Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.8 no.3 Joinville Jul./Set. 2011
CASE REPORT ARTICLE
Oral lymphangioma: case report
Marcelo Gadelha VasconcelosI; Bruna Câmara SantosII; Luciana Cristina Peixoto LemosII; Betania Fachetti RibeiroIII; Déborah Pitta Paraíso IglesiasI; Rodrigo Gadelha VasconcelosI; Ana Myriam Costa de MedeirosI
I Program of Post-Graduation in Dentistry, Federal University of Rio Grande do Norte – Natal – RN – Brazil
II School of Dentistry, Federal University of Rio Grande do Norte – Natal – RN – Brazil
III Program of Post-Graduation in Dentistry, Federal University of Paraiba – Joao Pessoa – PB – Brazil
ABSTRACT
Introduction: Lymphangioma is a change of lymphatic vessels that frequently affects the head and neck region. Its occurrence at oral cavity is rare and it is most commonly identified at the anterior two-thirds of the tongue. At this location, it is clinically characterized as transparent and generally grouped vesicles, which can be red or purple. The deep lesions appear as nodular masses of variable color and superficial texture. It can be classified according to the size of vessels into three types: capillary, cavernous, and cystic lymphangioma. Several types of treatment have been suggested; and the most commonly used treatments are: surgical excision, application of carbon dioxide laser, cryotherapy using liquid nitrogen, and sclerosing agents. Objective and case report: To describe a case of oral lymphangioma diagnosed in a 17-year-old female patient. The lesion was presented as multiple vesicles of soft consistency with thin epithelial lining and color ranging from translucent to yellow-reddish, involving the soft palate and the left retromolar region. Incisional biopsy confirmed the hypothesis of cavernous lymphangioma. Patient was followed-up for one year without signs of lesion relapse. Conclusion: Through this clinical case report and literature review, this study emphasizes the relevance of the clinical and histopathological features that should be considered to confirm the clinical hypothesis and indicate the proper therapeutic for oral lymphangiomas.
Keywords: lymphangioma; pathology; lymphatic vessels.
Introduction
Lymphangioma is a benign hamartomatous tumor of lymphatic channels, with a marked predilection for the head and neck region, at submandibular and parotid area 2,10. Approximately half of the cases are present since birth, and about 90% is developed before 2 years old; it is rarely diagnosed in adults 11. The lesion is classified according to the vessels diameter into: capillary or microcystic, cavernous or macrocystic, and cystic or hygroma lymphangioma 7,13.
At oral cavity, it presents a rare occurrence, and it is more frequently located at the anterior two-thirds of the tongue; although cases in palate, gingiva, jugal mucosa, lips, and mandibular alveolar ridge have already been described 2,5,12. Clinically, its location is superficial, seen as transparent and generally grouped vesicles, which can be red or purple due to secondary hemorrhages. The deep lesions appear clinically as nodular masses of variable color and superficial texture 13.
There are several therapeutic modalities for the treatment of oral lymphangioma. Surgical excision is mostly indicated when vital structures are not involved 7,8. Other treatments include the use of sclerosing agents, application of carbon dioxide laser and liquid nitrogen cryotherapy. However, studies have evidenced that such methods are not very efficient due to the possibility of lesion relapse 3,7,8.
The aim of this study was to report a case of lymphangioma in oral cavity treated by surgical incision as well as to compare the clinical-pathological data found with the information described in literature.
