Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.63 no.3 Porto Alegre Jul./Set. 2015
ORIGINAL / ORIGINAL
Reestablishment of the condyle-fossa and maxillomandibular relationships using a flat occlusal plane splint and implant-supported denture: case report with a 2-year follow-up
Restabelecimento das relações côndilo-fossa e maxilo-mandibular por meio de aparelho oclusal plano e próteses totais fixas implantossuportadas: relato de caso clínico com 2 anos de acompanhamento
Ana Lígia Piza MICELLII;Wilkens Aurélio BUARQUE E SILVAII; Frederico ANDRADE E SILVAII; Lígia Luzia BUARQUE E SILVAI; Josué Nogueira ALVESIII; Denise de Sa Maia CASSELLIIII
I Universidade Estadual de Campinas, Faculdade de Odontologia, Programa de Pós-Graduação em Clínica Odontológica. Av. Limeira, 901, Areião, 13414-903, Piracicaba, SP, Brasil
II Universidade Estadual de Campinas, Faculdade de Odontologia, Departamento de Prótese e Periodontia. Piracicaba, SP, Brasil
III Escola Cearense de Odontologia, Programa de Pós-Graduação em Implantodontia. Fortaleza, CE, Brasil
ABSTRACT
When the shape, structure, and/or function of one of the parts of the components of the stomatognathic system change, structural and physiological changes also occur to absorb or compensate the consequent loads. Hence, an insightful rehabilitation of this type of patient involves essential procedures, such as: correct orientation of the occlusal plane, determination of the vertical dimension of occlusion, and a stable and healthy maxillomandibular relationship, since the nonobservance of these aspects may result in prosthodontic rehabilitation failure. The objective of the present case study is to report the preoperative planning and prosthodontic rehabilitation of an edentulous patient with severe maxillary atrophy and signs and symptoms of temporomandibular disorders. The patient underwent flat occlusal plane splint therapy to reestablish the condyle-fossa and maxillomandibular relationships and muscle activity, followed by prosthodontic rehabilitation with implant-supported complete dentures. The maxillomandibular relationship was determined by the intraoral tracing technique, with a 24-month follow-up.
Indexing terms: Dental prosthesis, implant-supported. Temporomandibular joint. Vertical dimension.
RESUMO
Objetivo
Quando os componentes do sistema estomatognático sofrem alterações na forma, estrutura e/ou função de uma das partes, também ocorrem modificações estruturais e fisiológicas para a absorção ou compensação das resultantes criadas. Assim, uma criteriosa reabilitação deste tipo de paciente envolve procedimentos fundamentais, como: correta orientação do plano oclusal, determinação da dimensão vertical de oclusão adequada e a relação maxilo-mandibular estável e saudável, sendo que a não observação destes aspectos pode levar ao fracasso da reabilitação protética. O objetivo do presente caso é relatar o planejamento pré-cirúrgico e a reabilitação protética de um paciente edêntulo com atrofia severa dos maxilares e sinais e sintomas de Desordens Temporomandibulares, que foi submetido à terapia com aparelhos oclusais planos e lisos para restabelecimento das relações côndilo-fossa, maxilo-mandibular e da atividade muscular e, posterior reabilitação oral com próteses totais fixas implantossuportadas,onde a determinação da relação maxilo-mandibular foi realizada pela técnica do registro intraoral, com um período de proservação de 24 meses.
Termos de indexação: Prótese dentária fixada por implante. Articulação temporomandibular. Dimensão Vertical.
INTRODUCTION
When the components of the stomatognathic system work in harmony, their functions have maximum efficiency with minimal energy expenditure, working as a self-stimulatory system, that is, the function itself preserves and creates conditions that benefit the health of the system. Thus, when the shape, structure, and/or function of one the parts of the system change, structural and physiological changes also occur to absorb or compensate the consequent loads. These compensatory changes can cause morphological changes in some structures and/or their functions, and force the system to make a physiological compensation. Therefore, teeth can no longer be considered isolated elements because they are part of a system that decisively influences many physiological acts1.
