Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.8 no.4 Joinville Out./Dez. 2011
ORIGINAL RESEARCH ARTICLE
Bond strength of self-adhesive resin cements to deep dentin
Rubens Nazareno GarciaI,II; Amanda Graziela Zattar RenzettiIII; Bernd Rainer SchaibleIV; Roland FrankenbergerV; Ulrich LohbauerVI; Luiz Carlos Machado MiguelII
I University of Itajaí Valley – Itajaí – SC – Brazil. Group of Research in Interdisciplinary Dentistry
II School of Dentistry, University of the Region of Joinville – Joinville – SC – Brazil. Group of Research in Dental Biomaterials
III Private practice – Joinville – SC – Brazil
IV Private practice – Bad Orb – Hessen – Germany
V Department of Operative Dentistry and Endodontics, Philipps University of Marburg – Marburg – Hessen – Germany
VI Department of Operative Dentistry and Periodontology, FAU Erlangen – Erlangen – Baviera – Germany
ABSTRACT
Introduction and objective: Self-adhesive resin cements are applied in only one clinical step whose technique is considered less sensitive and of easy handling. However, there is some concern relating to a reliable and effective bonding to tooth structure, particularly when dentin is involved. The aim of this study was to evaluate microtensile bond strength of self-adhesive resin cements to deep dentin as well as to discuss some concepts involving these materials. Material and methods: Twenty-eight freshly extracted third molars were used. Their crowns were sectioned using a diamond disc (Isomet) to obtain occlusal deep dentin flat surfaces. The teeth were randomly assigned to four groups (n = 7): RelyX ARC/3M ESPE conventional resin cement (Group 1), and three self-adhesive resin cements – RelyX U100/3M ESPE (Group 2), Set/SDI (Group 3) and Maxcem/Kerr (Group 4). The products were applied according to the manufacturer's instructions. Tetric EvoCeram (Ivoclar Vivadent) blocks were used to simulate indirect restorations that were cemented onto the dentin surfaces. These blocks were sandblasted with oxide aluminum before adhesive procedures. The samples were stored in distilled water at 37±2°C for one week. Following, the samples were prepared for microtensile bond strength tests, which were performed at a crosshead speed of 1.0 mm/min until failure. Tensile bond strength data were calculated and the results were statistically analyzed by two-way ANOVA and Tukey test (p < 0.05). Results: The means (SD) (in MPa) were – Group 1: 14.7a (5.7); Group 2: 7.5b (2.3); Group 3: 5.6b (2.1); and Group 4: 4.7b (1.4). ANOVA showed significant differences and Tukey test identified differences among groups. Group 1 showed the highest bond strength mean. Bond strength mean of the other self-adhesive resin cements to dentin did not show statistical difference among them. Conclusion: Self-adhesive resin cements showed lower bond strength to dentin than RelyX ARC conventional resin cement. The highest bond strength mean of RelyX ARC is related to its mechanism of action. However, the mechanism of action involved in self-adhesive resin cements seems to be effective for clinical use if a proper prosthetic dental preparation is observed.
Keywords: dentin; resin cements; tensile strength.
Introduction
With the currently advancements of adhesive Dentistry, resin cements played an important role both for Restorative Dentistry and Prosthodontics. These products have several advantages when compared to conventional powder/liquid cements: better retention, minimum solubility at oral environment, less microleakage, and acceptable biocompatibility 9,16. Additionally, these materials' potential of bonding to both substrates (tooth and restoration) favors tooth structure reinforcement and allows aesthetic treatment success 2,7.
According to Garcia et al. (2007) 6, currently, bond to dentin is obtained by surface pre-treatment with acid, followed by adhesive system application containing hydrophilic and hydrophobic components. These steps either remove or modify smear layer and demineralize dental surface to expose the collagen layer for resin monomer infiltration, consequently forming the hybrid layer 15.
Self-adhesive resin cements were launched into market aiming to simplify the clinical steps and diminish the sensibility of the previous technique comprising multiple steps 8. The material is directly applied onto tooth surface, without demanding any pre-treatment. Otherwise, it is normally necessary the crown or restoration pre-treatment. The smear layer is partially incorporated by the acid monomers which promote micromechanical retention to tooth structure; chemical retention may occur by the reaction between acid monomers and hydroxyapatite present in tooth hard tissues 3.
The aim of this study was to evaluate the microtensile bond strength of self-adhesive resin cements to deep dentin as well as to discuss some concepts involving these materials.