Case report
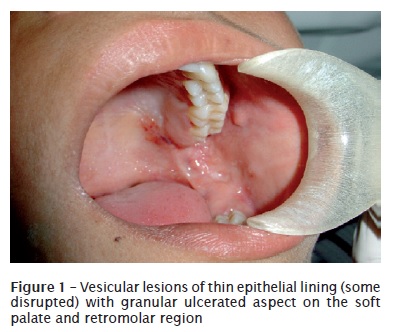
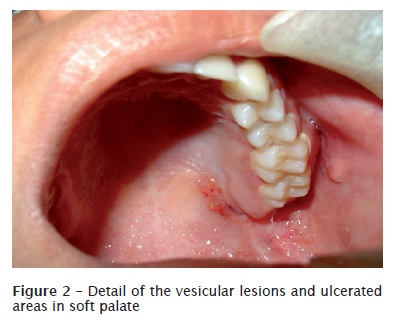
A 17-year-old female patient, brown skin, was referred to the Clinic of Stomatology of the School of Dentistry of the Federal University of Rio Grande do Norte, complaining about blisters within oral cavity for one year, which disrupted during feeding and were related commonly to episodes of bleeding. At clinical intraoral examination, we observed exophytic vesicular lesions with thin epithelial lining and color ranging from translucent to yellow-reddish, of soft consistency and sessile insertion, giving to the epithelial surface a granular aspect (figures 1 and 2). Clinically, such lesion was diagnosed as lymphangioma and hemangyoma.
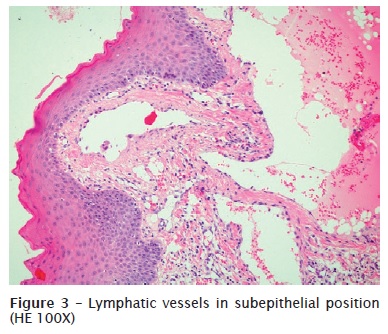
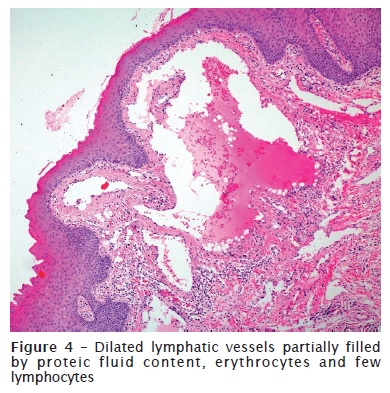
To confirm the diagnosis, an incisional biopsy was executed, and the sample was referred to the Service of Pathological Anatomy of the Discipline of Oral Pathology of the Federal University of Rio Grande do Norte for anatomopathological examination. The histological cuts were examined and stained in hematoxylin and eosin (HE), revealing lymphatic vessels of great diameter distributed in a conjunctive tissue poorly organized. Such vessels were mainly located at subepithelial position, occupying the lamina propria, and presented lumens partially filled by proteic fluid content, erythrocytes, and few lymphocytes (figures 3 and 4). Therefore, the histopathological diagnosis confirmed the clinical and surgical hypothesis of lymphangioma.
Patient was submitted to surgical treatment for lesion enucleation. The procedure was facilitated due to the superficial location of the lymphatic vessels. After 1 year of following-up, we did not observe the lesion relapse.
Discussion
Lymphangiomas are vascular malformations. It is hypothesized that they develop from congenital obstruction or sequestration of the primitive lymphatic cells that present proliferative capacity and are commonly capable of accumulating fluids, which give to them a cystic appearance. Because these cells do not anastomose efficiently with bigger lymphatic vessels, they then provoke areas of lymphatic blockage 4,10.
These lesions comprises about 30% of the lesions of lymphatic vessel origin and present markedly prediction by the neck and head area and common at the cervical region, mainly at the posterior triangle of the neck (upper middle third of clavicle, anterior edge of trapezius muscle, posterior border of sternocleidomastoid) 1. The anterior triangle may also be involved and the submandibular and parotid regions are the more commonly associated areas to lymphangioma development 2,8. The lesions have been reported in several organs, and only 1% occurs in the gastrointestinal tract 6.