Edentulism changes the position of the mandible in relation to the maxilla, as well as speech, deglutition, and aesthetics. An insightful rehabilitation of edentulous patients involves essential procedures, such as: correct orientation of the occlusal plane, determination of the vertical dimension of occlusion, and a stable and healthy maxillomandibular relationship1-2. The nonobservance of these aspects can result in oral rehabilitation failure.
Functional changes caused by edentulism can shorten the lower third of the face, compromising aesthetics, and cause poor fitting of complete dentures, accelerated dental wear, mandibular protrusion, an increase in the gonial angle, angular cheilitis, joint sounds, and pain3. However, incorrect lengthening can change phonetics and masticatory function; cause bad aesthetics, muscle discomfort, dental clenching, and difficulty reproducing the centric relation (CR); accelerate bone resorption; and injure the alveolar mucosa3.
Because of these aspects, prosthodontic rehabilitation procedures with unstable basic references for the reestablishment of occlusal and maxillomandibular relationships require the use of neuromuscular parameters to determine said relationships. The literature has suggested the use of flat occlusal plane splints4-5 for these cases in order to promote tonic reconditioning of the masticatory muscles by suppressing the proprioceptive mechanisms responsible for the maintenance of the altered muscle activity pattern5-6. Likewise, tracing and transferring this position to the articulator is a highly critical clinical procedure. In this sense, the use of intraoral tracing based on the precepts proposed by Gysi7, whose main characteristic is the reproduction of a mandibular position without mandibular manipulation and inductions, has been indicated for reproducing the position given by the voluntary muscle function.
Studies with an adequate follow-up period that assess the result of prosthodontic rehabilitation in patients with these characteristics may contribute to the differential diagnoses and efficiency of the available therapies.
Therefore, the objective of this study is to report a clinical case that involves the preoperative planning and prosthodontic rehabilitation of an edentulous patient with severe maxillary atrophy and signs and symptoms of temporomandibular joint disorders (TMD).
CASE REPORT
Clinical history and examination, and radiographic tests
A 57-year-old male patient visited the clinic of the Implantology Specialization Program of the Cearense School of Dentistry - ECO/SLM in Fortaleza (CE), wearing removable upper and lower complete dentures. He complained of difficulty chewing because of denture instability, bad aesthetics, and bilateral fatigue and pain in the temporomandibular joint (TMJ) and the masseter and temporal muscle regions during mastication. He reported having used the dentures for 10 years (Figure 1) and expressed the desire to replace them with fixed dentures. The patient did not report systemic diseases or surgeries that could compromise endosseous implants.

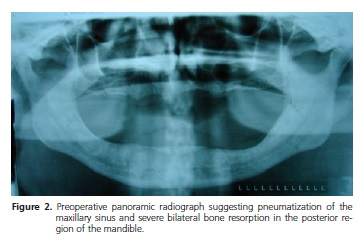
The patient underwent the clinical and physical assessments listed in the care protocol of the Cearense School of Dentistry. Extraoral examination found angular cheilitis and a vertical dimension of occlusion reduced by about 10 mm. Intraoral examination found extremely resorbed alveolar ridges and altered maxillomandibular relationship with the removable dentures, with high anteriorization of the mandible. No lesions were found in the attached gingiva or alveolar mucosa. The initial radiographic examination consisting of panoramic radiographs suggested maxillary sinus pneumatization and severe bilateral bone resorption in the posterior mandibular region (Figure 2). The patient was duly informed of the situation and signed an informed consent form as required by Resolution 466 of CNS/MS passed on October 10, 1996.
Differential diagnosis
The diagnosis was based on the clinical and scientific pieces of evidence, and the complaints expressed by the patient regarding removable denture instability and mastication difficulty, which could be associated with the probable disadaptation of the bases and reduced vertical dimension. Such aspects were confirmed by the presence of the following symptoms: bilateral fatigue and pain in the TMJ and masseter and temporal muscle regions when chewing. The fact that corroborates this hypothesis is the presence of angular cheilitis, reduced vertical dimension of occlusion, and mandibular anteriorization. The examination also detected severe resorption of the alveolar ridges.
