Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.63 no.2 Porto Alegre Abr./Jun. 2015
ORIGINAL / ORIGINAL
Weight loss promoted by the Intra-oral Alimentary Satiety Device in a morbidly obese patient
Redução de peso promovida pelo Aparelho Intraoral de Saciedade Alimentar em paciente obeso mórbido
Mariane HALMENSCHLAGERI; Alexandre CONDEII; Simara Rufatto CONDEI; Thaís Rodrigues MOREIRAI
I Centro Universitário Univates, Curso de Nutrição. Rua Avelino Tallini, 171, Bairro Universitário, 95900-000, Lajeado, RS, Brasil
II Faculdade da Serra Gaúcha, Curso de Odontologia. Caxias do Sul, RS, Brasil
ABSTRACT
Objective
To evaluate the weight loss fostered by the Intra-oral Alimentary Satiety Device in a patient diagnosed as morbidly obese.
Methods
A female patient diagnosed as morbidly obese who was seeing a nutritionist was examined. Based on her medical history and anthropometric assessment, a hypocaloric diet was prescribed. The nutritional state was assessed by the Body Mass Index (BMI). The patient was advised to wear the Intra-oral Alimentary Satiety Device, and an assessment by a dentist was suggested to discard contraindications. The appliance was then manufactured with dental molding material, orthodontic stainless steel wire, and heat-cured dental acrylic resin. The patient wore the device at every meal, putting it on 5 minutes in advance. For the data analysis the SPSS Statistics 17.0 software was used.
Results
In her first consultation, the patient weighed 115 kg and was 1.62 m tall, with BMI = 43.82 Kg/m. Weight loss was 13.3 kg, representing 11.57% of the initial weight. In relation to the BMI, the total loss was 5.06 Kg/m, representing 11.55%.
Conclusion
The Intra-oral Alimentary Satiety Device can be considered a safe and effective method which, together with a hypocaloric diet, shows satisfactory results, thus proving to be an important auxiliary option in the treatment of obesity.
Indexing terms: Morbid obesity. Satiety response. Weight loss.
RESUMO
Objetivo
Avaliar a redução de peso promovida pelo Aparelho Intraoral de Saciedade Alimentar em paciente com diagnóstico de obesidade mórbida.
Métodos
Foi avaliada uma paciente do gênero feminino com diagnóstico de obesidade mórbida, frequentadora de um consultório nutricional. Realizouse a anamnese alimentar, avaliação antropométrica e indicação de dieta hipocalórica. A avaliação do estado nutricional foi realizada através do índice de massa corporal. A paciente recebeu a indicação da utilização do Aparelho Intraoral de Saciedade Alimentar e foi encaminhada para avaliação do cirurgião dentista para descartar as contraindicações, sendo então confeccionado com material de moldagem odontológico, fio de aço inoxidável ortodôntico e acrílico termopolimerizável odontológico. A paciente utilizou o aparelho em todas as refeições, colocando-o na cavidade oral com 5 minutos de antecedência. Para análise estatística foi utilizado o software SPSS versão 17.0.
Resultados
Em sua primeira consulta, a paciente estava com 115 kg e altura 1,62 m, apresentando IMC = 43,82 kg/m². A perda de peso total foi de 13,3 kg, representando 11,57% em relação ao peso inicial. Em relação ao IMC, a perda total foi de 5,06 Kg/m², representando uma perda em percentual de 11,55%.
Conclusão
O Aparelho Intraoral de Saciedade Alimentar pode ser considerado um método seguro e efetivo que aliado à dieta hipocalórica mostrou resultados satisfatórios, demonstrando ser uma importante opção coadjuvante no tratamento da obesidade.
Termos de indexação: Obesidade mórbida. Perda de peso. Resposta de saciedade.
INTRODUCTION
Obesity and overweight affect, worldwide, over 1.7 billion people and is associated with premature mortality, chronic diseases and increase in health costs. Characterized as a chronic disease with a multifactorial etiology, environmental factors and a genetic predisposition appear to be the main cofactors1. There are several factors that act and interact in the regulation of food intake and energy deposition, contributing to the development and maintenance of obesity, including: endocrinal, adipose, intestinal and neuronal factors2.
According to data from the Brazilian Household Budget Survey Brasileira3 held between 2008 and 2009, about half of the adult population had excess body weight. This excess in male adults increased from 18.5% in 1974 to 50.1% in the year of the survey. Among female subjects, the study showed that 48% were overweight, compared to 28.7% in 1974. In the Southern region the prevalence of excess weight was 56.8% for males and 51.6% in females as well as being the region with the highest percentage of obesity: 15.9% of men and 19.6% of women.
