Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RGO.Revista Gaúcha de Odontologia (Online)
versão On-line ISSN 1981-8637
RGO, Rev. gaúch. odontol. (Online) vol.64 no.3 Porto Alegre Jul./Set. 2016
CLÍNICO / CLINICAL
Vertical bone augmentation of posterior mandibular region: a description of two surgical techniques
Aumento ósseo em altura da região mandibular posterior: descrição de duas técnicas cirúrgicas
Adalmir Gonzaga dos Santos QUEIROZI; Yuri Slusarenko da SILVAII; Pedro Jorge Cavalcante COSTAIII; Flávio Wellington da Silva FERRAZI; Maria da Graça NACLÉRIO-HOMEMII
I Universidade de São Paulo, Divisão de Odontologia do Hospital Universitário. São Paulo, SP, Brasil
II Universidade de São Paulo, Faculdade de Odontologia, Departamento de Cirurgia Prótese e Traumatologia Maxilo-Faciais
III Faculdade São Leopoldo Mandic, Curso de Odontologia, Programa de Pós-Graduação em Odontologia. Campinas, SP, Brasil
ABSTRACT
Correction of severe vertical bone deficiency in the posterior region of mandibular alveolar ridge requires surgical management if implants are scheduled and cannot have primary stability. The aim of the present study is to report two cases; one treated with alveolar osteogenesis distraction and the other with segmental osteotomy with autologous graft interposition, by describing the surgical steps as well as show the results and experiences acquired with these techniques. We opted for these methods to reconstruct the posterior mandibular region after remarkable vertical bone loss based mainly by the height and thickness of the remaining bone. Alveolar osteogenic distraction is highly advisable when vertical deficiency is severe, and if these cases are treated with the segmental osteotomy and autologous graft interposition, complications as graft failure, necrosis and resorption are more prone to occur due to insufficient vascularization. After bone maturation and bone neoformation secondary to alveolar osteogenic osteogenic distraction and segmental osteotomy with autologous graft interposition, respectively, the two presented case reports were able to securely receive dental implants. In cases of vertical bone loss of the posterior mandibular region, both surgeries currently represent the best choice for bone gain prior dental implants placement for oral rehabilitation, without technical challenges, although biological evidence to assure the superiority of one technique over the other must be further investigated.
Indexing terms: Dental implants. Mandibular osteotomy. Osteogenesis distraction.
RESUMO
A correção de deficiência óssea severa em altura na região posterior do rebordo alveolar da mandíbula requer tratamento cirúrgico caso a inserção de implantes dentários seja necessária e não se pode ter uma estabilidade primária. O objetivo do presente estudo é relatar dois casos; um tratado com distração osteogênica alveolar e o outro com osteotomia segmentar associada à interposição de um enxerto autógeno, descrevendo a sequência cirúrgica, bem como mostrar os resultados e as experiências adquiridas com essas técnicas. Optamos por esses métodos para reconstruir a região mandibular posterior baseados principalmente na altura e espessura óssea remanescentes. A distração osteogênica alveolar é altamente recomendável quando essa deficiência é avançada e, se esses casos são tratados com a osteotomia segmentar e interposição de enxerto autógeno, complicações como falha do enxerto, necrose e reabsorção são mais prováveis de ocorrer devido à vascularização sua insuficiente. Após os períodos de reparação e neoformação óssea secundária à distração osteogênica alveolar e à osteotomia segmentar com interposição de enxerto autógeno, respectivamente, os dois casos relatados estavam aptos a receberem seguramente os implantes dentários. Nos casos de perda óssea em altura na região mandibular posterior, ambas as cirurgias representam, atualmente, a melhor escolha para o ganho de estrutura óssea antes da colocação dos implantes dentários e reabilitação oral, sem muita complexidade quanto à técnica cirúrgica, embora ainda sejam necessário estudos posteriores para assegurar a superioridade de uma técnica em relação a outra.
Termos de indexação: Implante dentário. Osteotomia mandibular. Osteogênese por distração.