Treatment
Given the complaint of complete denture instability during mastication and aesthetic problems, we proposed a rehabilitating treatment using complete dentures fixed on endosseous implants. The treatment was performed in three distinct stages. Initially we used the treatment protocol indicated by the Center for the Study and Treatment of Functional Changes of the Stomatognathic System of the School of Dentistry of the State University of Campinas5-6,8, which consisted of using a flat occlusal plane splint fabricated by waxing the plaster model of the upper complete denture mounted on a semi-adjustable articulator (Bio-Art Model 4000, São Paulo, Brazil) in maximum intercuspation. Once an initial reference for reestablishing the vertical dimension of occlusion was available, the incisal pin of the articulator was raised by 10 mm, equating the vertical dimension of occlusion with the vertical dimension at rest9. The splints were fabricated with colorless heat-polymerized acrylic resin (Vipi Wave - VIPI Indústria Comércio Exportação Importação de Produtos Odontológicos Ltda., Pirassununga, Brazil), respecting its flat and smooth anteroposterior and laterolateral configuration. Once finished and polished, the splint was adjusted to the upper complete denture to produce simultaneous bilateral contacts with maximum intercuspation and during excursive mandibular movements (Figure 3).
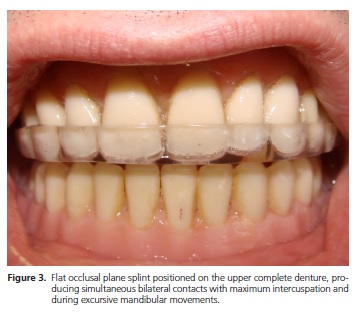
The patient was instructed to wear the splint for 180 days, removing it only during meals and oral hygienization. Twice a month we conducted adjustments to ensure simultaneous bilateral contacts with maximum intercuspation and during excursive movements, and clinical assessments of the initial signs and symptoms. The symptoms were reported by the patient during the adjustment sessions and investigated with a visual analog scale9. The intensity and frequency of the signs and symptoms decreased steadily during this treatment stage, culminating with remission of the initial symptoms.
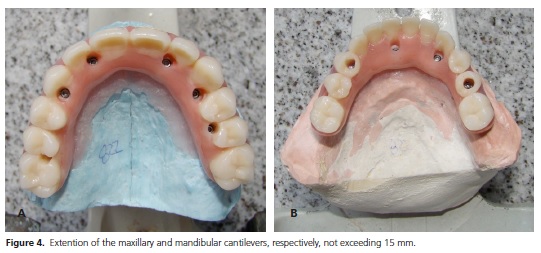
Concurrently with this stage the procedures for the second clinical stage were planned and implemented. The doubled complete dentures of the patient served as guides for computed tomography scans and the fabrication of surgical guides. The surgeries were conducted in two stages. The first stage consisted of installing the implants and the second, conducted six months later, consisted of opening and installing the pillars. Five implants were placed in the intraforaminal region of the mandible and six in the maxilla (Conexão Sistemas de Prótese Ltda., external hexagon, 4.0X10mm, Arujá, Brazil). The most posterior mandibular and maxillary implants were placed at 30o angles to ensure that the implant platform would be as distal as possible10. This angle should be compatible with the existing angulated pillars (on average 17o to 30o), reducing the cantilever extension and consequently, the lever effect, better distributing the mastication forces throughout the structure (Figure 4).