Obesity is considered a risk factor for many diseases that contribute to increased morbidity and mortality, such as type 2 diabetes mellitus, dyslipidemia, hypertension, ischemic heart disease, strokes and some types of cancer1. The main modifiable risk factor in the development of coronary artery disease is obesity, giving it a degree of cardiovascular risk similar to that associated with hypertension, hyperlipidemia, smoking and sedentarism4. Currently, the main treatments available to aid weight reduction are dietary guidance, the practice of supervised physical activity and the use of anti-obesity drugs. However, patients usually quickly abandon this type of treatment, leading to unsatisfactory results and obtained for shorter periods of time5. On the other hand, the demand for surgical intervention in patients with morbid obesity has increased significantly throughout the world, due to its effectiveness, safety and reduction in costs of health systems6.
Studies in several countries have found an increasing trend in the prevalence of third degree obesity or morbid obesity compared to the prevalence of first and second degree obesity. In Spain there was an increase of over 200% in the prevalence of morbid obesity between 1993 and 2006, from 1.8 to 6.1 cases per thousand inhabitants7. In the US, the prevalence of third degree obesity or morbid obesity was estimated at 4.7%. In Brazil, this data is not yet well defined, but is estimated to be around 0.5 to 1% of the adult population8.
In dentistry, the search for a solution to excess weight and obesity through an intraoral device with palatal allocation is not new. Brown & Comstock9 applied for a patent which referred to a metal device for this purpose. Gustafson10, with another device, registered his invention which consisted of a mobile acrylic device. Costigan & Costigan11 developed another acrylic oral device with a similar purpose. Apelbaum & Silveira12 in their invention for the purpose of regulating food intake, also registered their intraoral invention for allocation in the palatal region.
In this context, a new, non-surgical and nonpharmacological method was developed in order to contribute to weight reduction and long term maintenance of normal weight. This method is based on the use of an oral appliance that aims to stimulate earlier satiety by pre-absorptive means. This method is called the AIOSA (Intraoral Food Satiety Apparatus) and is considered a non invasive method, without risk to the patient and which aims to promote earlier food satiety by using it only during meals13.
This study aimed to evaluate the weight loss promoted by the AIOSA, associated with nutritional therapy in a patient with a diagnosis of morbid obesity.
METHODS
This work is characterized as a case study. The inclusion criteria were: an adult aged between 25 and 45 years, sedentary and with a diagnosis of morbid obesity. Exclusion criteria were: children, adolescents, the elderly, pregnant women, postpartum women; adults who did not agree to participate and did not sign the informed consent; adults who had any pathology that implied significant changes in their diet; adults using drugs for weight loss.
Morbid obesity is defined by body weight criteria which establish that the individual has an increase of 100% in their ideal weight or an excess of 45- 50 kg with respect to their ideal weight, which includes men weighing over 120-130 kg and women weighing over 100-110 kg14. The World Health Organization (WHO) uses the Body Mass Index (height / weight²) and the associated risk of mortality, with the definition of third degree obesity or morbid obesity being when the BMI exceeds 40 kg / m²15.
A female patient, aged 42, was assessed, with a diagnosis of morbid obesity, who habitually attended a nutritional consultancy and consented to participate in the study by signing the Informed Consent (IC). This patient was selected after an initial consultation with the professional nutritionist, in which her dietary record was made and anthropometric assessment carried out.
In her dietary record data was collected regarding eating habits, medical history and lifestyle. The anthropometric assessment was carried out for the variables height and weight. Weight was measured with a Welmy brand R-110 model scale (Welmy Indústria e Comércio Ltda., Santa Barbara d'Oeste, Brazil), with the patient barefoot, standing in the center of the platform, wearing light clothing, taking the reading to the closest 0.1 kg. Height was determined by a Welmy brand R-110 model stadiometer (Welmy Industria e Comercio Ltda., Santa Barbara d'Oeste, Brazil) attached to the scale the patient being barefoot, with her weight evenly distributed between her limbs and her feet as close together as possible, taking the reading to the nearest 0.1 cm. The assessment of the nutritional status of the patient was carried out using the body mass index (BMI), and classified according to the criteria of the World Health Organization15 as morbid obesity.
The use of the AIOSA was recommended for the patient and she was referred for evaluation by the dentist to discard any contraindications to the device. The AIOSA was made and its use explained to the patient and it was then used by the patient at every meal by placing it on her palate five minutes before eating. The AIOSA was made with dental mold material, orthodontic stainless steel wire and acrylic dental thermopolymerizable acrylic in accordance with the Conde & Conde patent16.
