Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.8 no.4 Joinville Out./Dez. 2011
ORIGINAL RESEARCH ARTICLE
Epidemiology of maxillofacial injuries at a regional hospital in Goiania, Brazil, between 2008 and 2010
Cláudio Maranhão PereiraI; Mauro Silva FilhoII; Danilo Santos CarneiroII; Renan Correia ArcanjoII; Leonardo Araújo de AndradeIII; Michelle Gomes Benício de AraújoIII
I School of Dentistry, Paulista University, and Estácio de Sá University – Goiania – GO – Brasilia – DF – Brazil
II School of Dentistry, Paulista University – Goiania – GO – Brazil
III Buccomaxillofacial Surgery and Traumatology Service of the "Hospital Cidade Jardim" – Goiania – GO – Brazil
ABSTRACT
Introduction and objective: Facial lesions assume an outstanding role in the attendance of polytraumatized patients in hospital emergency services. The aim of this study was to conduct and epidemiologic study of patients attended at the Buccomaxillofacial Surgery and Traumatology Service of a regional hospital in Goiania/GO, Brazil, between 2008 and 2010. Material and methods: 521 files of patients, who had suffered maxillofacial traumatisms that resulted in a total of 615 fractures, were evaluated. The files were used to analyze gender, age, etiologic agents and distribution of fractured bones. Results: About 80% of patients were male, whereas 20% of the affected individuals were women. The most frequently etiologic factor found in the two groups was automobile accidents, followed by physical aggressions and falls. Concerning to fractured bones, the zygomatic complex, followed by fractures of the mandible, the nasal bones themselves, condyle and Le Fort type fractures were the most prevalent ones, in both groups. Conclusion: Knowledge of the incidence and etiology of maxillofacial fractures is of great importance to the professionals involved in the treatment of these patients. Within this context, Buccomaxillofacial Surgery and Traumatology is increasingly being affirmed as one of the most important specialties at the emergency centers of regional hospitals concerning to the treatment of patients who are victims of traumatisms.
Keywords: maxillofacial injuries; trauma centers; craniocerebral; trauma, head and neck.
Introduction
Facial traumatism is the greatest threat to public health and the main cause of death in the first 40 years of life in the United States 2,7. Among trauma victims, cranio-maxillofacial lesions affect a significant number of patients. These lesions may occur in isolation or in combination with other injuries, and may include lesions of the cranium, spine, and of the upper and lower members 2,6,8,12,17.
Many authors have affirmed that the approach to maxillofacial traumatism should include: treatment of the facial bone fractures, dento-alveolar trauma and soft tissue lesions, as well as head and neck injuries and those associated with the thorax and abdomen 9. This demands the integration of a specialist in facial traumatology into multidisciplinary teams in order to promote effective attendance 3.
The causes of injuries and maxillofacial fractures have changed over the last three decades. Recent international studies have pointed out the main causes as being traffic accidents, aggressions, falls, domestic and industrial accidents, lesions related to sporting practices and urban violence 6,7,8.
Understanding of the cause, severity and temporal distribution of maxillofacial traumas may help to establish clinical priorities for the effective treatment and prevention of these injuries. Epidemiology may and should be used for the purposes of administrating health services. It contributes to establish the diagnosis of the presence, nature and distribution of health and disease in a community 7.
Facial lesions, among which fractures are included, assume an outstanding role in the attendance of polytraumatized patients at hospital emergency services. Studies conducted with the intention of outlining the epidemiological profile of facial traumatisms worldwide have correlated the social urban and rural changes as modifying agents of interpersonal relationships, generating actions of physical violence, both of a personal and group nature, and are represented by physical aggressions, violence in traffic, domestic violence and violence against women 5.
Therefore, the objective of this study was to trace the profile of maxillofacial trauma victims who sought attendance and were hospitalized at a regional hospital – "Hospital Regional Cidade Jardim" (HRCJ), at the city of Goiania (GO), Brazil, from 2008 to 2010.
Material and methods
Five hundred and twenty-one (521) files of patients with maxillofacial traumatisms attended in the period from January 01, 2008 to November 30, 2010 (35 months) at the Buccomaxillofacial Surgery and Traumatology Service of HRCJ were individually studied. The files were obtained from the Medical Archives Sector, after obtaining previously authorization. Gender, etiologic agents and the distribution of fractured bones were analyzed. After data collection and analysis, the results were submitted to descriptive statistical treatment and distributed into tables and graphs.
The research was submitted to and approved by the Ethics Committee in Research of the Medical Science Institute of the Paulista University.