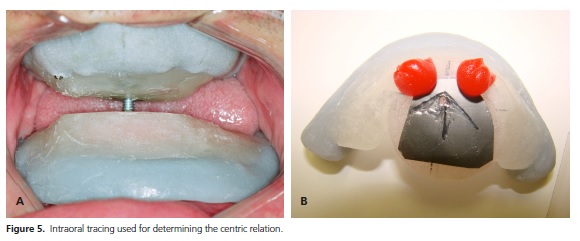
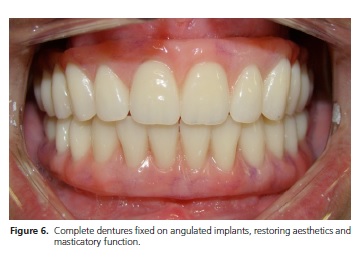
The patient used the occlusal splint described above during the healing period of six months (180 days). The third stage began after this period and consisted of the clinical and laboratory procedures involving the fabrication of the fixed complete dentures. After the open-mouth and closed-mouth impressions and fabrication of the final models, the upper model was mounted on a semi-adjustable articulator (Bio-Art Model 4000, São Paulo, Brazil) guided by the facial arch. The maxillomandibular relationship was determined and the lower model was mounted. Gysi's7 intraoral tracing technique was used for tracing and transferring the maxillomandibular position obtained by the occlusal splints, using as mounting reference the position 1.5 mm before the apex of the gothic arch8,11 (Figure 5). The vertical dimension of occlusion determined for the fixed dentures was the same as that used for the occlusal splints. The subsequent stages were common to the fabrication of the fixed implant-supported complete dentures, from implant impression and transference, and fabrication of the metal support, to tooth selection, aesthetic tests, and placement of the finished dentures (Figure 6).
The patient was thoroughly followed-up for 24 months after denture placement. The assessments were made at 90-day intervals, considering the following aspects: symptom recurrence assessed by the visual analog scale9; occlusal stability assessed by occlusal mapping, making sure the bilateral balanced occlusion type was maintained; loosening of the retention screws assessed with a digital screwdriver; and masticatory efficiency assessment based on the patient's report. None of the considered factors recurred after this period.
DISCUSSION
Occlusal splint therapy in patients with mastication muscle tenderness reduces the tenderness significantly12. Some authors consider occlusal splint therapy the first step in prosthodontic rehabilitation13-14. Fu et al.15 found 34% pain reduction in the temporomandibular joints and 44% joint sound reduction in patients who used occlusal splints for four weeks. The hypothesis supported by Hongchen et al.16 regarding the presence of the initial symptoms of the study patient, such as bilateral fatigue and pain in the TMJ and masseter and temporal muscle regions during mastication, can stem from tooth loss, which would promote a distal dislocation of the mandibular heads in the respective mandibular fossae and a shortening of the fibers of the mandibular elevator muscles, which could lead to their occurrence.
Flat occlusal plane splint therapy changes the activity pattern of the masticatory muscles17-18, equalizing the electric activities in electromyographic assessments. In this sense, some authors observed that the values obtained for the masseter and anterior temporalis tend toward a numerical approximation when compared bilaterally, indicating that the therapy promoted a bilateral balance between the muscles19-21. In the present case, the use of a flat occlusal plane splint had precise indication, helping to alleviate pain, recondition the muscles, and optimize the intra-articular space.
The reduction of the vertical dimension of occlusion caused by the wear in the dental structure or even by the absence of posterior teeth can change the position of the mandibular heads in the joint cavity, which can be considered a pathological position since it may reduce the joint space in its upper and posterior portion, suggesting condylar dislocation to a more posterosuperior position and mandibular anteriorization. Hence, the correct reestablishment of the vertical dimension does not only imply on aesthetic and functional improvements but also on the correct positioning of the condyles in the respective joint cavities22.
Casselli et al.1 assessed the freeway space (FS) in edentulous patients after the placement of bimaxillary complete dentures and found that after 60 days, the FS had increased by 1.18 mm. The authors suggested that this occurred because of the adaptive ability of the muscles: as their volume and length changes in response to stimulation, their density also changes, associated with a self-protective mechanism of the masseter muscle23. The roughly 10 mm increase in the vertical dimension of occlusion of the present case with the use of flat occlusal plane splints enabled muscle balance without compromising the aesthetics, phonetics, and especially, the masticatory function.