After the patient had the AIOSA fitted, she returned to the nutritionist where she was given a prescription for a reduced calorie diet, which was calculated using the equation recommended for obese patients17, using 25 kcal / kg ideal weight / day. The diet was divided into six meals a day with a total of 1748.5 Kcal / day and the caloric distribution of macronutrients was 54.7% carbohydrates, 20.4% proteins and 25% lipids in accordance with the recommendation of the Dietary Reference Intakes (DRI)18. The prescription of micronutrients followed the DRI recommendations for the gender and age of this patient. Consultations with the nutritionist to monitor the development of weight and for guidance on the proper use of the AIOSA, were carried out fortnightly, totaling 120 days of study.
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) software, version 17.0, carrying out a descriptive statistical analysis. This study was approved by the ethics committee of the Univates University Center with protocol number 024/11.
RESULTS
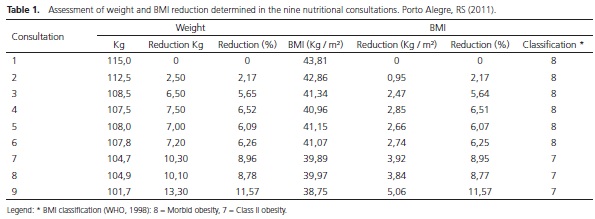
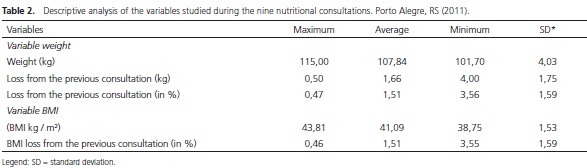
Table 1 shows the evolution of weight and BMI of the patient after starting to use the AIOSA associated with nutritional intervention. The consultations were fortnightly. At the first visit, the patient weighed 115 kg and was 1.62 m tall, with BMI = 43.82 kg / m², classified as morbidly obese according to the WHO, 1998. In the last consultation the patient weighed 101.7 kg and had a BMI of 38,75kg / m², being then classified as Class II obesity, according to the WHO, 1998. The percentage variations of reduction for BMI and weight were 11.57% and 11.57% respectively, considering the nine consultations, compared to baseline values.
In relation to the variation in weight (Table 2), it was observed that on average, the patient lost 1.66 kg at each visit and the total weight loss at the end of the 9 visits was 13.3 kilograms (Table 1). As regards the BMI, the average loss at each visit was 1.51 kg / m² and the total loss at the end of the 9 visits was 5.06 kg / m².
DISCUSSION
Body weight is the result of the balance of energy and nutrients over a given period of time, so a positive energy balance for months or years leads to excess weight and obesity2. Morbid obesity is a chronic disease characterized by an excessive accumulation of adipose tissue and visceral fat, and is a determining factor for the development of insulin resistance and Metabolic Syndrome19-20.
Several physiological factors and body mechanisms influence food intake and energy compensation, the main ones being: age and sex, which respond to anorexia processes and other eating disorders; body weight, which is influenced by hunger, satiety, food preferences and standards; gastric distension and emptying, which are related to satiety processes; peripheral and central hormones which act on gastric emptying, bowel transit, gastric and intestinal distension, blood glucose levels and hepatic metabolism21.
Therefore, satiety may be defined as a sensation in which the individual does not accept more food, since it is modulated by the hypothalamic nerve function in accordance with digestive, metabolic and endocrinal indices. Under normal physiological conditions, food is eaten after the perception of hunger and eating ceases when the feeling of satiety is achieved / reached22. Thus, food intake and energy expenditure are regulated by the hypothalamic region of the brain, which is also responsible for the expression of appetite which is chemically codified in this area2.
In the physiology of satiety, the chewing process produces a rich source of multiple impulses which further stimulate the satiety center, like those generated in muscle proprioceptors excited during the distension and contraction of the different muscle groups involved in mastigating, especially the muscles in the stomatognathic region. Similarly, nerve impulses generated at the temporomandibular joint, mobilized by jaw movements GWII receptors and periodontal distension receptors also contribute to the stimulation of the stomatognathic system23.
In this context, the AIOSA optimizes the stimuli originated by the system described above, stimulating satiety triggered via the pre-absorptive path of the stomathognatic region, inducing the individual to ingest smaller portions of food and to chew them more slowly. This method provides greater exposure of food in the mouth, stimulating the mechanoreceptors in the oral mucosa and conducting satiety stimuli to the hypothalamus that work by inhibiting the hunger center, providing as a result an earlier satiety13. However, the inhibition produced by gastric distension and the chemical signals of the circulating nutrients (glucose, amino acids and fatty acids) is even more lasting and intense compared to the intraoral pressure caused by chewing, salivation, and sense of taste24.