INTRODUCTION
Correction of severe vertical bone deficiency in the posterior region of mandibular alveolar ridge requires surgical management if implants are scheduled and cannot have primary stability without bone augmentation. During physiologic atrophy, the mandible loses up to 60% of its osseous volume, characteristically in the body of the mandible posteriorly to the mental foramens, leading to an unsafe distance between the alveolar ridge and the mandibular canal that also preclude dental implants insertion1. When these scenarios occur, their correction include, among other techniques, alveolar osteogenic distraction (OD) and alveolar segmental osteotomy (SO) with placement of an inlay bone graft autologous. Both therapies demonstrate better clinical results when compared with other techniques2-4. The phenomenon of the alveolar osteogenic distraction consists of an application of a continuous slow and low-intensity traction in an opposite movement between the osteotomized alveolar ridge and the basal bone, exactly at the moment that this gap is filled with collagenous fibers (initial phase of bone healing), leading to a careful and delicate stretch of this premature tissue5-6. The alveolar segmental osteotomy technique, also known as alveolar segmental "sandwich" osteotomy3, consists of two verticals parallels and one horizontal inferiorly placed osteotomies (same manner as the DO) releasing the osteotomized alveolar ridge that will be slid superiorly until it reaches the occlusal plane, creating a large gap. After this, a block of autologous bone graft harvested from an intraoral area, commonly the mandibular ramus or symphysis, will be placed as an inlay into this gap and these structures fixed with a titanium miniplate or screw, promoting stability for osseointegration7. The purpose of the present study report two cases, one treated with OD and the other with segmental osteotomy SO with autologous graft interposition, by describing the surgical steps as well as show the results and experiences acquired with these techniques.
CASE REPORT
Case 1
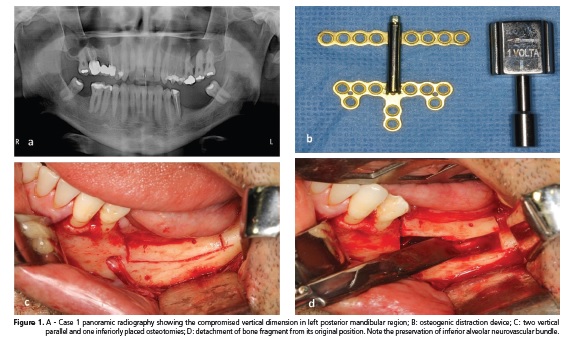
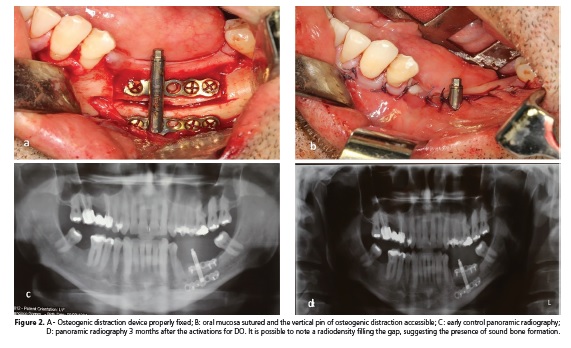
A 48-year-old male was referred to the Dentistry Division - University Hospital of São Paulo University for the correction of a vertical bone deficiency in the left posterior mandibular region, for dental implants placement. Intraoral examination revealed the presence of a lengthened partial denture that overlaid this edentulous area. Panoramic radiography demonstrated a severe vertical bone deficiency, making difficult the placement of implants due to the proximity between the alveolar ridge and the mandibular canal and inferior alveolar nerve. A OD was planned in order to gain hard and soft tissue simultaneously. The device used was an alveolar distraction device of 12 mm (Figure 1A,B). The procedure was undertaken under general anesthesia for patient and surgeon comfort. The surgical technique consists of a linear incision 3 mm below the mucogingival junction from the oblique line of the mandible to the ipsilateral tooth with a relieeving incision at this region, raising of a mucoperiosteal flap to expose the underlying bone. The osteogenic distraction device is prebent directly on the bone before the osteotomies. These osteotomies are two verticals parallels and one horizontal inferiorly placed, shaping a rectangle, and the cuts are perpendicular to the buccal and lingual corticals. They are performed with a sagittal saw handpiece and create the transport disc osteogenic distraction. The alveolar ridge segment is mobilized with the aid of chisels and any osseous interference that could difficult the alveolar OD process needs to be removed. After detachment, the alveolar ridge segment is left in place similarly to before bone osteotom (Figure 1C,D) and the distraction device is fixed with titanium screws in both the alveolar ridge segment and body of the mandible. It is important to plan adequately the perforations for screws insertion in order to avoid excessive bone damage and to place the perforations of the bone below the mandibular canal (Figure 2A). The flap is repositioned and the mucosa sutured. The pin of the distraction device remains in the oral cavity, allowing activations (Figure 2B). After postoperative latency, the OD starts and the clinician or the patient activates the pin of the device, turning it leftwards or rightwards depending on the manufacturer instructions (Figure 1B). As the distraction device pin is activated, the free alveolar segment slides upwards. The latency period consists in the initial inflammatory healing phase and varies between 5 to 10 days, permitting the immature bone to fill the gap. Our protocol recommends to start device activation at the seventh day as follows: a total of 0.66 mm daily activation, divided in two cycles of 0.33 mm in the morning and 0.33 mm at night, for a total of 15 days (total gain of 10 mm height) stopping the activation afterwards. In the present case, the distraction device was left in place for four months and was removed at the time of dental implants placement. The ideal time for removal is when it is expected the region to have a sound bone, commonly to the forth to sixth month postoperatively (Figure 2C,D). In the present case, the osteogenic distraction device was removed, under local anesthesia, about six months after the stop of activations and the patient was referred back to the service of origin for implant placement and finish the case with oral rehabilitation.