Ramos et al.12 conducted a study with fully dentulous patients with ideal occlusion and found that in the horizontal plane, between the mandibular position during deglutition and maximum intercuspation position, there was a space of approximately 1.5 mm before the apex formed by Gysi's7 gothic arch tracing, suggesting that in these patients centric occlusion coincided with the maximum intercuspation position. These authors also suggested that the use of intraoral tracing for determining centric occlusion results in less variability and greater reproducibility, favoring deglutition without any intraarticular compression12. In the study case the reference for mounting the final models for prosthodontic rehabilitation was the position suggested by the authors, obtained by gothic arch tracing.
The use of angulated endosseous implants proved to be a viable option for the rehabilitation of maxillary and mandibular atrophy because this technique reduces cost, treatment time, and morbidity associated with reconstructive surgeries. During masticatory function, the tensions generated on the occlusal surface of the denture are dissipated on the implants, affecting the implantbone interface and possibly causing bone resorption. The magnitude of this occlusal tension on the more distal implants increases with the angle of the implant10 or with the extension of the cantilever. Therefore, the study technique reduced the extension of the cantilever and consequently, the lever effect, better distributing the masticatory forces throughout the entire structure. Since the study case involved fixed complete dentures, the implants behaved as components of a single structure, the denture24-25. Although the resulting lateral forces resulting from the axial masticatory loads directly affected the bone adjacent to the implant, they were not great enough to change the structures around the implants (bone resorption), which indeed was not observed during the study period. A possible explanation can be related to the hardness of the structure, which is capable of resisting both the axial and lateral force vectors25.
The follow-up protocol was strict, and included clinical and radiographic assessments. None of the initial complaints, signs, and symptoms recurred. Despite the highly positive results, other studies should try to better understand muscle and TMJ behaviors during rehabilitation treatments.
CONCLUSION
The use of flat occlusal plane splints helped to reestablish the vertical dimension of occlusion and to distribute the masticatory forces on the dentures more evenly by allowing voluntary recovery of the condylar and mandibular positions and reestablishing muscle tone, which together with the intraoral tracing technique, allowed the dental position to coincide with the condylar position, contributing to optimal therapeutic performance.
Collaborators
ALP MICELLI prepared the manuscript, searched the literature, and wrote the article. WA BUARQUE E SILVA, F ANDRADE E SILVA, LL BUARQUE E SILVA, and DSM CASSELLI guided the clinical procedure and helped to write the article. JN ALVES helped with the clinical case and to write the article.
REFERENCES
1. Casselli H, Silva FA, Landulpho AB, Silva WAB. Electrognatographic evaluation of rehabilitated edentulous patients. Braz Oral Res. 2007;21(4):355-61. doi: 10.1590/ S1806-83242007000400013 [ Links ]
2. Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol. 1997;106(10 Pt 1):805-19.
3. Wagner AG. Complete dentures with an acquired protrusive occlusion. Gen Dent. 1989;37(1):56-7.
4. Massad JJ, Connelly ME, Rudd KD, Cagna DR. Occlusal device for diagnostic evaluation of maxillomandibular relationships in edentulous patients: a clinical technique. J Prosthet Dent. 2004;91(6):586-90. doi:10.1016/j.prosdent.2004.03.008
5. Vedana L, Landulpho AB, Silva FA, Silva WAB. Electromyographic evaluation during masticatory function, in patients with temporomandibular disorders following interocclusal appliance treatment. Electromyogr Clin Neurophysiol. 2010;50(1):33-8.
6. Silva WAB, Silva FA, Okino LA. Epidemiologic study of the temporomandibular disorders. J Dent Res. 2000;79:584-8.
7. Gysi A. The problem of the articulation. Part I. Dent Cosmos. 1910;52(1):1-19.
8. Paixão F, Silva WAB, Silva FA, Ramos GG, Cruz MVJ. Evaluation of the reproducibility of two techniques used to determine and record centric relation in Angle's Class I patients. J Appl Oral Sci. 2007;15(4):275-9. 10.1590/S1678-77572007000400007
9. Zanatta G, Buarque e Silva WA, Andrade e Silva F, Ramos GG, Casselli H. Assesment of painful symptomatology in patients with temporomandibular disorders by mean a combined experimental scale. Braz. J. oral Sci. 2006; 5(19): 1244-48.
