Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.64 no.1 Porto Alegre Jan./Mar. 2016
CLÍNICO / CLINICAL
Verruciform xanthoma: case report
Xantoma verruciforme: relato de caso clínico
Maria Carolina de Lima Jacy MONTEIROI; Cristiane FURUSEII; Larissa Cunha CÊI; Alexandre Freitas SANTANAI; Vera Cavalcanti de ARAÚJOI
I Faculdade São Leopoldo Mandic, Curso de Odontologia, Programa de Pós-Graduação em Patologia Bucal.
II Universidade Estadual Paulista Júlio de Mesquita Filho, Faculdade de Odontologia, Departamento de Patologia e Propedêutica Clínica. Araçatuba, SP, Brasil
ABSTRACT
Verruciform xanthoma is a rare, benign lesion, with a papillary aspect, asymptomatic, sessile, white colored, and well-demarcated, that occurs in the gingiva and alveolar mucosa. The histopathological aspect is characterized by the presence of macrophages with foam cytoplasm (xanthoma cells) confined to the soft papillary tissue. The etiology and pathogenic mechanisms are unknown, although some hypothesis, such as local trauma or viral origin have been suggested. The aim of this article was report a clinical case of verruciform xanthoma located in the gingiva showing the clinical and histopathological aspects.
Indexing terms: Xanthomatosis. Diagnosis. Oral pathology.
RESUMO
O xantoma verruciforme é uma lesão muito rara, benigna, com aspecto papilar, indolor, séssil, localizada, principalmente, na gengiva e mucosa alveolar, podendo ocorrer na pele e genitália. O grau de queratinização da superfície influencia na cor, variando de branca a vermelha. Histopatologicamente é caracterizado pela presença de macrófagos com citoplasma espumoso (células de xantoma) acumulados e confinados ao tecido conjuntivo papilar. Criptas invaginadas alternam-se com extensões papilares. As cristas epiteliais alongadas estendem-se para a lâmina própria em profundidade uniforme. Sua etiologia e patogênese são desconhecidas, apesar de várias hipóteses terem sido sugeridas, como trauma local ou viral. O diagnóstico diferencial pode incluir o papiloma escamoso, o carcinoma escamoso papilar e o condiloma acuminado. O tratamento é a excisão conservadora e o prognóstico é excelente. O objetivo deste trabalho foi relatar um caso clínico de xantoma verruciforme localizado na gengiva inserida mostrando seu aspecto clínico e histopatológico.
Termos de indexação: Xantomatose. Diagnóstico. Patologia bucal.
INTRODUCTION
Verruciform Xanthoma (VX) is a rare, benign, primary lesion that affects the oral mucosa that was described for the first time by Shafer in 19711. XV usually has a papillary or verruciform appearance, is sometimes associated with hyperkeratosis, and does not have a welldefined etiopathogenesis. It affects the two sexes in equal proportions, and there are reports of predilection for one of the sexes. The affected age-range is around 50 years of age, equally involving the maxilla and mandible, in which the gingiva (premolar area) is the site presenting greatest incidence of VX2. Generally, it presents as a small, asymptomatic, slow-growing lesion, that is either sessile or pedunculated, and pink or whitened. The most common area of occurrence is the oral masticatory mucosa (gingiva, palate), however, other uncommon areas may be affected by its existence, such as the lateral border of the tongue, jugal mucosa, and floor of the mouth3-6. Extra-oral areas, such as the vulva, scrotum and penis have been related7-10. Due to its clinical characteristics, many of these lesions are diagnosed as papillomas, condylomas, ordinary (vulgar) warts, leukoplasias and occasionally as verrucous or epidermoid carcinomas. Histopathologically, VX is characterized by papillary or verrucous projections associated with the proliferation of pavimentous stratified epithelium with hyperparakeratosis and numerous foamy cells (histiocytes)1. These cells are known as xanthoma cells and are confined within the lamina propria subjacent to the projections, and do not extend below the rete ridges2. In 1974, Zegarelli et al.12 demonstrated that VX has macrophages containing lipids within them, anD after immunohistochemical studies, they confirmed the macrophagic origin of the xanthoma cells13-14, in which their cytoplasm is PAS-positive2. The pathogenic mechanisms reported in the literature for VX comprise inflammation, virus, local trauma, lipid metabolism disorders and immunological changes7,12,15.