Material and methods
Twenty-eight freshly extracted human third molars were used and stored at -20°C for a month, after the approval of the Ethical Committee of Dental Clinic 1, Department of Operative Dentistry and Periodontology, Friedrich-Alexander-University Erlangen-Nuremberg (FAU), Erlangen, Germany. Their roots were removed with aid of a diamond disc (Isomet, Buehler, Evanstone, IL, USA) under refrigeration. In these conditions, their crowns were sectioned to obtain occlusal deep dentin flat surfaces (2 mm below enamel-dentin junction of the central groove).
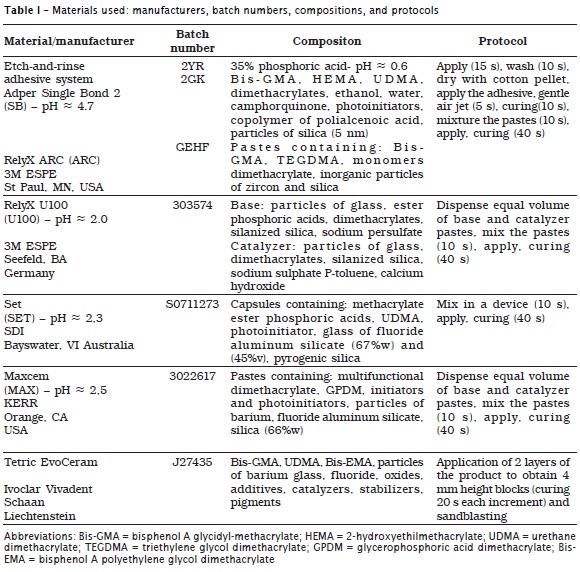
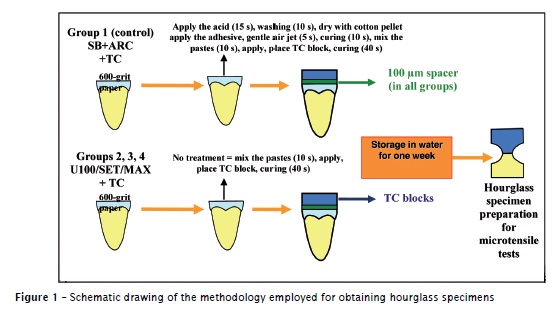
The teeth were randomly divided into four experimental groups (n = 7) and the products were used according to manufacturer's instructions: conventional resin cement (adhesive system – Adper Single Bond 2 + RelyX ARC/3M ESPE – group 1 / control) and three self-adhesive resin cements – RelyX U100/3M ESPE (group 2), Set/SDI (group 3) and Maxcem/Kerr (group 4) (table I). Blocks with 4 mm height were constructed with Tetric EvoCeram – TC (Ivoclar Vivadent) and their adhesive surfaces abraded with aluminum oxide (50 μm). Immediately prior to adhesive procedures, dentin samples underwent 600-grit silicon-carbide sandpaper to create fresh smear layer. To perform the luting procedures of the composite blocks on dentin samples, a 100 μm spacer was positioned at the samples lateral surfaces and all edges were light-cured for 20 seconds with Elipar Trilight (3M ESPE) halogen curing device, at power density of 750 mW/cm2.
Samples were stored in distilled water at 37±2°C for one week. Following, hourglass specimens were obtained for microtensile bond strength tests (figure 1) in a universal testing machine (Zwick Z 2.5, Ulm, Germany), at crosshead speed of 1.0 mm/min, until fracture.