In this study nutritional therapy was associated with the use of the AIOSA because according to the study by Conde & Conde13, which worked with four different groups, it was shown that the exclusive use of the AIOSA promoted a weight reduction of 1.87% of the initial weight, However, the best results were obtained by the association of the apparatus with nutritional therapy (reduction of 7.83% of initial weight) surpassing the results solely with nutritional therapy (reduction 4.97% of initial weight). In this case study, the patient reached, at the end of 3 months, a reduction of 11.57% of her initial weight.
It is known that conventional, non-invasive, treatments of morbid obesity, such as nutritional therapy, physical activity, and use of anti-obesity drugs, often lead to a loss of 5 to 10% of the body weight, and are considered effective in controlling manifestations of metabolic syndrome, with improved lipid profile, glycemic control, blood pressure, among others5. However, the medium and long term results are unsatisfactory, because there is no maintenance of weight loss in most cases20.
The option of invasive treatment for patients with morbid obesity is bariatric surgery, which has proven effective in controlling various comorbidities and a substantial reduction in the risk of disease and mortality of surgical patients, with an appropriate reduction in BMI and body weight14.
The use of an intraoral device installed on the palate in search of food satiety has already been the target of research. In the study Walden et al.25, researchers evaluated another device manufactured by DDS System in which 32 adults aged 27-40 were divided into two groups and evaluated for 2 days. The results led the researchers to assert that the DDS system is associated with reduced food intake; however, there was no association of the device with satiety or reduction of hunger.
In our study, although we used an oral food satiety device and a different methodology from the study by Walden et al.25, the patient reported that when using the AOISA it was necessary to eat smaller portions of food and it was necessary to chew them for a longer period of time, which caused a reduction in food intake, since she felt the sensation of satiety earlier.
When compared to the other available methods for reducing weight, AIOSA demonstrated satisfactory results and without the risks and side effects encountered in the other methods. Weight reduction was obtained in a gradual and sustained manner, reaffirming the effectiveness of the method used.
CONCLUSION
The AIOSA can be considered a safe and effective method, which, combined with nutritional therapy, showed very satisfactory results, with a weight loss percentage higher than the other treatments currently available, proving to be an important adjunctive option for the treatment of obesity. It is important to emphasize that this is a non-invasive and non-pharmacological method, whose principle is to induce the individual to eat more slowly, encouraging earlier food satiety.
However, in order to obtain good results in reducing weight, the AIOSA methodology should be well indicated, well conducted and followed without deviation from its method; it is essential that the patient receives proper guidance on how to use it and, in this context, the professionals capacitated to indicate and carry out the treatment are the dentist, the nutritionist and the doctor, who should pass on all relevant information regarding it and reassure the patient that they will have all the necessary support for the success of their treatment.
Collaborators
M HALMENSCHLAGER was responsible for the development of the work, the literature review, the collection and processing of data, analysis and interpretation of data and writing of the article. A CONDE was responsible for the conception of the project, the methodological design and writing of the article. SR CONDE and TR MOREIRA were responsible for data analysis, guidance and writing of the article.
REFERENCES
1. Costa LD, Valezi AC, Matsuo T, Dichi I, Dichi JB. Repercussão da perda de peso sobre parâmetros nutricionais e metabólicos de pacientes obesos graves após um ano de gastroplastia em Y-de- Roux. Rev Col Bras. 2010;37(2):96-101. doi: 10.1590/S0100- 69912010000200005 [ Links ]
2. Halpern ZSC, Rodrigues MDB, da Costa RF. Determinantes fisiológicos do controle do peso e apetite. Rev Psiq Clin. 2004;31(4):150-3. doi: 10.1590/S0101-60832004000400002
3. IBGE. Fundação Instituto Brasileiro de Geografia e Estatística. POF - Pesquisa de orçamentos familiares 2008 - 2009: análise da disponibilidade domiciliar de alimentos e do estado nutricional no Brasil. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística; 2010.
4. Nordstrand N, Gjevestad E, Dinh KN, Hofso D, Roislien J, Saltvedt E. The relationship between various measures of obesity and arterial stiffness in morbidly obese patients. BMC Cardiovascular Disorders. 2011;11:7. doi: 10.1186/1471- 2261-11-7
5. Eid I, Birch DW, Sharma AM, Sherman V, Karmali S. Complications associated with adjustable gastric banding for morbid obesity: a surgeons' guide. Can J Surg. 2011;54(1):61-
6. doi: 10.1503/ cjs.015709 6. Victorzon M, Tolonen P, Sintonen H. Health -related quality of life in severely and morbidly obese patients waiting for bariatric surgery in Finland. Scand J Surg. 2010;99(3):122-6.