CLINICAL CASE
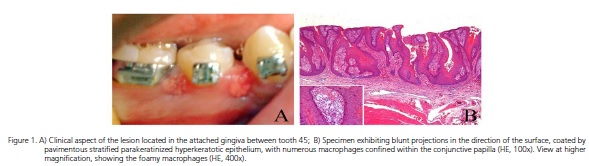
While the patient, a 21-year-old black man, was undergoing orthodontic treatment, he was referred to the stomatologist, presenting with two lesions located in the attached gingiva. On clinical exam, two papillary lesions were observed between the mesial and distal papillae of tooth 45. The lesions were pink, painless, of soft consistency, and measured approximately 0.5 cm in their largest diameter (Figure 1A). The patient reported that the lesions had appeared about one year ago, and he had previously had this type of lesion in the same place. An excisional biopsy was therefore performed to remove the lesion, and the material was sent for histopathological analysis. Under the microscope, a specimen was observed exhibiting blunt projections in the direction of the surface, with uniform depth, coated by pavimentous stratified parakeratinized epithelium, with numerous foamy macrophages confined in the conjunctive papilla. (Figure 1B) After histopathological analysis, the diagnosis was verruciform xanthoma. The patient is being followed-up, and up to the present date has presented no recurrence.
DISCUSSION
In this article, the authors report a clinical case of verruciform xanthoma in the attached gingiva. The clinical and histopathological findings are in agreement with those of other previously published case reports in the literature.
Verruciform Xanthoma is a rare, benign lesion, of which only 282 cases had been reported in the literature up to 20013. In the authors' laboratory, in a period from 2003 to 2007, only 3 cases were diagnosed as verruciform xanthoma, proving it to be a rare lesion. The other two cases were: a 14-year old white male patient, with the lesion located in the floor of the mouth, measuring approximately 1 cm in its largest diameter; and a 58-yearold white woman patient, with the lesion located in the labial mucosa, measuring approximately 1 cm in its largest diameter. Buchner et al.3 showed an incidence of 0.025% (in a total of 24,425 specimen evaluated in a period of 12 years, between 1968 and 1980).
VX mainly affects patients in the four and fifth decade of life4, at a mean age of 44.9 years, according to Oliveira et al.14, however, the present case showed a young patient of 21 years of age affected. According to the literature, the duration of the lesion is unknown, since it is usually diagnosed during a routine exam. However, according to the cases reported, the duration of the lesion ranges from 1 month to 10 years with a mean duration of approximately two years, in agreement with the case here related that had appeared 1 year before. The majority of lesions are clinically diagnosed in the wrong manner, as papillomas, therefore, verruciform xanthoma must be included in the differential diagnosis of oral lesions with a verrucous appearance.
In the case reported, the lesions were located in the attached gingiva, more precisely in the mesial and distal papillae of tooth 45. According to Philipsen et al.11, the most frequent site of occurrence is the attached gingiva, followed by the palate, tongue, jugal mucosa, floor of the mouth and alveolar mucosa.
As regards gender, the patient was a man. There is a discrete predilection for the male sex in a proportion of 1:1.111,16. However, not all authors take the gender of their patients into consideration in their studies. There appears to be predilection for Caucasian patients2,11,14. In the case presented, the patient was of Afro-Brazilian descent.
Clinically, the lesions presented a papillary aspect, pink to white color, measuring approximately 0.5 cm in the largest diameter of each lesion.
The size of oral VX lesions normally ranges between 0.2 to 2.0 cm3,4,16-17 with exception of a large lesion measuring 4.0 x 1.5 cm reported by Graff et al.19.
With regard to appearance, Neville et al., described that this may vary from "white and verruciform" to "red and ulcerated".
The main relevant clinical differential diagnosis in the case reported were papilloma and ordinary (vulgar) wart. According to the literature, the differential diagnosis must include lesions with a papillomatous or verrucous aspect, such as papilloma, condylomata acuminatum, common (vulgar) wart, verrucous carcinoma or even epidermoid carcinoma in the initial stage 11,20. The treatment of choice was to perform excisional biopsy of the two lesions, with excellent prognosis up to the present date. Treatment was performed by surgical excision, in which recurrence is extremely rare 16-17.
An interesting finding in the present case was the fact that the patient presented two oral lesions. According to Philipsen et al.11, in their review study of 282 cases, only four authors described multifocal occurrence (two or more lesions) of oral VX.
The case reported presented no other alteration in the oral cavity. Some previous studies have reported the association of a previous or concomitant lesion in the oral mucosa together with VX. These lesions included lichen planus8,26, penfigo vulgar6, carcinoma in situ10 and epidermoid carcinoma2.
