Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.8 no.2 Joinville Jun. 2011
CASE REPORT ARTICLE
Chronic graft versus host disease: a scleroderma-like case report
Claudio Maranhão PereiraI; Laura Guimarães MeloII; Patrícia Freire GasparettoI; Maria Elvira P. CorrêaIII
ISchool of Dentistry, Paulista University – Goiania – GO – Brasília – DF – Brazil
IISchool of Dentistry, Paulista University – Goiania – GO – Brazil
IIIDentistry Ambulatory, Hematology and Hemotherapy Center, State University of Campinas – Sao Paulo – Brazil
ABSTRACT
INTRODUCTION: Chronic graft versus host disease (cGVHD) is the most common consequence of allogeneic bone marrow transplantation, and it is associated with morbidity and mortality. Oral manifestations are diagnosed in approximately 80% of patients with chronic GVHD.
OBJECTIVE: To present a case of chronic GVHD with scleroderma-like lesions in skin and oral cavity
CASE REPORT: A 27-year-old female was admitted, in a Hematology Center, in 1997, with previous diagnosis of chronic myeloid leukemia since 1994. Over past four months after allogeneic BTM she developed cGVHD in eyes, mouth, liver, lungs and skin. The patient presented sclerotic skin changes, hyperkeratosis of hands and xerophthalmia.
CONCLUSION: Clinical manifestations of chronic GVHD are similar to autoimmune collagen vascular disease and the two main types of cutaneous chronic GVHD are lichenoid and sclerodermatous.
Keywords: bone marrow transplantation; graft-versus-host disease; oral cavity.
Introduction
Bone marrow transplantation (BMT) is the treatment of choice for lymphoma, aplastic anemia, various types of leukemia and immunodeficiency disorders [5]. Chronic graft-vs-host disease (cGVHD) is the most common complication following allogeneic BMT [10]. Chronic or late GVHD may appear months after transplantation and remain present for years [1, 5].
Oral manifestations, commonly expressed by atrophy, erythema, and lichnoides lesions on buccal and labial mucosa, have been diagnosed in approximately 80% of patients with chronic GVHD [1, 11]. The condition often shares the features of a variety of autoimmune diseases, such as lichen planus, Sjögren's syndrome, systemic lupus erythematosus or primary biliary cirrhosis [12, 13]. Lichenoid and sclerodermatous are the two main types of cutaneous chronic GVHD [14].
Scleroderma is a relatively rare connective tissue disorder characterized by skin fibrosis, obliterative vasculopathy and distinct autoimmune abnormalities. Many other clinical conditions present substantial skin fibrosis and may be potentially confused with Scleroderma, sometimes leading to a wrong diagnosis (eosinophilic fasciitis, systemic amyloidosis, scleromyxedema, graft-versus-host disease, progeroid disorders, stiff skin syndrome). In most cases, even when the etiology is known or suspected, the precise pathogenetic mechanisms leading to skin and tissue fibrosis remain elusive. Effective therapies are available for some of these conditions. For this reason, a prompt diagnosis is important to spare the patients from ineffective treatments and inadequate management [2, 7].
Although the oral manifestations are common, because the simultaneous involvement of the skin mimicking scleroderma leads to a decrease of the stomatognathic functions, these are not frequently reported in literature. Herein, we present one case of chronic GVHD with scleroderma-like lesions in skin and oral cavity with patient complaint of normal oral function loss.
Case report
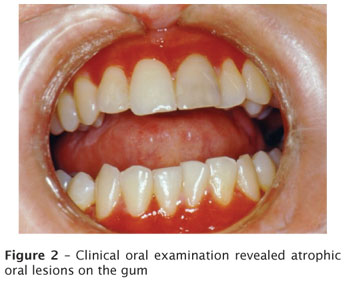
A 27-year-old female was admitted in a Hematology Center, Hemocentrounicamp, in 1997, with previous diagnosis of chronic myeloid leukemia since 1994. Patient underwent allogeneic BTM and two days later developed acute GVHD on intestine. Over past four months she developed cGVHD in eyes, mouth, liver, lungs and skin. The patient presented sclerotic skin changes, hyperkeratosis of hands and xerophthalmia. In oral cavity, she presented atrophic lesions on buccal mucosa, gum, upper and lower lips, floor of the mouth, xerostomia and microstomia (figures 1 and 2). The patient reported that the lesions caused considerable discomfort and affected her normal oral function. She also reported a weight loss since the beginning of the ulcers due to difficulty to eat. She received a protocol therapy using a daily dose of 100 mg cyclosporine and 10 mg prednisone; 400 mg aciclovir twice a day; 500 mg phenoxymethylpenicilin twice a day, combined with 100 mg fluconazole, 150 mg ranitidine daily; and 400mg Foraseq twice a day. Due to lesions clinical stabilization and improvement in performance of the stomatognathic functions, the therapy was considered successful. The patient is still under clinical control at Hemocentro/Unicamp.

Discussion
GVHD disease is the most common consequence of allogeneic BMT and the skin is the most commonly affected organ [5, 13]. Chronic GVHD could be present more than 100 days after BMT. It can occur either directly following acute GVHD or following a disease-free period [10].