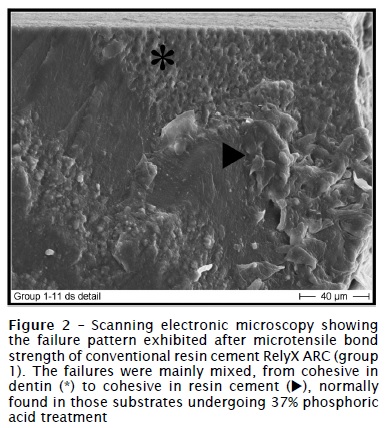
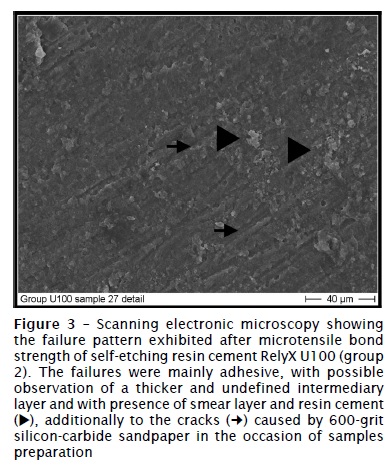
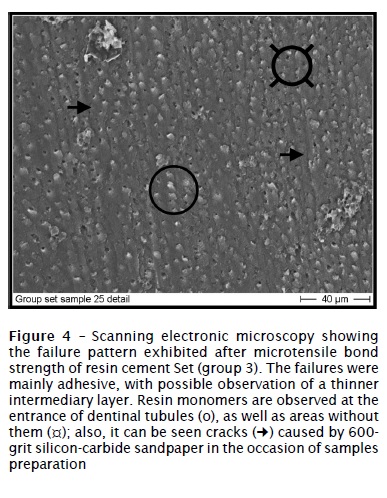
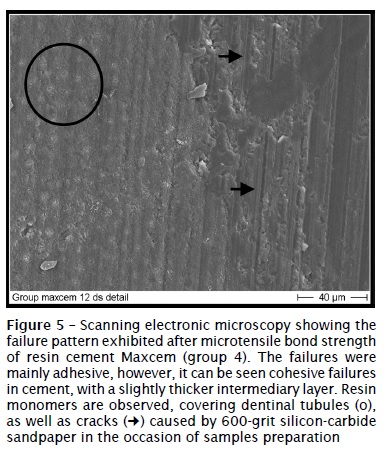
Bond strength data were calculated and analysed by two-way ANOVA and Tukey's test with level of significance set at 5% (p < 0.05). The specimens were mounted into an aluminum base, metalized with gold and examined in scanning electronic microscope (ISI-SR-50, Akashi Seisakusho Co. Ltd., Japan). Photomicrographies of representative areas were obtained to evaluate the fracture pattern. This latter is classified in adhesive, cohesive (either in dentin or in cement) and/or mixed.
Results
ANOVA showed statistically significant differences among experimental groups, and Tukey's test (p < 0.05) identified the differences. Group 1 exhibited the highest bond strength mean; there is no statistically significant difference among the other groups (table II).
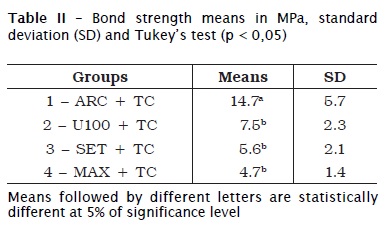
The specimens tested in group 1 (figure 2) exhibited predominately mixed failures, from cohesive in dentin to cohesive in cement. The other groups (figures 3 to 5) presented mainly adhesive failures.
Discussion
Dentin is a more heterogeneous and physiologically dynamic substrate than enamel. Garberoglio and Brännström (1976) 5 showed that the number and diameter of dentinal tubules increase with deepness. At superficial dentin, 96% of the area is occupied by intertubular dentin, 3% by peritubular dentin and only 1% by dentinal fluid. There is an inverse relationship, however, for the area closer to pulp, when 66% of the area is occupied by peritubular dentin, 12% by intertubular dentin and 22% by dentinal fluid. According to Swift Junior et al. (1995) 19, differences in composition and morphology in relation to deepness may directly influence the behavior and mechanical properties of dentin against chemical and physical agents to which dentin is submitted during the operative and restorative procedures, such as the application of resin cements.
In this present study, the focus was to evaluate the bond strength of self-adhesive resin cements in deep dentin, through microtensile methodology proposed by Sano et al. (1994) 17, by using hourglass specimens. This type of mechanical test solves problems related to tension propagations bonded to larger areas. Additionally, it presents the advantage that several specimens can be obtained from one sample (tooth), through the cut performed in a cutting machine (Isomet).
Traditionally, conventional cements demand the use of either conventional or self-etching adhesive systems 4. The technique sensibility and the difficulty of obtaining a hermetic sealing associated with conventional adhesive systems probably leads to a greater incidence of post-operative sensibility related to indirect restorations' luting procedure. Self-adhesive resin cements, however, did not demand tooth structure pre-treatment, therefore simplifying the clinical steps during the installation procedures of crowns/fixed partial dentures. Additional advantages of these products are the decrease or elimination of post-operative sensibility, as well as lesser susceptibility to moisture, according to Mazzitelli et al. (2008) 12.
