Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.64 no.3 Porto Alegre Jul./Set. 2016
ORIGINAL / ORIGINAL
Prevalence of peri-implant mucositis
Prevalência de mucosite peri-implantar
Paulo Sérgio Gomes HENRIQUESI; Ana Elisa Amaro RODRIGUESI; Daiane Cristina PERUZZOI; Luciana Satie OKAJIMAI; Nathália TREVENSOLLI (In Memoriam)I
I Faculdade São Leopoldo Mandic, Curso de Odontologia, Programa de Pós-Graduação
ABSTRACT
Objective
The aim of this study was to evaluate the prevalence of peri-implant mucositis, as well as hygiene care around implants and the correlation between keratinized gingiva and probing depth around implants.
Methods
The study consisted of 107 dental implants of 24 patients treated at Faculdade São Leopoldo Mandic who were evaluated for the presence of bleeding, presence of keratinized gingiva and implant placement time. Moreover, demographic data and oral hygiene methods used in the area of implants were obtained.
Results
The prevalence of mucositis in this population was 81.31% of the implants. The average percentage of bleeding score was 29.91%. Of the 107 implants, 52.34% had keratinized tissue. Regarding the use of interproximal tooth cleaning, 43% of patients used dental floss, 26.71% used interdental brush and 20.56% used single brush. It was observed only a weak negative correlation between marginal bleeding and presence of keratinized tissue (p <0.001, r = -0.27).
Conclusion
It can be observed a high prevalence of mucositis around the implants, which highlights the need for professionals' greater awareness about oral hygiene guidance and health promotion encouragement in patients receiving dental implant rehabilitation, as well as more studies to investigate the real role of keratinized tissue around implants.
Indexing terms: Dental implantation. Mucositis. Toothbrushing.
RESUMO
Objetivo
O objetivo desse estudo foi avaliar a prevalência de mucosite, bem como os cuidados de higiene bucal ao redor de implantes e a correlação entre a faixa de gengiva queratinizado e a profundidade de sondagem nos implantes.
Métodos
Foram avaliados 107 implantes dentários de 24 pacientes em atendimento na Faculdade de Odontologia São Leopoldo Mandic. Os implantes foram avaliados em relação à presença de sangramento, tecido queratinizado e tempo de instalação dos implantes. Além disso, foram obtidos dos voluntários, os dados demográficos, bem como informações sobre os cuidados e métodos de higienização utilizados na região dos implantes.
Resultados
A prevalência de mucosite foi de 81,31% dos implantes. A média de porcentagem de sangramento obtida foi de 29,91%. Dos 107 implantes, em 52,34% havia presença de tecido queratinizado. Quanto ao uso de métodos auxiliares para controle de biofilme, 43% dos pacientes utilizavam fio dental, 26,71% utilizavam escova interdental e 20,56% utilizavam escova unitufo. Foi observada apenas uma fraca correlação negativa entre sangramento marginal e presença de tecido queratinizado (p< 0,001, r= -0,27).
Conclusão
Pode-se observar uma alta prevalência de mucosite ao redor dos implantes, o que evidencia a necessidade de uma maior conscientização dos profissionais quanto à orientação de higiene bucal e incentivo à promoção de saúde em pacientes que recebem reabilitação com implantes dentais, bem como mais estudos investigando o real papel do tecido queratinizado ao redor dos implantes.
Termos de indexação: Implantação dentária. Mucosite. Escovação dentária.
INTRODUCTION
Peri-implant mucositis is a reversible inflammation, limited only to the soft tissues around the implant1 and it is caused by dental biofilm accumulation2-3. Soft tissue arrangement around the implants seems to be identical to that around the teeth4, but it is not. Mucositis is similar to gingivitis, although it has a more intense immuneinflammatory response.
Given the prevalence of mucositis, Zitzmann & Berglundh5 and Rinkee et al.6 have found its percentage to range from 39.4 to 80.0% in patients undergoing dental implants, while Marrone et al.7 have observed a prevalence of 31.0% of mucositis in patients rehabilitated with implants. In 2015, Derks & Tomasi8 conducted a systematic review reporting percentage 19-65%, with average values of 42.9% for meta-analysis of studies. These often asymptomatic diseases present slow development and their late resolution can normally be quite complex and end up in doubtful prognosis9. The progression of mucositis can develop into a peri-implantitis, in which the inflammation extends progressively and rapidly through the peri-implant tissues, since they present less efficient defense mechanisms than periodontal tissues10. This deficiency is largely due to lack of the periodontal ligament and a reduced number of fibroblasts and blood vessels11. Moreover, the soft tissue sealing, which typically consists of a narrow strip of circular fibers holding the tissues around the implants6, when exposed to bacterial attack causes loosening of this sealing likely resulting in peri-implant infection and then leading to the apical migration of the epithelium below the boneinterface implant7.