Oral cavity rarely represents an occurrence site. When oral cavity is affected, the most prevalent site is the tongue, mostly restricted to its anterior third; but the lesions can be extended and involve great extensions of the tongue 1,6. Brennan et al. 3 revised 49 cases of oral lymphangioma and found that 17 were located in tongue, while only one case was described at retromolar region and one at soft palate. Therefore, the case described here shows an uncommon site of oral lymphangioma 2,5, involving the retromolar region, extending to the soft palate.
Lymphangioma is observed since birth or is manifested before 2 years of age; consequently, these lesions diagnosis is rarely performed in adult patients 8. In the case reported here, the lesion developed in a patient older than the common age group, who had 17 years-old at the moment of the diagnosis and had reported that the problem persisted by at least one year.
Clinically, oral lymphangioma is manifested as clear vesicles giving the mucosa a granular aspect. Such vesicles, which normally present a translucent aspect due to the superficial location of the lymphatic vessels, may occasionally assume a red or blue aspect because of the rupture of blood capillary into the lymphatic inner spaces 6,10,13. In this case, the clinical lesions appearance is in agreement with the form classically described for oral lymphangiomas: grouped translucent vesicles with some presenting reddish color. It was observed that the vesicles characterizing the granular aspect of the jugal mucosa surface sometimes were disrupted, conferring the mixed aspect (ulcerated and vesiculous) to the lesion. In some cases the rupture of great part of the vesicles can determine whether the lymphangioma would be clinically manifested as a predominantly ulcerated lesion 6.
The deep lesions generally are shown as masses of diffuse growth, which depending on the anatomical location may determine damages such as tissue swelling, obstruction of upper airways, pain, tongue's extrusion, sialorrhea, deformity of jaws, as well as difficulties in mastication, speech, and during oral hygiene 6,7. Some reports described that lymphangiomas assume great proportions and can measure 14 cm. Often, the fast growth of the lesion occurs due to the association with a secondary tumor or an infection in the respiratory tract, which determine an increase of the lymph production, blockage of the lymphatic drainage or infection due to the tumor 10.
Contrastively, in this case, the lesions were located more superficially and demonstrated well-defined limits, which normally, according to Leboulanger et al. 7, are not associated to discomfort related to the lesion. Despite of the asymptomatic feature described by the patient, the lesion was associated with bleeding episodes perceived during and/or after the meals. Therefore, the presence of secondary hemorrhage inside some lymphatic spaces accounted for the purple vesicles, which can be misplaced by hemangioma 10. Lymphangiomas are classified into three types: simple (capillary or microcystic), composed of small vessels as capillaries; cavernous (macrocystic), comprising great and dilated lymphatic vessels which often become macroscopically visible, and cystic (hygroma cystic), in which the vessels occupy great cystic spaces, commonly greater than 1 cm 7,13.
In oral cavity, the dense conjunctive tissue and the presence of the skeletal muscles do not allowed the vessels great expansion. Consequently, the most common intraoral type is cavernous lymphangioma 9. Notwithstanding, because one lesion can display the three aforementioned vessel diameters, this classification is not routinely applied 10.
The microscopic examination of the histological cuts stained in HE found the presence of vascular spaces exhibiting a thin endothelial lining with a single cell layer. This finding corroborated the descriptions of Yaita et al. 14. The authors still added that these vessels did not present an external layer of smooth muscle cells and the immunohistochemical profile demonstrate a weak expression for CD-1 and strong expression for D2-40, a marker to be used in cases which the differential diagnosis with blood vessels is necessary. In this case, such lymphatic vessels presented great lumens partially filled by proteic fluid material, erythrocytes and few lymphocytes. The preferential location of these vessels was lamina propria, projecting on the oral mucosa epithelium, compatible with either the translucent or red vesicles, clinically identified 10,14. Areas of epithelial discontinuity corroborate the clinical findings of ulceration, previously described.
While multiple therapeutic modalities have been described for the treatment of deep lymphangiomas, such as surgical excision, cryotherapy, electrocauterization, eschlerotherapy, steroids administration, embolization, and laser therapy 14, surgical excision has been the best alternative for lesions presenting localized growth 2,6. Because the lesions described in this case report exhibited a superficial location, we opted for their surgical removal. After one year of follow-up, no sign of lesion relapse was identified.