10. Bevilacqua M, Tealdo T, Pera F, Menini M, Mossolov A, Drago C, et al. Three- dimensional finite element analysis of load transmission using different implant inclinations and cantilever lengths. Int J Prosthodont. 2008;21(6):539-42.
11. Ramos GG, Casselli H, Silva LLB, Silva FA, Silva WAB. Avaliação de duas técnicas para a obtenção da relação cêntrica em pacientes classe I de Angle. Pesqui Odontol Bras. 2006;20:249.
12. Canay S, Cinda A, Uzun G, Hersek N, Kutsal YG. Effect of muscle relaxation splint therapy on the electromyographic activities of masseter and anterior temporalis muscles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(6):674-9. doi:10.1016/ S1079-2104(98)90034-8
13. Wood GN. Centric relation and the treatment position in rehabilitating occlusions: a physiologic approach. Part II: The treatment position. J Prosthet Dent. 1988;60(1):15-8.
14. Clayton JA. Occlusion and prosthodontics. Dent Clin North Am. 1995;39(2):313-33.
15. Fu AS, Mehta NR, Forgione AG, Al-Badawi EA, Zawawi KH. Maxillomandibular relationship in TMD patients before and after short-term flat plane bite plate therapy. Cranio. 2003;21(3):172-9.
16. Hongchen L, Jilin Z, Ning L. Edentulous position of the temporomandibular joint. J Prosthet Dent. 1992 Mar;67(3):401-4.
17. Kawazoe Y, Kotani H, Hamada T, Yamada S. Effect of occlusal splints on the electromyographic activities of masseter muscles during maximum clenching in patients with myofascial paindysfunction syndrome. J Prosthet Dent. 1980;43(5):578-80.
18. Hamada T, Kotani H, Kawazoe Y, Yamada S. Effect of occlusal splints on the EMG activity of masseter and temporal muscles in bruxism with clinical symptoms. J Oral Rehabil. 1982;9(2):119-23.
19. Liu ZJ, Yamagata K, Kasahara Y, Ito G. Electromyographic examination of jaw muscles in relation to symptoms and occlusion of patients with temporomandibular joint disorders. J Oral Rehabil. 1999;26(1):33-47. doi: 10.1046/j.1365- 2842.1999.00356.x
20. Landulpho AB, Silva WAB, Silva FA. Efeitos dos aparelhos interoclusais nas disfunções têmporomandibulares avaliado através da eletromiografia. Rev Assoc Paul Cir. 2003;57(2):129-32.
21. Sheikholeslam A, Holmgren K, Riise C. A clinical and electromyographic study of the long-term effects of an occlusal splint on the temporal and masseter muscles in patients with functional disorders and nocturnal bruxism. J Oral Rehabil. 1986;13(2):137-45. doi: 10.1111/j.1365-2842.1986.tb00646.x
22. McCarroll RS, Naeije M, Kim YK, Hansson TL. Short-term effect of a stabilization splint on the asymmetry of submaximal masticatory muscle activity. J Oral Rehabil. 1989;16(2):171-6. doi: 10.1111/j.1365-2842.1989.tb01330.x
23. Hongchen L, Jilin Z, Ning L. Edentulous position of the temporomandibular joint. J Prosthet Dent. 1992;67(3):401-4.
24. Krekmanov L, Kahn M, Rangert B, Lindstrom H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15(3):405-14.
25. Hansen CA, DeBoer J, Woolsey GD. Esthetic and biomechanical considerations in reconstructions using dental implants. Dent CIin North Am 1992;36(3):713-41.
 Correspondence to:
Correspondence to:
ALP MICELLI
e-mail: analigiamicelli@hotmail.com
Received on: 14/7/2013
Final version resubmitted on: 3/5/2014
Approved on: 15/8/2014