Clinical manifestations of chronic GVHD are similar to autoimmune collagen vascular disease, such as oral ulcerations (lichen planus), keratoconjunctivitis sicca, xerostomia, polyserositis, esophagitis and stricture, intrahepatic obstructive liver disease, obstructive pulmonary disease, scleroderma, morphea, fasciitis. Lichenoid and sclerodermatous are the two main types of cutaneous chronic GVHD [1, 3, 5, 10, 14]. The oral mucosa is the most frequently involved site by chronic GVHD, and the clinical findings range from erythema to leukoplakia, lichenoid lesions, ulcers, mucosal atrophy, and xerostomia [11, 12].
Similarities between the clinical features of chronic GVHD and several autoimmune diseases have been commonly observed. Autoantibody formation has been noted in experimental models of chronic GVHD and clinical studies also report these findings [6, 7]. Occurrence of antinuclear, anti-double-stranded DNA, and anti-smooth muscle autoantibody ranges in frequency from 11% to 62% of patients with chronic GVHD, while anticytoskeletal and antinuclear antibodies have also been detected [6, 8, 9]. Although specific nucleolar phosphoproteins have been identified as targets of GVHD, the pathogenetic role for antibodies in chronic GVHD is still poorly defined [4].
The primary treatment of GVHD usually consists of therapy with systemic steroids and cyclosporine. In severe cases, if patients fail to respond to initial immunosuppressive therapy, several recovery protocols are available. Thalidomide and irradiation with Psoralem® and ultraviolet light (PUVA) have also been used, but their effects are limited and less effective, requiring further studies to optimize their uses [3, 10, 12].
The earlier and more accurately the cGVHD diagnosis can be made, the greater the success will be in predicting the outcome of the disease and in defining an optimum treatment at an early stage [10, 12]. In summary, the GVHD is a complex and dynamic process that requires the skills of a multidisciplinary health care team. Intervention is necessary for a successful prognosis for the BMT patient and to improve his quality of life.
References
1. Aractingi S, Chosidow O. Cutaneous graft-versus-host disease. Arch Dermato. 1998;134:602-12. [ Links ]
2. Boin F, Hummers LK. Scleroderma-like fibrosing disorders. Rheum Dis Clin North Am. 2008 Feb;34(1):199-220. [ Links ]
3. Chao NJ, Schmidt GM, Niland JC, Amylon MD, Dagis AC, Long GD et al. Cyclosporine methotrexate, and prednisone compared with cyclosporine and prednisone for prophylaxis of acute graft-versus-host disease. N Engl J Med. 1993;329:1225-30. [ Links ]
4. Dighiero G, Intrator L, Cordonnier C, Tortevoye P, Vernant JP. High levels of anti-cytoskeleton autoantibodies are frequently associated with chronic GVHD. Br J Haematol. 1987;67:301-5. [ Links ]
5. Eggleston TI, Ziccardi VB, Lumerman H. Graft-versus-host disease. Case report and discussion. Oral Surg Oral Med Oral Pathol Oral Radiol Endo. 1998;86:692-6. [ Links ]
6. Fialkow P, Gilchrist C, Allison AC. Autoimmunity in chronic graft-versus-host disease. Clin Exp Immunol. 1973;13:479-86. [ Links ]
7. Foti R, Leonardi R, Rondinone R, Di Gangi M, Leonetti C, Canova M et al. Scleroderma-like disorders. Autoimmun Rev. 2008 Feb;7(4):331-9. [ Links ]
8. Graze PR, Gale RP. Chronic graft versus host disease: a syndrome of disordered immunity. Am J Med. 1979;66:611-20. [ Links ]
9. Kier P, Penner E, Bakos S, Kalhs P, Lechner K, Volc-Platzer B et al. Autoantibodies in chronic GVHD: high prevalence of antinuclear antibodies. Bone Marrow Transpl. 1990;6:93-6. [ Links ]
10. Parkman R. Chronic graft-versus-host disease. Current Opin Hematol. 1998;5:22-5. [ Links ]
11. Pereira CM, Almeida OP, Correa MEP, Souza CA, Barjas-Castro ML. Oral involvement in chronic graft versus host disease: a prospective study of 19 Brazilian patients. Gen Dent. 2007;55(1):48-51. [ Links ]
12. Redding SW, Callander NS, Haveman CW, Leonard DL. Treatment of oral chronic graft-versus-host disease with PUVA therapy: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:183-7. [ Links ]
13. Schubert MM, Sullivan KM, Izutsu KT, Peterson DE, Flournoy N, Truelove EL et al. Oral complications of bone marrow transplantation. In: Peterson DE, Sonis ST, editors. Oral complications of cancer chemotherapy. Boston: Martinus Nijhoff; 1983. p. 93-112. [ Links ]
14. Schubert MM, Sullivan KM, Morton TH, Izutsu KT, Peterson DE, Flournoy N et al. Oral manifestations of chronic graft-v-host disease. Arch Intern Med. 1984;144:1591-5. [ Links ]
 Corresponding author:
Corresponding author:
Claudio Maranhão Pereira
School of Dentistry of Paulista University, Brasília campus
Dentistry coordination
SGAS Quadra 913, s/n.º – Conjunto B – Asa Sul
Zip code 70390-130 – Brasília – DF
E-mails: odontologiabrasilia@unip.br / claudiomaranhao@hotmail.com
Received for publication: October 4, 2010.
Accepted for publication: November 3, 2010.