Histopathologically, VX presents acanthotic and papillary epithelium covered by a thick layer of parakeratin. The gaps or crypts between the epithelial projections are filled with parakeratin, in which the papillary crests are elongated with uniform depth. The aspect that characterizes the lesion is the accumulation of numerous and large macrophages with foamy cytoplasm, confined within the papilla of connective tissue. These cells, known as xanthoma cells, contain granules of lipids and periodic Acid-Schiff (PAS) positive granules, resistant to diastase2, corroborating the case reported.
The etiology and pathogenesis of VX remain uncertain. Based on microscopy studies, Zegarelli et aL proposed that the foamy cells are macrophages with lipid granules, and oral VX may develop as a consequence of epithelial retention with subsequent degeneration and accumulation of lipids12. The authors suggested a local irritation as initial factor for the development of the disease, since oral VX is frequently found in the masticatory mucosa, where local trauma is very common7,12. This fact is most relevant, since in the case reported, the patient made use of an orthodontic appliance, and this is a possible local irritant that may cause appearance of the lesion. In the literature, trauma is taken into consideration in denturewearing patients 2. Iamarron et al studied 12 cases of VX by means of in situ hybridization and immunohistochemistry. They found that only 12 specimens of VX were positive for HPV subtype 6/11 by in situ hybridization. However, the predominant cells in the inflammatory infiltrate were T cells (51.8%) and 43.3% of the inflammatory cells were positive for HLA-DR. The authors suggested that an immune response could play an important role in the pathogenesis of VX. Rowden et al.15 demonstrated the presence of Langerhans cells in VX lesions by the positive marking of S-100, suggesting a possible immunological component in the pathogenesis of VX. Mostafa et al.23 suggested that VX could be a local immunological disorder mediated by T cells.
CONCLUSION
In the present case, the authors reported a case of VX with clinical and histopathological characteristics typical of the lesion, adding another case to the world literature, with a view to the rarity of this lesion. In spite of the etiopathogenesis continuing to be uncertain, immunohistochemical and molecular studies are being conducted, so that in the near future we may know the real cause of this lesion.
Contributors
MCLJ MONTEIRO was responsible for the clinical part of the case, and writing the article. C FURUSE was responsible for the anatomo-pathological part, photography and digitization of the images. L CÊ and A FREITAS participated in writing the article. VC ARAÚJO was responsible for the anatomo-pathological part of the study, photography, guidance of the work and writing the article.
REFERENCES
1. Shafer WG. Verruciform xanthoma. Oral Surg Oral Med Oral Pathol. 1971;31(6):784-9. [ Links ]
2. Neville BW, Weathers DR. Verruciform xanthoma. Oral Surg Oral Med Oral Pathol. 1980;49(5):429-34.
3. Buchner A, Hansen LS, Merrell PW. Verruciform xanthoma of the oral mucosa. Report of five cases and review of the literature. Arch Dermatol. 1981;117(9):563-5. doi: 10.1001/ archderm.1981.01650090045024
4. Takehana S, Kameyama Y, Fukaya M, Kawai T. Verruciform xanthoma of the gingiva: report of three cases. J Oral Maxillofac Surg. 1989;47(10):1079-81. doi: 10.1016/0278- 2391(89)90185-7
5. Kakarantza-Angelopoulou E, Nicolatou O, Anagnostopoulou S. Verruciform xanthoma of the palate: Case report with electron microscopy. J Oral Maxillofac Surg. 1991;49(4):409-12. doi: 10.1016/0278-2391(91)90381-U
6. Miyamoto Y, Nagayama M, Hayashi Y. Verruciform xanthoma occurring within oral lichen planus. J Oral Pathol Med. 1996;25(4):188-91. doi: 10.1111/j.1600-0714.1996.tb00218.x
7. Santa Cruz DJ, Martin SA. Verruciform xanthoma of thevulva. Report of two cases. Am J Clin Pathol. 1979;71(2):224-8.
8. Polonowita AD, Firth NA, Rich AM. Verruciform xanthoma and concomitant lichen planus of the oral mucosa. A report of three cases. Int J Oral Maxillofac Surg. 1999;28(1):62-6.
