Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.8 no.3 Joinville Jul./Set. 2011
CASE REPORT ARTICLE
Subepithelial connective tissue graft: a case report
Juliana Alcarás SaraivaI; Edson Alves de CamposI; Rodrigo CavassimII; Shelon Cristina de Souza PintoII; Lucas Amaral FontanariII; Guilherme José Pimentel Lopes OliveiraII; José Eduardo Cezar SampaioII
I Department of Operative Dentistry, Sao Paulo State University – Araraquara – SP – Brazil
II Department of Diagnosis and Surgery, Sao Paulo State University – Araraquara – SP – Brazil
ABSTRACT
Introduction and objective: Marginal tissue recession represents a common condition in Periodontology. Miller's Classes I and II recessions, in which the etiological factors are well diagnosed and eliminated, show great predictability of total coverage when the technique of subepithelial connective tissue graft is used. This technique success has been mainly attributed to the double blood supply for graft's nutrition, originating from the connective tissue of both the periosteum and flap. Case report and conclusion: The authors reported a clinical case in which a Miller's Class I recession was treated by the surgical technique of subepithelial connective tissue graft, obtaining total coverage, eliminating the aesthetic deficiency and the dentin hypersensitivity complained by patient.
Keywords: subepithelial connective tissue graft; marginal tissue recession; root coverage.
Introduction
Marginal tissue recession is a common condition in Periodontology and is characterized by the displacement of the gingival margin towards to the mucogingival junction with root surface exposure; it may occur at isolated or multiple areas of oral cavity with different extension degrees 14. Today, "marginal tissue recession" has been the most accepted term, because the tissue showing the problem can be the alveolar mucosa instead of the gingiva 18.
Several etiological factors may account for the recessions' appearance, such as traumatic toothbrushing, tooth malpositioning, periodontal disease, frenum and bridle insertions, occlusal trauma, restoration with subgengival overhanging margins, maladapted crowns, extractions of adjacent teeth, orthodontic movement, iatrogenic factors and bone dehiscences 4. A more detailed analysis of such agents shows that most of them present a common feature: gingival inflammation 8.
When present, marginal tissue recessions may implicate in compromising the patient's periodontal health, aesthetic, and comfort. Concerning to periodontal health, the recessions are capable of acting as a local modifying factor for the installation and progression of periodontal disease, because an alteration in the normal gingival contour (regular concave arch) occurs, which collaborates for greater bacterial plaque accumulation 8. This alteration also contributes for an unfavorable aesthetics. Finally, the recessions may compromise the patient's comfort due to the possibility of cervical dentinal hypersensibility occurrence after the root surface exposure to oral cavity 11.
The surgical treatment is an alternative to obtain patient's aesthetic, diminish or eliminate dentinal hypersensibility and allow better conditions of dental hygiene performance in the affected area. Subepithelial conjunctive tissue graft is the surgical technique mostly studied and presents the most predictability of root coverage; however, the evaluation of factors such as defect's width and height and condition of interproximal gingival and bone tissue are determinant to reach a good prognosis 18.
In 1985, Miller 14 established the clinical classification of marginal tissue recessions: class I – the recession does not reach the mucogingival junction without loss of interproximal tissue; class II – the recession reaches or surpasses the mucogingival junction without loss of interproximal tissue; class III – loss of interproximal tissue is seen and the proximal gingival tissue is apically to the enamel-cementum junction and coronally to the recession; class IV – proximal gingival tissue is at the recession base level. The higher the periodontal tissue loss (Miller's class III and IV), the worse the prognosis related to root coverage amount obtained after surgery.
The aim of this study is to describe a case report using subepithelial conjunctive tissue graft, as well as to show the technique's success predictability when well indicated.
Case report
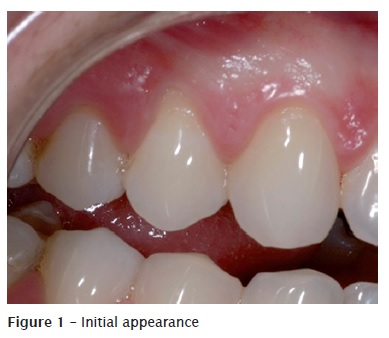
Patient J. A. S., 22 years-old, female, leucoderm, systemically health, non-smoking, presented as chief complaints the esthetic deficiency at tooth #14 (figure 1) and dentinal hypersensibility in this same tooth.