Some studies have examined the relationship between the need and/or the extent of keratinized tissue and the peri-implant tissue health. Most of the studies stated that there is the need for some adequate keratinized tissue range in order to optimize health maintenance around the implants. Recent studies have shown that despite good oral hygiene and periodontal maintenance therapy, implants with less than 2 mm keratinized tissue in the peri-implant region were significantly more prone to bleeding and exhibited a greater radiographic bone loss as well as higher labial soft tissue recession12-13.
Brito et al.14 have performed a systematic review of the importance of keratinized tissue concerning the maintenance of peri-implant health and the study has shown that patients without keratinized tissue presented better clinical outcomes when surgery was performed to increase this tissue. Surgeries such as to increase keratinized tissue may be indicated in the following cases: presence of inflammation sites, pain during brushing, recession sites and attachment loss, patients presenting higher periodontitis risk and poor oral hygiene patients13.
Peri-implantitis can be an unpredictable15 leading, ultimately, to implant loss (5-11%)16. Clinical important features such as early diagnosis of peri-implant mucositis and effective treatment are essential17. For a successful implant-supported treatment, the presence of healthy gingival tissue around the implants is of utmost importance. Other factors such as good biofilm control, patient's involvement, maintenance and commitment with their dental appointments and the good quality of restorations are great contributors for successful periimplant health18-19.
Therefore, it is essential to establish a clinical hygiene protocol for the different possibilities of implantsupported rehabilitation and the clear need for early diagnosis of mucositis.
The aim of this study was to evaluate the prevalence of mucositis, as well as hygiene around implants in a sample of patients from Faculdade São Leopoldo Mandic.
METHODS
This study was approved by the Ethics Committee of the Faculdade São Leopoldo Mandic under the protocol number 2012/0100.
The study target population consisted of 24 randomly chosen patients, who presented with 107 osseointegrated dental implants and were aged from 20 to 70 years. These patients were assisted at the Undergraduate and Graduate clinics of São Leopoldo Mandic. The exclusion criteria as follows: patients who did not sign the free and informed consent, smokers, diabetic patients, those who did not have previous radiographs and those who had undergone surgery in less than 12 months.
For these selected patients, the clinical examination consisted of Colorvue® (Hu-Friedy® - Chicago - IL) periodontal probe plastic resin use in order to diagnose bleeding around osseointegrated implants The survey was carried out by single calibrated examiner, on four surfaces per implant. The following data was recorded in each patient's medical report:
a) clinical history and demographics;
b) presence or absence of bleeding in the periimplant margin, according to Bleeding Index probing by Ainamo & Bay20, in which the mean bleeding percentage was obtained using the number of surfaces with marginal bleeding, divided by the total number of surfaces present;
c) presence and absence of keratinized tissue;
d) features concerning the patient's oral hygiene care related to the area of the implant such as flossing and the use of interdental and single brushes.
Data analysis was performed descriptively for the demographics and through the Pearson correlation test for quantitative variables and Spearman correlation test for qualitative variables.
RESULTS
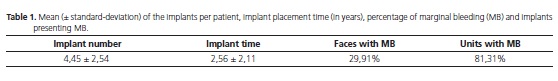
Of the 24 patients, 10 were female and 14 male, totalizing 107 implants, with an average of 4.45 (± 2.54) implants per patient, with an average time of implant placement of 2.56 (± 2.11) years. The mean percentage of bleeding, as measured by the number of surfaces with marginal bleeding, divided by the total number of surfaces, was 29.91% (Table 1). Out of these implants, 52.34% presented keratinized tissue around the margins.
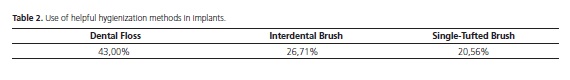
Regarding the use of auxiliary mechanical methods of biofilm control in implants, 43% of patients used dental floss, 26.71% for interdental brush and 20.56% made use of a single-tufted brush. Of the 107 patients, 9.07% did not use any auxiliary method and 17% associated more than one oral hygiene technique (Table 2).
A correlation analysis in order to evaluate the association between variables was performed: marginal bleeding, presence of keratinized tissue, flossing, use of interdental brush, use of single-tufted brush and implant placement time. A weak negative correlation was observed between marginal bleeding and the presence of keratinized tissue (p <0.001, r = -0.27). The other variables were not correlated.