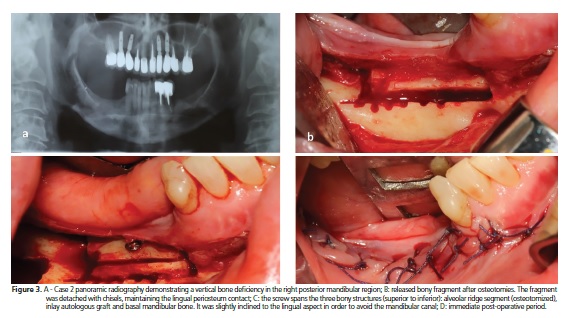
Case 2
A 54-year-old female patient was referred to the Dentistry Division - University Hospital of São Paulo University, for the correction of a vertical bone deficiency in the right posterior mandibular region, for dental implants placement. Intraoral examination revealed absence of all inferior molars teeth. Radiographically, vertical bone deficiency was observed in the right posterior mandibular region and an image suggestive of thickness deficiency in the left posterior mandibular region (Figure 3A). An SO was planned with the interposition of an inlay of autologous graft, harvested from the ipsilateral mandibular ramus. Also known as alveolar segmental "sandwich" osteotomy3, the procedure was also performed under general anesthesia for patient and surgeon comfort. The technique consists of a linear incision 3 mm below the mucogingival junction, similar to the incision employed for the OD technique, with a design of an envelope flap to expose the underlying bone. The gingival attachment of the lingual aspect must be preserved to maintain adequate blood supply to the graft and recipient area. The osteotom is identical to the OD technique (see Case 1) but were performed with a round drill handpiece. The alveolar ridge segment is detached and released with chisels followed by removal of any bony interference. After preparation of the recipient site, a corticocancellous bone graft harvested from the ipsilateral mandibular ramus is interposed between the detached alveolar ridge segment and the mandibular basal bone. The released segment, the inlay graft and the basal bone are fixed all together with one 1.5 mm long screw of 15 millimeters in length that crosses these three surfaces, assuring the stability required for the interpositional (inlay) graft (Figure 3B). By inclining the scren slightly obliquely, the surgeon avoids the mandibular canal and consequently the inferior alveolar neurovascular bundle. After screw fixation, the gingival flap is repositioned and sutured. Theoretically, the interfragmentary screw could be removed four to eight weeks after its placement to assure bone healing, but it may be wise to wait until dental implants have been placed, commonly at fourth to sixth month postoperatively to allow for sound bone for implant stability as well as ensuring a single procedure. In the present case, the screw was removed, under local anesthesia, about six months after its fixation and the implants were placed simultaneously to this procedure successfully.