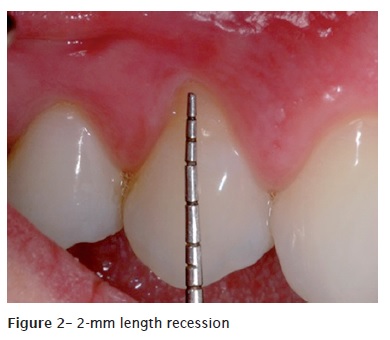
After anamnesis, the probable etiological factors were defined as traumatic toothbrushing and orthodontic movement. Clinically, the tooth presented a marginal tissue recession of about 2 mm length, with lack of probing depth greater than 2 mm (figure 2). Therefore, the recession was classified as Miller's class I and, then, root coverage by subepithelial conjunctive tissue graft was indicated.
Antisepsis was carried out through aqueous solution of 0.12% chlorhexidine digluconate. After local anesthesia with 2% mepivacaine with adrenaline (Mepiadre, DFL, Rio de Janeiro, Brazil), scaling and root planing were executed on tooth #14 (figure 3). Scaling procedure is necessary to remove the contaminated and exposed cementum.

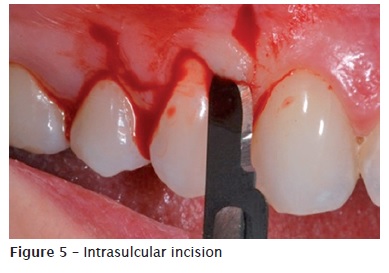
Then, preparation of the receptor site was performed through horizontal incisions, towards enamel-cementum junction direction, at each papilla (figure 4). Following, two vertical relaxing incisions and one intrasulcular incision were executed (figure 5). Next, full-thickness flap was raised, up to the mucogingival junction and continued as a partial-thickness flap based on this junction. Later, the papilla's epithelium was coronally removed up to their apexes.

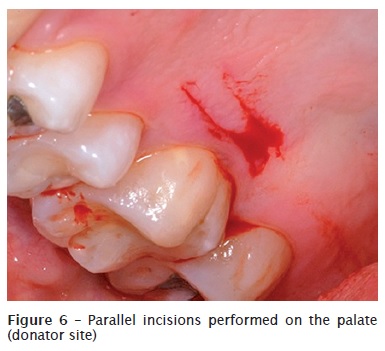
After preparing the receptor site, we obtained the subepithelial conjunctive tissue graft from the palate, through the technique of two parallel incisions: one perpendicular to the tooth axis and the other parallel to the bone surface, deepening up to the desired graft height (figure 6).
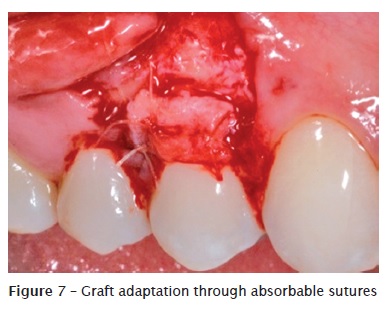
The graft was adapted onto the donator site (figure 7) through sutures with absorbable thread (5-0 Vicryl, J&J Ethicon, USA).
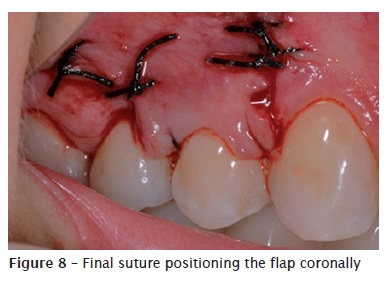
A suspensory suture was performed (silk thread 4-0, J&J Ethicon, USA), aiming to position the flap coronally onto the graft (figure 8) to improve therefore the graft's stabilization and nutrition on the receptor site. Also, complementary sutures were executed.