Control group, which used conventional resin cement RelyX ARC, exhibited the highest bond strength mean with statistically difference relating to the other groups. We speculate that the bond mechanism involved in this product, which requires the previous application of 37% phosphoric acid and the application of the adhesive system Adper Single Bond 2 (3M ESPE), account for the statistical difference in comparison with the other groups (which did not show any difference among them). This adhesive system, classified as "two-steps / wet-bonding technique" by Van Meerbeek et al. (2003) 21, exhibits a mechanism of action that promotes greater micromechanical retention, because it results in a deeper demineralization of the substrate by the action of the phosphoric acid, which is posteriorly replaced by resin monomers.
The quality of the hybrid layer formed by using "wet-bonding technique", however, has been questioned by some authors 23,25, who still considered the complete sealing of dentin/resin interface a great challenge. Sano et al. (1995) 18 proposed the concept of nanoleakage, understood as a degradation phenomenon occurring at the interface, even without marginal failures in (direct or indirect) restorations. Nanoleakage would be explained by 1) resin monomers that do not effectively infiltrate at the same deepness of dentin etched by phosphoric acid, or 2) an area of increase permeability caused by an inferior curing due to excessive hydrophilicity of the current adhesive systems. Also, nanoleakage relates to long-term durability of the restorations 20.
In a recent literature review study, Moon et al. (2010) 14 cited other concept related to adhesive systems, which involve the metalloproteinase matrixes (MMPs). MMPs are a family of cells derived from a proteolytic enzyme with 26 identified members. Specific enzymes from this family may function beneficially during tissue remodeling or dentin mineralization. However, MMPs may act during inflammation and increase the side effects of periodontal disease and caries process, due to destruction of both collagen and other extracellular matrix proteins. Therefore they also may be released by (inorganic or organic) acids and activated by specific proteins or organic acids at oral environment or in the mechanism of action of the adhesive systems. More specifically, if collagen fibrils are left exposed and unprotected by resin monomers in hybrid layer, they could be degraded by MMPs activation. As time goes by, bond degradation may lead to the loss of retention or the decreasing in bond strength. This mainly occurs in conventional adhesive systems, although this phenomenon is also observed with other self-etching products. According to these authors, 2% chlorhexidine application onto the surface etched by phosphoric acid may prevent bond strength long-term decrease. In control group, the failures were predominantly mixed from cohesive in dentin to cohesive in resin cement, as shown by figure 2.
In this present study, there was no statistically significant difference in bond strength among self-adhesive resin cements. The three researched products contain similar acid monomers in their compositions, which presumably account for the mechanism of bonding. Currently, literature has reported controversial data on bond strength of these products. Two studies did not find statistical difference among the products, similarly to our study 11,22. On the other hand, other studies observed differences among the products and even in the same product, when different protocols and surface pre-treatments were executed 16.
Previous studies of Monticelli et al. (2008) 13 reported similar interfacial patterns produced by self-adhesive cements, without clear demineralization and/or infiltration of the products in dentin. This could also explain bond strength mean values of our study, which did not present statistical significant difference. The employed materials are self-etching and self-adhesive cements, which produce a slightly thick hybrid layer of difficult visualization. The methacrylate phosphoric acids ionized by the monomeric mixture are responsible for bonding to dentin, as well as the intermediary interfacial layer results in a particle layer incorporated to the smear layer, similarly to the action of glass ionomer cements 1.
By correlating the mechanism of action of these cements to that of glass ionomer cements, as cited by Yip et al. (2001) 24 and Hikita et al. (2007) 10, we speculate that the residual presence of self-adhesive cements on the fractured surfaces observed by scanning electronic microscopy suggests these materials' ability of bonding to the substrate. Two alternatives may explain this bonding. The first is that dentinal smear layer not modified by acid monomers creates an intermediary superficial layer rich in calcium and phosphate ions that may facilitate the chemical reaction with the methacrylate phosphoric acids of the cements. The second refers to the possibility of these acids have promoted (due to their pHs), even partially, a demineralization enough to create a layer rich in collagen, consequently allowing cements' penetration. Further studies are necessary to evaluate both hypotheses.
Conclusion
Self-adhesive resin cements showed lower bond strength mean than conventional resin cement RelyX ARC. The highest bond strength mean obtained by the conventional cement relates to its mechanism of action. However, the mechanism of action involved in self-adhesive cements seems to be effective for clinical use, if an adequate prosthetic dental preparation is observed.
