am. 1998;42(4):567- 77.
3. Aguilar-Mendoza JA, Rosales-Leal JI, Rodríguez-Valverde MA, González-López S, Cabrerizo-Vílchez MA. Wettability and bonding of self-etching dental adhesives: influence of the smear layer. Dent Mater. 2008;24(7):994-1000. doi: 10.1016/j. dental.2007.11.013
4. Perdigao J. Dentin bonding-variables related to the clinical situation and the substrate treatment. Dent Mater. 2010;26(2):e24-37. doi: 10.1016/j.dental.2009.11.149
5. Perdigão J, Duarte S Jr, Lopes MM. Advances in dentin adhesion. Compend Contin Educ Dent. 2003;24(8 Suppl):10-6.
6. Lopes GC, Baratieri LN, de Andrada MA, Vieira LC. Dental adhesion: present state of the art and future perspectives. Quintessence Int. 2002;33(3):213-24.
7. Pereira PN, Okuda M, Sano H, Yoshikawa T, Burrow MF, Tagami J. Effect of intrinsic wetness and regional difference on dentin bond strength. Dent Mater. 1999;15(1):46-53.
8. Reis A, Loguercio AD, Azevedo CL, de Carvalho RM, da Julio Singer M, Grande RH. Moisture spectrum of demineralized dentin for adhesive systems with different solvent bases. J Adhes Dent. 2003;5(3):183-92.
9. Tay FR, Carvalho RM, Pashley DH. Water movement across bonded dentin - too much of a good thing. J Appl Oral Sci. 2004;12(spe):12-25. doi: 10.1590/S1678-77572004000500003
10. Liu Y, Tjäderhane L, Breschi L, Mazzoni A, Li N, Mao J, et al. Limitations in bonding to dentin and experimental strategies to prevent bond degradation. J Dent Res. 2011;90(8):953-68. doi: 10.1177/0022034510391799
11. Sadek FT, Braga RR, Muench A, Liu Y, Pashley DH, Tay FR. Ethanol wet-bonding challenges current anti-degradation strategy. J Dent Res. 2010;89(12):1499-504. doi: 10.1177/0022034510385240
12. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34(6):849-53. doi: 10.1177/00220345550340060801
13. Gwinnett AJ, Matsui A. A study of enamel adhesives: the physical relationship between enamel and adhesive. Arch Oral Biol. 1967;12(12):1615-20. doi: 10.1016/0003- 9969(67)90195-1
14. Fusayama T, Nakamura M, Kurosaki N, Iwaku M. Non-pressure adhesion of a new adhesive restorative resin. J Dent Res. 1979;58(4):1364-70. doi: 10.1177/00220345790580041101
15. Retief DH, Austin JC, Fatti LP. Pulpal response to phosphoric acid. J Oral Pathol. 1974;3(3):114-22. doi: 10.1111/j.1600-0714.1974. tb01703.x
16. Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982;16(3):265-73. doi:10.1002/jbm.820160307
17. Kanca J. Improving bond strength through acid etching of dentin and bonding to wet dentin surfaces. J Am Dent Assoc. 1992;123(9):35-43.
18. Nakajima M, Sano H, Burrow MF, Tagami J, Yoshiyama M, Ebisu S, et al. Tensile bond strength and SEM evaluation of caries-affected dentin using dentin adhesives. J Dent Res. 1995;74(10):1679-88. doi: 10.1177/00220345950740100901
19. Yoshiyama M, Carvalho R, Sano H, Horner J, Brewer PD, Pashley DH. Interfacial morphology and strength of bonds made to superficial versus deep dentin. Am J Dent. 1995;8(6):297-302.
20. Sano H, Takatsu T, Ciucchi B, Horner JA, Matthews WG, Pashley DH. Nanoleakage: leakage within the hybrid layer. Oper Dent. 1995;20(1):18-25.
21. Ikemura K, Kouro Y, Endo T. Effect of 4-acryloxyethyltrimellitic acid in a self-etching primer on bonding to ground dentin. Dent Mater J. 1996;15(2):132-43.
22. Ikemura K, Arai K, Hashimoto H, Kawakami T. Effects of aminobenzoic acid derivatives with 4-AET/HEMA in selfetching primer on bonding to ground dentin. Dent Mater J. 1996;15(2):144-53. doi: 10.4012/dmj.15.144
23. Perdigao J, Lopes L, Lambrechts P, Leitao J, van Meerbeek J, Vanherle G. Effects of a self-etching primer on enamel shear bond strengths and SEM morphology. Am J Dent. 1997;10(3):141-6.
24. Yoshiyama M, Matsuo T, Ebisu S, Pashley D. Regional bond strengths of self-etching/self-priming adhesive systems. J Dent. 1998;26(7):609-16. doi: 10.1016/S0300-5712(97)00046-8
25. Sano H, Yoshikawa T, Pereira PN, Kanemura N, Morigami M, Tagami J. Long-term durability of dentin bonds made with a self-etching primer, in vivo. J Dent Res. 1999;78(4):906-11. doi: 10.1177/00220345990780041101
26. Magne P, Douglas WH. Rationalization of esthetic restorative dentistry based on biomimetics. J Esthet Dent. 1999;11(1):5- 15.