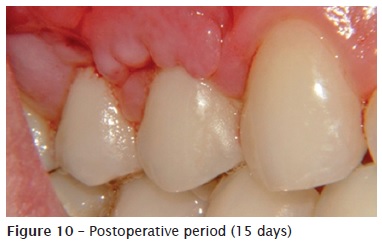
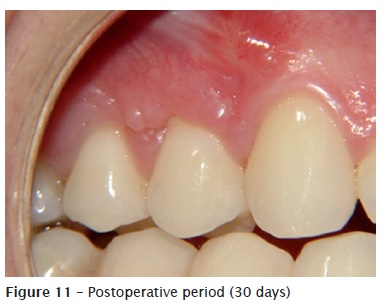
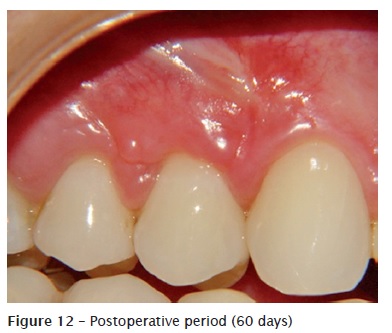
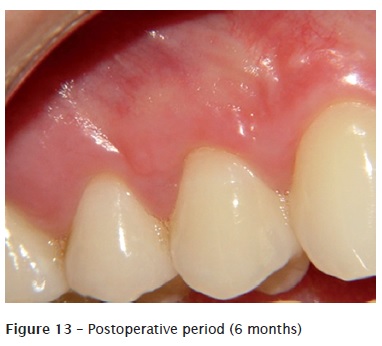
At postoperative period, patient was oriented to use aqueous 0.12% chlorhexidine digluconate mouthrinse for 10 days, and analgesics for pain. Sutures were removed 7 days post-surgery. At 15, 30, and 60 days, as well as 6 months and 1 year, patient's follow-up was performed by radiographs, in which were seen a good root coverage and significant aesthetic improvement (figures 10, 11, 12, 13, and 14).

Discussion
Several mucogingival techniques have been introduced in literature aiming to correct marginal tissue recessions 19. During the decades of 1960s and 70s, the most used techniques were coronally positioned flap 1, laterally displaced flap 9, and the combination of coronally positioned flap with free gingival graft 2. At the beginning of the decade of 1980s, the use of subepithelial conjunctive tissue graft was disseminated, assuring the obtainment of excellent results in areas with localized root exposure 13.
The choice of the adequate technique and the long-term success of the procedure depend on the careful evaluation of the defect type, recession's etiology, operator's ability, presence of keratinized tissue, tissue width, predictability, single or multiple gingival recessions, healing, aesthetic result, and risk factors 15.
Subepithelial connective tissue graft can be indicated for the treatment of single or multiple gingival recessions, correction of the papilla's volume or deformities of the edentulous gingival border, creation and/or increasing of the amount of the keratinized mucosa 1, and perspective improvement of the root coverage associated with restorative procedures, abrasion, or dental caries 17.
In 1985, Langer and Langer 13 described a technique of subepithelial conjunctive tissue graft for root coverage in the treatment of recessions at single or multiple areas, attributing the procedure success to the double blood supply for the graft's nutrition, originating from the connective tissue of both the periosteum and flap. Additionally, this aforementioned technique is less invasive at the palatal area, causing a minimum postoperative discomfort to patient and offering a great predictability of coverage. Consequently, this technique is the first choice in cases needing good aesthetical outcomes, as the case reported here. Notwithstanding, this methodology also exhibit disadvantages: need of a greater amount of tissue than the required for covering the area due to the contraction suffered by the tissue, from the surgery to its functional incorporation within the receptor site 7; and difficulty of standardization of the graft thickness, which may result in aesthetical alterations 3. Accordingly, these aspects must be observed during the surgical procedure.
In this case report, full-thickness flap up to the mucogingival junction in the receptor site was performed attempting to avoid this bone loss. A partial-thickness flap may implicate in perforation, capable of resulting in flap necrosis, and consequently in bone tissue loss 6. Furthermore, in partial-thickness flaps, the presence of the highly vascularized tissues adjacent to the root surface may be a necessary condition for root resorption 12. According to Harris 10, the desired results after the surgical procedure are: root coverage up to the enamel-cementum junction, tissue firmly attached to the tooth with sulcular probing depth smaller than 2 mm, absence of bleeding on probing, presence of an adequate keratinized tissue, color similar to the adjacent tissues, tissue's aesthetical contour, and decreasing of the sensibility reported by the patient.