DISCUSSION
Mucositis, despite being a reversible inflammation if left untreated can lead to the development of periimplantitis3. Therefore, early detection of disease and appropriate treatment is of utmost importance. All patients who have implants should belong to a support periodontal therapy program in order to prevent mucositis and peri-implantitis.
Some studies have investigated the possibility of circumferential seal of dense connective tissue as a prerequisite for the success of long-term dental implant. In the systematic review by Brito et al.13 the authors found three studies21-23 showing higher index rate of bleeding in implants with keratinized tissue width around implants measuring less than 2mm. Adibrad et al.24 reported that the absence of an appropriate keratinized tissue area around the implant presents significantly larger buildup biofilm scores, gingival inflammation, bleeding on probing as well as marginal recession.
This study showed a weak correlation between probing depth and the presence of keratinized tissue. The evaluation was dichotomized so the height of keratinized tissue was not measured. Thus, a definite final conclusion could not be described on the protective role of keratinized tissue in dental implants as it would require a more thorough investigation of the potential role that the keratinized tissue plays in the quality of the peri-implant tissue.
This study also assessed whether patients with implant performed conventional brushing using the Bass technique added to oral hygiene mechanical aids methods. It was found that less than half of the sample used interproximal cleaning devices or single-tufted brush. The prevalence of mucositis in this population was 81.31%. The data show the need for greater awareness while assisting patients receiving rehabilitation with dental implants and the need for thorough oral hygiene care as well as encouragement of health promotion. A regular periodontal maintenance program is also essential. Jepsen et al.25 reported that inadequate dental biofilm control has been associated with peri-implant disease. Marron et al.7 showed that high biofilm indices (30% or more) may increase the risk of peri-implant disease compared to patients with low index biofilm. One should take time to ensure that oral hygiene instructions are properly passed to the patient and that they have understood the importance of effective biofilm control.26 Thus, the patient's cooperation including biofilm control and attendance to periodontal therapy support are relevant factors to prevent the development of mucositis and periimplantitis25-27.
CONCLUSION
The high prevalence of mucositis and poor oral hygiene found in this sample population lead us to highlight the need for greater and better awareness by regarding dental implant specialists oral hygiene care and encouragement of health promotion for patients receiving rehabilitation with dental implants. Added to this is the importance of preventing periodontal disease around implants as well as avoiding complex and expensive treatment when they are affected by mucositis or periimplantitis. There is also evidence of the importance of a keratinized tissue band providing better maintenance of the peri-implant health.
Collaborators
PSG HENRIQUES, AEA RODRIGUES, DC PERUZZO, LS OKAJIMA and N TREVENSOLLI have throughly participated in all stages of the article preparation.
REFERENCES
1. Albrektsson T, Isidor F. Consensus report of session IV. In: Lang NP, Karring T (eds). Proceedings of the FIRST European Workshop on Periodontology. London: Quintessence Publishing Co.; 1994. p. 365-9. [ Links ]
2. Pontoriero R, Tonelli MP, Carnevale G, Mombelli A, Nyman SR, Lang NP. Experimentally induced peri-implant mucositis. A clinical study in humans. Clin Oral Implants Res. 1994;5:254-9. doi: 10.1034/j.1600-0501.1994.050409.x
3. Salvi GE, Aglietta M, Eick S, Sculean A, Lang NP, Ramseier CA. Reversibility of experimental peri-implant mucositis compared with experimental gingivitis in humans. Clin Oral Implants Res. 2012;23:182-90. doi: 10.1111/j.1600-0501.2011.02220.x
4. Schupbach P, Glauser R. The defence architecture of the human peri-implant mucosa: a histological study. J Prosthet Dent. 2007;97:S15-25. doi: 10.1016/S0022-3913(07)60004-3
5. Zitzmann NU, Berglundh T. Definition and prevalence of periimplant diseases. J Clin Periodontol. 2008;35:286-91. doi: 10.1111/j.1600-051X.2008.01274.x
6. Rinke S, Ohl S, Ziebolz D, Lange K, Eickholz P. Prevalence of periimplant disease in partially edentulous patients: a practice-based cross-sectional study. Clin Oral Implants Res. 2011;22(8):826-33. doi: 10.1111/j.1600-0501.2010.02061.x
7. Marrone A, Lasserre J, Bercy P, Brecx MC. Prevalence and risk factors for peri-implant disease in Belgian adults. Clin Bucal Implants Res. 2012;24(8):934-40. doi: 10.1111/j.1600-0501.2012.02476.x
8. Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015;42(Suppl. 16):S158–S171. doi: 10.1111/ jcpe.12334
9. Bauman GR, Mills M, Rapley JW, Hallmon WW. Plaque-induced inflammation around inplants. Int J Oral Maxillofac Implants. 1992;7(3):330-7.