9. Toida M, Koizumi H. Verruciform xanthoma involving the lip: a case report. J Oral Maxillofac Surg. 1993;51(4):432-4.
10. Drummond JF, White DK, Damm DD, Cramer JR. Verruciformxanthoma within carcinoma in situ. J Oral Maxillofac Surg. 1989;47(4):398-400. doi: 10.1016/0278-2391(89)90343- 1
11. Philipsen HP, Reichart PA, Takata T, Ogawa I. Verruciform xanthoma—biological profile of 282 oral lesions based on a literature survey with nine new cases from Japan. Oral Oncol. 2003;39(4):325-36. doi: 10.1016/S1368-8375(02)00088-X
12. Zegarelli DJ, Aegarelli-Schmidt EC, Zegarelli EV. Verruciformxanthoma. A clinical, light microscopic, and electron microscopicstudy of two cases. Oral Surg Oral Med Oral Pathol. 1974 Nov;38(5):725-34.
13. Shin HI, Choi KS, Nagatsuka H, Murata M, Nagai N. Verruciform xanthomaof the oral mucosa: an immunohistochemical and ultrastructural study of two cases. Oral Oncol. 1997;33(4):279- 83.
14. Oliveira PT, Jaeger RG, Cabral LA, Carvalho YR, Costa AL, Jaeger MM. Verruciform xanthoma of the oral mucosa. Report of four cases and a review of the literature. Oral Oncol. 2001;37(3):326- 31. doi: 10.1016/S1368-8375(00)00068-3
15. Rowden D, Lovas G, Shafer W, Sheikh K. Langerhans cells inverruciform xanthomas: an immunoperoxidasstudyof 10 oral cases. J Oral Pathol. 1986;15(1):48-53.
16. Nowparast B, Howell FV, Rick GM. Verruciform xanthoma.A clinicopathologic review and report of fifty-four cases. Oral Surg Oral Med Oral Pathol. 1981;51(6):619-25.
17. Iamaroon A, Vickers RA. Characterization of verruciform xanthoma by in situ hybridization and immunohistochemistry. J Oral Pathol Med. 1996;25(7):395-400. doi: 10.1111/j.1600- 0714.1996.tb00285.x
18. Platkajs MA, Scofield HH. Verruciform xanthoma of the oral mucosa: report of seven cases and review of the literature. J Can Dent Assoc. 1981;47(5):309-12.
19. Graff SG, Burk JL, McKean TW. Verruciform xanthoma. First case reported in a black person. Oral Surg Oral Med Oral Pathol. 1978;45(5):762-7.
20. Yu CH, Tsai TC, Wang JT, Liu BY, Wang YP, Sun A, et al. Oral verruciform xanthoma: a clinicopathologic study of 15 cases. J Formos Med Assoc. 2007;106(2):141-7. doi: 10.1016/S0929- 6646(09)60230-8
21. Huang JS, Tseng CC, Jin YT, Huang CC, Wong TY, Chen HA, et al. Verruciform xanthoma. Case report and literature review. J Periodontol. 1996;67(2):162-5. doi: 10.1902/jop.1996.67.2.162
22. Neville BW, Damm DD, Allen CM. Oral and Maxillofacial Pathology. 2nd edition. Philadelphia: WB Saunders; 2002. p. 324-5.
23. Mostafa KA, Takata T, Ogawa I, Ijuhin N, Nikai H. Verruciform xanthoma of the oral mucosa: a clinicopathological study with immunohistochemical findings relating to pathogenesis. Virchows Arch A Pathol Anat Histopathol. 1993;423(4):243-8.
24. Gehrig RD, Baughman RA, Collins JF. Verruciform xanthoma in a young male patient with a past history of pemphigus vulgaris. Oral Surg Oral Med Oral Pathol. 1983;55(1):58-61.
25. Cobb CM, Holt R, Denys FR. Ultrastructural features of the verruciform xanthoma. J Oral Pathol. 1976;5(1):42-51.
26. Hume WJ, Smith CJ, Franklin CD. Verruciform xanthoma. Br J Oral Surg. 1980;18(2):157-61.
27. Miyamoto Y, Nagayama M, Hayashi Y. Verruciform xanthoma occurring within oral lichen planus. J Oral Pathol Med. 1996;25(4):188-91. doi: 10.1111/j.1600-0714.1996.tb00218.x
 Correspondence to:
Correspondence to:
MCLJ MONTEIRO
Rua José Rocha Junqueira, 13, 13045-755
Swift, Campinas, SP, Brasil
e-mail: kikamonteiro@yahoo.com.br
Received on: 25/10/2014
Final version resubmitted on: 10/4/2015
Approved on: 28/4/2015