Results
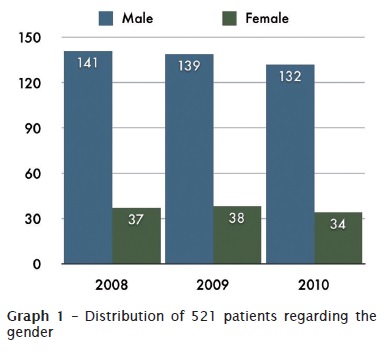
Of the 521 patients analyzed in this research, 412 were men (79.07%) and 109 women (20.92%), as shown in graph 1.
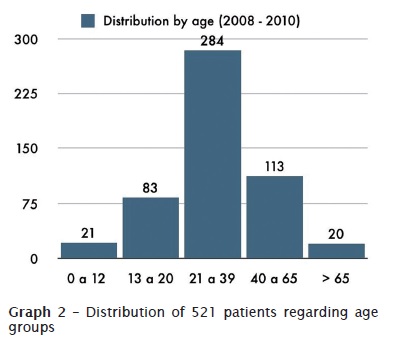
The patients were distributed into five age groups, with age-range between 2 and 73 years. The group with the highest rate of incidence was the one from 21 to 39 years of age (graph 2).
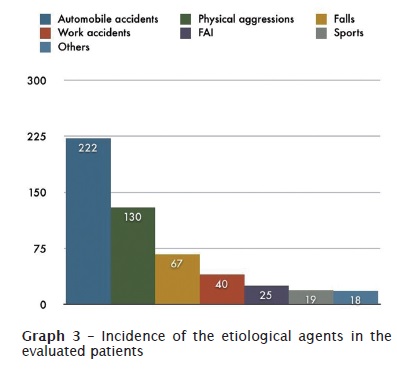
As regards the etiological agents, these were classified into automobile accidents, physical aggressions (interpersonal aggressions by punching and/or kicking), falls (falls from the person's own height or higher), work accidents, firearm-related injuries (FAI), accidents during sports practice and other causes. The automobile accidents prevailed, with a rate of 39% of the cases, followed by physical aggression (26%), falls (14%), work accidents (9%), FAI (6%), sporting accidents (4%) and others (3%). Graph 3 shows the aforementioned distribution, however, in absolute numbers. Automobile accidents totalized a number of 222 cases, followed by physical aggression (130), falls (67), work accidents (40), FAI (25), sporting accidents (19) and others (18).
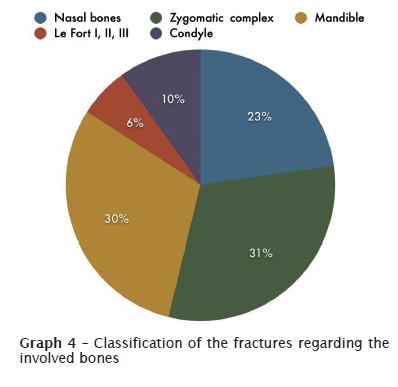
Finally, fractures were classified according to the bones affected. In the analysis of the 521 files, 615 fractures were found. Traumatisms of the zygomatic complex were the most frequent, totalizing a number of 191 cases (31%). Ranked immediately after this were fractures of the mandible, with 186 cases (30%); nasal bone fractures totaled 140 cases (23%); condylar fractures, with 61 cases (10%); and in 37 cases (6%), Le Fort type fractures were observed. The fracture rates in percentages are shown in graph 4.
Discussion
Epidemiologic studies of facial traumatisms have been well described in world literature. The results of cause and incidence tend to vary according to the geographic region, socioeconomic, cultural, religious and time factors 6,7,10,13.
Literature is practically unanimous as regards the fact that among the various surgical modalities attended, patients with facial traumatism are preponderantly young adults, in the age-range between 10 and 40 years of age 14. The predominance of men in this study is a finding similar to that of the majority of reports, which have also shown a lower incidence of maxillofacial traumatisms in women 11.
In literature, the main reason found for this male predominance results from men being more predisposed to risk factors, such as physical aggressions, automobile highway accidents, falls and accidents during sporting practice 11,10,13.
In Ontario, automobile accidents resulted in 70% of the facial injuries, followed by falls and intentional injuries (homicide / robberies) 10. In Osaka, traffic accidents caused 787 (52%) victims with facial fractures. The second most common cause was falling (16.6%), accompanied by robberies (15.5%) 13. Herein, among the main causes of attendance, automobile accidents accounted for 39%, followed by physical aggressions (26%) and by falls from the person's own height (14%).