10. Lang NP, Berglundh T, Working Group 4 of the Seventh European Workshop on Periodontology. Periimplant diseases: where are we now? - Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol. 2011 Mar;38(Suppl 11):178- 81. doi: 10.1111/j.1600-051X.2010.01674.x
11. Berglundh T, Abrahamsson I, Welander M, Niklaus PL, Lindhe J. Morphogenesis of the peri-implant mucosa: an experimental study in dogs. Clin Oral Implants Res. 2007;18(1):1-8.
12. Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP. Fiveyear evaluation of the influence of keratinized mucosa on periimplant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009;20(10):1170-7. doi: 10.1111/j.1600-0501.2009.01795.x
13. Esper LA, Ferreira Junior SB, Kaizer RF, Almeida AL. The role of keratinized mucosa in peri-implanted teeth. Cleft Palate Craniofac J. 2012;49:167-170. doi: 10.1597/09-022
14. Brito C, Tenenbaum HC, Wong BK, Schmitt C, Nogueira-Filho G. Is keratinized mucosa indispensable to maintain peri-implant health? A systematic review of the literature. J Biomed Mater Res B Appl Biomater. 2014 Apr;102(3):643-50. doi: 10.1002/jbm.b.33042
15. Faggion CM Jr, Listl S, Tu YK. Assessment of endpoints in studies on periimplantitis treatment- a systemic review. J Dent. 2010;38(6):443-50. doi: 10.1016/j.jdent.2010.03.003
16. Norowski PA, Bumgardner JD Jr. Biomaterial and antibiotic strategies for peri-implantitis. J Biomed Mater Res B Appl Biomater. 2009;88(2):530-43. doi: 10.1002/jbm.b.31152
17. Zeza B, Pilloni A. Peri-implant mucositis treatments in humans: a systematic review. Ann Stomatol (Roma). 2012;3(3):83-9.
18. Lewgoy HR, Matson MR, Matsushita MM, Forger SI, Tortamano P, Joly JC. Estabelecimento de um protocolo de higienização para prevenção de mucosites e peri-implantites. ImplantNews. 2012;9(1):11-9.
19. Thalji G , Bryington M, Kok IJ, Cooper LF. Prosthodontic management of implant therapy. Dent Clin N Am. 2014;58:207- 225. doi: 10.1016/j.cden.2013.09.007 20. Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25(4):229-35.
21. Langer B, Langer L. Overlapped flap: a surgical modification for implant fixture installation. Int J Periodontics Restorative Dent. 1990;10(3):208-15.
22. Landi L, Sabatucci D. Plastic surgery at the time of membrane removal around mandibular endosseous implants: a modified technic for implant uncovering. Int J Periodontics Restorative Dent. 2001 Jun;21(3):280-7.
23. Lee KH, Kim BO, Jang HS. Clinical evaluation of a collagen matrix to enhance the width of keratinized gingiva around dental implants. J Periodontal Implant Sci. 2010;40:96-101. doi: 10.5051/jpis.2010.40.2.96.
24. Adibrad M, Shahabuei M, Sahabi M. Significance of the width of keratinized mucosa on the health status of the supporting tissue around implants supporting overdentures. J Oral Implantol. 2009;35(5):232-7. doi: 10.1563/AAIDJOI- D-09-00035.1
25. Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol. 2015;42(Suppl. 16):S152-S157. doi: 10.1111/jcpe.12369
26. Renvert S, Polyzois IN. Clinical approaches to treat periimplant mucositis and peri-implantitis. Periodontol 2000. 2015 Jun;68(1):369-404. doi: 10.1111/prd.12069
27. Salvi GE, Ramseier CA. Efficacy of patient-administered mechanical and/or chemical plaque control protocols in the management of peri-implant mucositis. A systematic review. J Clin Periodontol. 2015;42(Suppl. 16):S187-S201. doi: 10.1111/jcpe.12321
 Correspondence to:
Correspondence to:
PSG HENRIQUES
Rua José Rocha Junqueira, 13
Swift, 13045-755
Campinas, SP, Brasil
e-mail: phenriques@mpc.com.br
Received on: 15/1/2016
Final version resubmitted on: 3/5/2016
Approved on: 9/6/2016