7. Basterra-Gortariab FJ, Beunzaa JJ, Bes–Rastrolloa M, Toledoac E, García-Lópezad M, Martínez-Gonzáleza MA, et al. Tendencia creciente de la prevalência de obesidade mórbida em España: de 1,8 a 6,1 por mil em 14 años. Rev Esp Cardiol. 2011;64(5):424- 6. doi: 10.1016/j.recesp.2010.06.010
8. Repetto G, Rizzoli J, Bonatto C. Prevalência, riscos e soluções na obesidade e sobrepeso: here, there, and everywhere. Arq Bras Endocrinol Metab. 2003;47(6):633-5. doi: 10.1590/S0004- 27302003000600001
9. Brown JS, Comstock CE, inventors; Brown JS, Comstock CE, assignee. Oral weight control device. United States patent US 4471771 A. 1984 Sep 18.
10. Gustafson L, inventor; Gustafson L, assignee. Oral device to aid weight control. United States patent US 5924422 A. 1999 Jul 20.
11. Costigan SH, Costigan BT, inventors; Costigan SH, Costigan BT, assignee. Lose at the source plate (L.A.T.S.Plate). United States patent US 2006/0185679 A1. 2006 Aug 24.
12. Apelbaum A, Silveira M, inventores; Apelbaum A, Silveira M, depositante. Regulador de ingestão intra-oral. Brasil patente PI 0803410-9. 2008 Maio 21.
13. Conde SR, Conde A. Avaliação da redução do peso por um aparelho intraoral de saciedade alimentar. Rev Bras Nutr Clín. 2010. 25(2):136-42.
14. Zilberstein B, Britto ACG, Joaquim HDG, Carballo MG. Banda gástrica com desvio jejunoileal: nova opção técnica em cirurgia bariátrica. Arq Bras Cir Dig. 2010; 23(2):105-7. doi: 10.1590/ S0102-67202010000200009
15. World Health Organization. Report of a WHO Consultation on Obesity: defining the problem of overweight and obesity. In: Obesity. Preventing and Managing the global epidemic. Geneve: WHO; 1998.
16. Conde A, Conde SR, inventores; Conde A, Conde SR, depositantes. Brasil patente PI 0902576-6. 2009 Jul 7.
17. Sociedade Brasileira de Hipertensão. I Diretriz Brasileira de Diagnóstico e Tratamento da Síndrome Metabólica. Arq Bras Cardiol. 2005;84(supl 1):3-28.
18. Trumbo P, Schlicker S, Yates AA, Poos M, Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol protein and amino acids. J Am Diet Assoc. 2002;102(11):1621-30.
19. Guimarães C, Pereira LRL, Junior NI, Cesarino EJ, Almeida CAN, Carvalho D, et al. Tolerability and effectiveness of fluoxetine, metformin and sibutramine in reducing antropometric and metabolic parameters in obese patients. Arq Bras Endocrinol Metab. 2006;50(6):1020-5. doi: 10.1590/S0004- 27302006000600007
20. Geloneze B, Pareja JC. Cirurgia bariátrica cura a síndrome metabólica? Arq Bras Endocrinol Metabol. 2006;50(2):400-7. doi: 10.1590/S0004-27302006000200026
21. Mourão DM, Bressan J. Influência de alimentos líquidos e sólidos no controle do apetite. Rev Nutr. 2009;22(4):537-47. doi: 10.1590/S1415-52732009000400009
22. Apolinário RMC, Moares RB, Motta AR. Mastigação e dietas alimentares para redução de peso. Rev CEFAC. 2008;10(2):191- 9. doi: 10.1590/S1516-18462008000200008
23. Douglas CR. Controle da ingestão alimentar. In: Guyton AC, Hall JE. Tratado de fisiologia aplicada à nutrição. São Paulo: Robe; 2002. p. 474-83.
24. Guyton AC, Hall JE. Balanços dietéticos; regulação da alimentação; obesidade e inanição. In: Guyton AC, Hall JE. Tratado de fisiologia médica. 10a ed. Rio de Janeiro: Guanabara Koogan; 2002. p.752-4.
25. Walden HM, Martin CK, Ortego LE, Ryan DH, Williamson DA. A new dental approach for reducing food intake. Obes Res. 2004;12(11):1773-80.
 Correspondence to:
Correspondence to:
TR MOREIRA
e-mail: th_rodrigues@ibest.com.br
Received on: 5/3/2012
Final version resubmitted on: 6/7/2012
Approved on: 7/12/2012