Fractures of the zygomatic-orbital complex and mandibles were the most prevalent sites of location, affecting 31% and 30% of the sample, respectively; followed by fractures of the nasal bones themselves (23%). Although mandibular fractures were the most prevalent type, the present research differs from the reports due to the very similar proportion between fractures of the mandible and factures of the zygomatic-orbital complex, being in agreement with various studies 1.
The literature consulted showed a wide predominance of fractures of the mandible. The fact that, mandible is the anatomic region that has most exhibited a solution of continuity, is possibly explained because it is the only mobile bone of the face, thus being more vulnerable to receiving strong impacts and fracturing 4,5,15.
According to various authors, patients who are victims of facial traumatisms must receive adequate attention as early as possible in relation to the time when the lesion occurred 4,5,13. The success of treatment of facial traumatisms and the implementation of preventive measures are dependent on epidemiological evaluations in the long term 6,10,16.
Conclusion
Based on the results obtained and the literature researched, it was concluded that:
• Of the patient's files analyzed, there was a predominance of fractures in individuals of the male gender;
• The most frequent cause of traumatisms was automobile accidents;
• The most prevalent fractures in the Maxillofacial Complex, in decreasing order were fractures of the zygomatic complex, mandible, nose, condyle and maxilla (Le Fort).
References
1. Adebayo ET, Ajyke OS, Adekeye EO. Analysis of the pattern of maxillofacial fractures in Kaduna, Nigeria. Br J Oral Maxillofac Surg.2003;41:396-400. [ Links ]
2. Alvi A, Doherty T, Lewen G. Facial fractures and concomitant injuries in trauma patients. Laryngoscope. 2003;113:102-6.
3. Costa R, Silva JJ. Condutas de atendimento em pacientes com lesões de face. BCI. 1998;5(2):21-4.
4. Erol B, Tanrikulu R, Görgün B. Maxillofacial fractures. Analysis of demographic distribution and treatment 2901 patients (25 year experience). J Cranio Maxillofac Surg. 2004;32:308-13.
5. Falcão MFL, Leite Segundo AV, Silveira MMF. Estudo epidemiológico de 1758 fraturas faciais tratadas no Hospital da Restauração, Recife - PE.. Rev Cir Traumatol Buco-Maxilo-Fac. 2005;5(3):65-72.
6. Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H. Cranio-maxillofacial trauma: a 10 year review of 9543 cases with 21 067 injuries. J Cranio Maxillofac Surg. 2003;31:51-61.
7. Girotto JA, Mackenzie E, Fowler C, Redett R, Robertson B, Manson PN. Long-term physical impairment and functional outcomes after complex facial fractures. Plast Reconstr Surg. 2001;108:312-27.
8. Haug RH, Prather J, Indresano AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac. 1990;48:926-32.
9. Hausamen JE. The scientific development of maxillofacial surgery in the 20th century and an outlook into the future. J CranioMaxillofac Surg. 2001;29:221.
10. Hogg NJV, Stewart TC, Armstrong JEA, Girotti M. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma. 2000;49:425-32.
11. Hollier L, Grantcharova EP, Kattash M. Facial gunshot wounds; a 4 year experience. J Oral Maxillofac Surg. 2001;59:277-82.
12. Hussain K, Wijetunge DB, Grubnic S, Jackson IT. A comprehensive analysis of craniofacial trauma. J Trauma. 1994;36:34-47.
13. Iida S, Kogo M, Sugiura T, Mima T, Matsuya T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg. 2001;30:286-90.
14. Manski RJ, Moeller JF. Use of dental services.An analysis of visits, procedure and providers. J Am Dent Assoc. 2002;133:167-75.
15. Motamedi MHK. An assessment of maxillofacial fractures: a 5 – year study of 237 patients.J Oral Maxillofac Surg. 2003;61:61-4.
16. Mouzakes J, Koltai PJ, Kuhar S, Bernstein DS, Wing P, Salsberg E. The impact of airbags and seat belts on the incidence and severity of maxillofacial injuries in automobile accidents in New York State. Arch Otolaryngol – Head Neck Surg. 2001;127:1189-93.
17. Oikarinen KS. Clinical management of injuries to the maxilla, mandible, and alveolus. Dent Clin North Am. 1995;39:113-31.
 Correspondence:
Correspondence:
Cláudio Maranhão Pereira
Faculdade de Odontologia da Universidade Paulista, campus Brasília
Coordenação de Odontologia
SGAS Quadra 913, s/n.º – Conjunto B – Asa Sul
CEP 70390-130 – Brasília – DF – Brasil
E-mail: claudiomaranhao@hotmail.com
Received for publication: January 27, 2011
Accepted for publication: March 30, 2011