Special attention should be given concerning to subepithelial conjunctive tissue graft indication in cases of Miller's class III and IV marginal tissue recession. The aforementioned technique presents less predictability of root coverage in such recessions, because of the difficulty of graft's adaptation and nutrition which may result in necrosis 16.
Conclusion
The success of this clinical case may be attributed to the precise indication of the technique of subepithelial conjunctive tissue graft due to the high predictability of root coverage in Miller's class I and II and the double blood supply for the graft's nutrition.
References
1. Bernimoulin JP, Luscher B, Muhlemann HR. Coronally repositioned periodontal flap. Clinical evaluation after one year. J Clin Periodontol. 1975;2(1):1-13. [ Links ]
2. Caffesse RG, Guinard EA. Treatment of localized gingival recessions. Part II. Coronally repositioned flap with a free gingival graft. J Periodontol. 1978;49(7):357-61.
3. Callan DP, Silverstein LH. Use of acellular dermal matrix for increasing keratinized tissue around teeth and implants. Pract Periodontics Aesthet Dent. 1998;10(6):731-4.
4. Cardoso RJA, Gonçalves EA. In: Proceedings of the 20th Congresso Internacional de Odontologia; 2002. São Paulo: Artes Médicas; 2002. p. 201-48.
5. Duarte AC. Cirurgia periodontal pré-protética e estética. São Paulo: Santos; 2002. p. 3-19.
6. Edel A. Clinical evaluation of free connective tissue grafts used to increase the width of keratinised gingiva. J Clin Periodontol. 1974;1(4):185-96.
7. Edel A. The use of a free connective tissue graft to increase the width of attached gingiva. Oral Surg Oral Med Oral Pathol. 1975;39(3):341-6.
8. Fontanari LA, Rodrigues MR, Scremin EI, Kitano MSI, Sampaio JEC, Trevisan Júnior W. Enxerto de tecido conjuntivo subepitelial: uma alternativa em cirurgia plástica periodontal. Perionews. 2009;3(2):131-5.
9. Guinard EA, Caffesse RG. Treatment of localized gingival recessions. Part I. Lateral sliding flap. J Periodontol. 1978;49(7):351-6.
10. Harris RJ. The connective tissue and partial thickness double pedicle graft: a predictable method of obtaining root coverage. J Periodontol. 1992;63(5):477-86.
11. Holbrook T, Ochsenbein C. Complete coverage of the denuded root surface with a one-stage gingival graft. Int J Periodontics Restorative Dent. 1983;3(3):8-27.
12. Hokett SD, Peacock ME, Burns WT, Swiec GD, Cuenin MF. External root resorption following partial-thickness connective tissue graft placement: a case report. J Periodontol. 2002;73(3):334-9.
13. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56(12):715-20.
14. Miller Jr. PD. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5(2):8-13.
15. Ottoni J, Magalhães LF. Cirurgia plástica periodontal e periimplantar: beleza com proporção e harmonia. São Paulo: Artes Médicas; 2006. 440 p.
16. Polson AM. Periodontal regeneration: current status and direction. Hong Kong: Quintessence Books; 1994. p. 53-70.
17. Nevins M, Melloning JT. Periodontal therapy: clinical approaches and evidence of success. Tokyo: Quintessence; 1998. p. 355-64.
18. Steffens JP, Santos FA, Pilatti GL. Cirurgias mucogengivais para recobrimento radicular: o enxerto de conjuntivo subepitelial como técnica de sucesso para defeitos isolados. Dental Science. 2008;2(7):207-14.
19. Wennstrom JL. Mucogingival therapy. Ann Periodontol. 1996;1(1):671-701.
 Correspondence:
Correspondence:
Juliana Alcarás Saraiva
Rua Humaitá, n. 1.740, apto. 52 – Centro
CEP 14801-385 – Araraquara – SP – Brasil
E-mail: julialcaras@yahoo.com.br
Received for publication: December 15, 2010
Accepted for publication: February 2, 2011