Conclusion
Oral lymphangiomas are uncommon lesions occurring at the dorsal region of the tongue, and rarely at the retromolar and soft palate area. Superficial and localized lesions can be treated by conservative surgical excision with low relapse rates. Therefore, this condition knowledge is of fundamental importance for its correct diagnosis and proper therapeutic indication.
References
1. Best SR, Coelho DH, Ahrens WA, Atez G, Sasaki CT. Laser excision of multiple esophageal lymphangiomas: a case report and review of the literature. Auris Nasus Larynx. 2008 Jun;35(2):300-3. [ Links ]
2. Bozkaya S, Ugar D, Karaca I, Ceylan A, Uslu S, Baris E et al. The treatment of lymphangioma in the buccal mucosa by radiofrequency ablation: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Nov;102(5):e28-31.
3. Brennan TD, Miller AS, Chen S. Lymphangiomas of the oral cavity: a clinicopathologic, immunohistochemical, and electron-microscopic study. J Oral Maxillofac Surg. 1997 Sep;55(9):932-5.
4. Huang HY, Ho CC, Huang PH, Hsu SM. Coexpression of VEGF-C and its receptors, VEGFR-2 and VEGFR-3, in endothelial cells of lymphangioma. Implication in autocrine or paracrine regulation of lymphangioma. Lab Invest. 2001 Dec;81(12):1729-34.
5. Iamaroon A, Pongsiriwet S, Srisuwan S, Krisanaprakornkit S. Lymphangioma of the tongue. Int J Paediatr Dent. 2003 Jan;13(1):62-3.
6. Jian XC. Surgical management of lymphangiomatous or lymphangiohemangiomatous macroglossia. J Oral Maxillofac Surg. 2005 Jan;63(1):14-9.
7. Leboulanger N, Roger G, Caze A, Enjolras O, Denoyelle F, Garabedian E. Utility of radiofrequency ablation for haemorrhagic lingual lymphangioma. Int J Pediatr Otorhinolaryngol 2008 Jul;72(7):953-8.
8. Mandel L. Parotid area lymphangioma in an adult: case report. J Oral Maxillofac Surg. 2004 Oct;62(10):1320-3.
9. Mosca RC, Pereira GA, Mantesso A. Cystic hygroma: characterization by computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 May;105(5):e65-9.
10. Neville BW, Damm DD, Allen CM, Bouquot JE. Tumores dos tecidos moles. In: Patologia oral e maxilofacial. 3. ed. Rio de Janeiro: Elsevier; 2009. p. 509-72.
11. Queiroz AM, Silva RA, Margato LC, Nelson-Filho P. Dental care manegement of a young patiet with extensive lymphangioma of the tongue: a case report. Spec Care Dentist. 2006 Jan-Feb;26(1):20-4.
12. Stănescu L, Georgescu EF, Simionescu C, Georgescu I. Lymphangioma of the oral cavity. Rom J Morphol Embryology. 2006;47(4):373-7.
13. Weiss SW, Goldblum JR. Tumors of lymph vessels. In: Soft tissue tumors. 4. ed. St. Luis: Mosby; 2001. p 955-67.
14. Yaita T, Onodera K, Xu H, Ooya K. Histomorphometrical study in cavernous lymphangioma of the tongue. Oral Dis. 2007 Jan;13(1):99-104.
 Correspondence:
Correspondence:
Marcelo Gadelha Vasconcelos
Avenida Praia dos Búzios, n. 9067 – Ponta Negra
CEP 59092-200 – Natal – RN – Brasil
E-mail: marcelo.vasconcelos@yahoo.com.br
Received for publication: September 28, 2010
Accepted for publication: December 6, 2010