DISCUSSION
Alveolar osteogenic distraction (OD) is indicated to treat severe vertical bony defects (or deficiencies) greater than 9 mm; however, smaller defects may also benefit from this procedure3. This technique offers a favorable stimulation for bone and soft tissue to grow simultaneously5-6. On the other hand, alveolar segmental osteotomy (SO) with inlay autologous graft is low cost and does not have the inconvenient intraoral pin of the osteogenic distraction device, which also demands daily distraction activation that is directly related to the amount and quality of bone gain. Nevertheless, the need of a donor area increases surgical morbidity that may be overcome with the interposition of a homologous graft like a freeze-dried human bone. However, autologous graft is still the best choice for the bone reconstruction of the posterior mandibular region prior to dental implants placement and prosthodontic rehabilitation8. The alveolar segmental osteotomy with inlay graft is indicated when vertical bone deficiency ranges between 4 to 9 mm. Together with the vertical bone gain the patient may also benefit from thickness gain, although the soft tissue remains unchanged9. The surgical protocol indicated for the OD suggests a device activation of 1 mm daily, but this protocol is classically used for long bones distraction. When the OD is used in the alveolar ridge, the 1 mm daily activation could lead to distraction failure and complications. Less of device activation is more secure, preventing oral mucosa perforation and, consequently, bone exposure as well as instability and hardware failure. All surgeries requires meticulous techniques to perform the osteotomies, in order to avoid excessive bone heating and preserve the inferior alveolar neurovascular bundle9. OD is highly advisable when vertical deficiency of alveolar region is severe and if these cases are treated with the SO and inlay graft, complications as graft failure, necrosis and resorption are more prone to occur secondary to insufficient vascularization. Suture dehiscence of the gingival mucosa may occur, facilitating graft exposure, infection and graft loss4. In case report 2, a suture dehiscence with minimal graft exposure occurred a few days after surgery and was cautiously treated with topical chlorhexidine at 0.12% for 21 days. This maneuver was sufficient to promote gingival tissue granulation and recuperation of graft coverage, maintaining its viability. Although the patients were under general anesthesia for the procedures, these surgeries may be permormed under local anesthesia in an outplatent enviroronment, with or without conscious sedation.
CONCLUSION
We conclude that in cases of vertical mandibular bone loss, the OD and SO currently represent the although biological evidence to assure the superiority of one technique over the other are is not well established.
Collaborators
AGS QUEIROZ, complete surgery and textual production. YS SILVA, textual production, the English revision and submission of the manuscript. PJC COSTA, participation of surgeries and textual production. FWS FERRAZ, complete surgery and image acquisition. MG NACLÉRIO-HOMEM, textual production.
REFERENCES
1. Ulm CW, Solar P, Blahout R, Matejka M, Watzek G, Gruber H. Reduction of the compact and cancellous bone substances of the edentulous mandible caused by resorption. Oral Surg Oral Med Oral Pathol. 1992;74(2):131-6. doi: 10.1016/0030- 4220(92)90370-6 [ Links ]
2. Kueppel LE, Nóia CF, Mazzonetto R. Osteotomia segmentar com enxerto interposicional. In: Mazzonetto R. Reconstruções em implantodontia, protocolos clínicos para o sucesso e previsibilidade. Nova Odessa: Napoleão; 2008. p. 248-66.
3. Mazzonetto R, Allais de Maurette M. Distração osteogênica alveolar. In: Mazzonetto R. Reconstruções em implantodontia, protocolos clínicos para o sucesso e previsibilidade. Nova Odessa: Napoleão; 2008. p. 268-87.
4. Simion M. Distraction osteogenesis vs onlay bone grafts and guided bone regeneration: what we know and what we suppose. J Oral Maxil Surg. 2002;60(6):722-23. doi: 10.1053/ joms.2002.33335
5. Ilizarov GA. The principles of the Ilizarov method. Bull Hosp Jt Dis Orthop Inst. 1988;48(1):1-11.
6. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and softtissue preservation. Clin Orthop Relat Res. 1989;238:249-81. doi: 10.1097/00003086-198902000-00029
7. Nóia FC, Andrade CV, Lopes OR, Mazzonetto R. Distração osteogênica alveolar e osteotomia segmentar com enxerto interposicional: revisão de literatura e considerações clínicas. Rev Elet Facimed. 2011;3:322-31.
8. Kueppel LE, Nóia CF, Mazzonetto R. Osteotomia segmentar com enxerto interposicional. In: Mazzonetto R. Reconstruções em implantodontia, protocolos clínicos para o sucesso e previsibilidade. Nova Odessa: Napoleão; 2008. p. 248-66.
9. Bormann KH, Suarez-Cunqueiro MM, von See C, Kokemüller H, Schumann P, Gellrich NC. Sandwich osteotomy for vertical and transversal augmentation of the posterior mandible. Int J Oral Max Surg. 2010;39:554-60.
 Correspondence to:
Correspondence to:
YS SILVA
Av. Professor Lineu Prestes, 2227, Cidade Universitária
05508-000, São Paulo, SP, Brasil
e-mail: yu.slu@hotmail.com
Received on: 7/3/2016
Final version resubmitted on: 28/4/2016
Approved on: 20/5/2016