27. Bouillaguet S, Gysi P, Wataha JC, Ciucchi B, Cattani M, Godin C, et al. Bond strength of composite to dentin using conventional, one-step, and self-etching adhesive systems. J Dent. 2001;29(1):55-61.
28. Urabe I, Nakajima S, Sano H, Tagami J. Physical properties of the dentin-enamel junction region. Am J Dent. 2000;13(3):129-35.
29. Bouillaguet S, Degrange M, Cattani M, Godin C, Meyer JM. Bonding to dentin achieved by general practitioners. Schweiz Monatsschr Zahnmed. 2002;112(10):1006-11.
30. Mak YF, Lai SC, Cheung GS, Chan AW, Tay FR, Pashley DH. Micro-tensile bond testing of resin cements to dentin and an indirect resin composite. Dent Mater. 2002;18(8):609-21. doi: 10.1016/S0109-5641(02)00005-2
31. Tay FR, Pashley DH, Suh BI, Carvalho RM, Itthagarun A. Singlestep adhesives are permeable membranes. J Dent. 2002;30(7- 8):371-82. doi: 10.1016/S0300-5712(02)00064-7
32. Tay FR, King NM, Chan KM, Pashley DH. How can nanoleakage occur in self-etching adhesive systems that demineralize and infiltrate simultaneously?. J Adhes Dent. 2002;4(4):255-69.
33. Tay FR, Pashley DH, Yoshiyama M. Two modes of nanoleakage expression in single-step adhesives. J Dent Res. 2002;81(7):472- 6. doi: 10.1177/154405910208100708
34. Jacobsen T. Bonding of resin to dentin. Interactions between materials, substrate and operators. Swed Dent J Suppl. 2003;(160):1-66.
35. Jacobsen T, Söderholm KJ, Yang M, Watson TF. Effect of composition and complexity of dentin-bonding agents on operator variability--analysis of gap formation using confocal microscopy. Eur J Oral Sci. 2003;111(6):523-8.
36. Perdigão J, Geraldeli S, Hodges JS. Total-etch versus self-etch adhesive: effect on postoperative sensitivity. J Am Dent Assoc. 2003;134(12):1621-9.
37. van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;28(3):215-35.
38. Carrilho MR, Carvalho RM, Tay FR, Yiu C, Pashley DH. Durability of resin-dentin bonds related to water and oil storage. Am J Dent. 2005;18(6):315-9.
39. Reis A, Loguercio AD, Carvalho RM, Grande RH. Durability of resin dentin interfaces: effects of surface moisture and adhesive solvent component. Dent Mater. 2004;20(7):669-76. doi: 10.1016/j.dental.2003.11.006
40. Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, et al. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004;83(3):216-21. doi: 10.1177/154405910408300306
41. Carvalho RM, Pegoraro TA, Tay FR, Pegoraro LF, Silva NR, Pashley DH. Adhesive permeability affects coupling of resin cements that utilise self-etching primers to dentine. J Dent. 2004;32(1):55-65. doi: 10.1016/j.jdent.2003.08.003
42. Carvalho RM, Chersoni S, Frankenberger R, Pashley DH, Prati C, Tay FR. A challenge to the conventional wisdom that simultaneous etching and resin infiltration always occurs in self-etch adhesives. Biomaterials. 2005; 26(9):1035-42. doi:10.1016/j.biomaterials.2004.04.003.
43. Wang Y, Spencer P. Effect of acid etching time and technique on interfacial characteristics of the adhesive-dentin bond using differential staining. Eur J Oral Sci. 2004;112(3):293-9. doi: 10.1111/j.1600-0722.2004.00127.x
44. De Munck J, van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84(2):118- 32. doi: 10.1177/154405910508400204
45. Bayne SC. Dental biomaterials: where are we and where are we going? J Dent Educ. 2005;69(5):571-85.
46. Carrilho MR, Tay FR, Pashley DH, Tjäderhane L, Carvalho RM. Mechanical stability of resin-dentin bond components. Dent Mater. 2005;21(3):232-41. doi: 10.1016/j.dental.2004.06.001
47. Marshall SJ, Bayne SC, Baier R, Tomsia AP, Marshall GW. A review of adhesion science. Dent Mater. 2010;26(2):e11-6. doi: 10.1016/j.dental.2009.11.157
48. Cardoso MV, de Almeida Neves A, Mine A, Coutinho E, van Landuyt K, De Munck J, et al. Current aspects on bonding effectiveness and stability in adhesive dentistry. Aust Dent J. 2011;56(Suppl 1):31-44. doi: 10.1111/j.1834- 7819.2011.01294.
 Correspondence to:
Correspondence to:
WA RICCI
e-mail: wricci@foar.unesp.br
Received on: 8/2/2012
Final version resubmitted on: 24/5/2014
Approved on: 6/6/2014