Acknowledgments
This study (Project FAU2 from Univille) was partially supported by the cooperation program between University of Erlangen-Nuremberg (FAU), Erlangen, Germany (Dental Clinic 1, Operative Dentistry and Periodontology) and the University of the Region of Joinville (Univille), Joinville, Brazil (Department of Dentistry).
References
1. Al-Assaf K, Chakmakchi M, Palaghias G, Karanika-Kouma A, Eliades G. Interfacial characteristics of adhesive luting resins and composites with dentine. Dent Mater. 2007;23:829-39. [ Links ]
2. Costa CAS, Teixeira HM, Nascimento ABL, Hebling J. Biocompatibility of resin-based dental materials applied as liners in deep cavities prepared in human teeth. J Biomed Mater Res B Appl Biomater. 2007;81:175-84.
3. De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater. 2004;20:963-71.
4. Frankenberger R, Lohbauer U, Schaible RB, Nikolalenko SA, Naumann M. Luting of ceramic inlay in vitro: marginal quality of self-etch and etch-and-rinse adhesives versus self-etch cements. Dent Mater. 2008;24:185-91.
5. Garberoglio R, Brännström M. Scanning electron microscopic investigation of human dentinal tubules. Arch Oral Biol. 1976;21:355-62.
6. Garcia RN, de Goes MF, Giannini M. Effect of water storage on bond strength of self-etching adhesives to dentin. J Contemp Dent Pract. 2007 Nov;(8)7:46-53.
7. Gemalmaz D, Ergin S. Clinical evaluation of all-ceramic crowns. J Prosthetic Dent. 2002;87:189-96.
8. Goracci C, Cury AH, Cantoro A, Papacchini F, Tay FR, Ferrari M. Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J Adhes Dent. 2006;8:327-35.
9. Han L, Okamoto A, Fukushima M, Okiji T. Evaluation of physical properties and surface degradation of self-adhesive resin cements. Dent Mater J. 2007;26:906-14.
10. Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K, Maida T et al. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater. 2007;23:71-80.
11. Lührs AK, Guhr S, Günay H, Geurtsen W. Shear bond strength of self-etching resins compared to resin cements with etch and rinse adhesives to enamel and dentin in vitro. Clin Oral Investig. 2010;14:193-9.
12. Mazzitelli C, Monticelli F, Osorio R, Casucci A, Toledano M, Ferrari M. Effect of simulated pulpal pressure on self-adhesive cements bonding to dentin. Dent Mater. 2008;24:1156-63.
13. Monticelli F, Osorio R, Mazzitelli C, Ferrari M, Toledano M. Limited decalcification/diffusion of self-adhesive cements into dentin. J Dent Res. 2008;87:974-9.
14. Moon PC, Weaver J, Brooks CN. Review of matrix metalloproteinases' effect on the hybrid dentin bond layer stability and chlorhexidine clinical use to prevent bond failure. Open Dent J. 2010;4:147-52.
15. Nakabayashi N, Pashley DH. Hybridization of dental hard tissues. Tokyo: Quintessence; 1998. p. 16-89.
16. Pavan S, Santos PH, Berger S, Bedran-Russo AKB. The effect of dentin pretreatment on the microtensile bond strength of self-adhesive resin cements. J Prosthet Dent. 2010;104:258-64.
17. Sano H, Shono T, Sonoda H, Takatsu T, Ciucchi B, Carvalho RM. Relation between surface area for adhesion and tensile bond strength – evaluation of a microtensile bond test. Dent Mater. 1994 Jul;10(4):236-40.
18. Sano H, Takatsu T, Ciucchi B, Horner JA, Matthews WG, Pashley DH. Nanoleakage: leakage within the hybrid layer. Oper Dent. 1995 Jan-Feb;20(1):18-25.
19. Swift Junior EJ, Perdigão J, Heymann HO. Bonding to enamel and dentin: a brief history and state of the art. Quintessence Int. 1995;26(2):95-110.
20. Tay FR, Pashley DH. Water treeing – A potential mechanism for degradation of dentine adhesives. Am J Dent. 2003;16:6-12.
21. Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P et al. Adhesion to enamel and dentin: current status and future challenges. Oper Dent. 2003;28:215-35.
22. Viotti RG, Kasaz A, Pena CE, Alexandre RS, Arrais CA, Reis AF. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J Prosthet Dent. 2009;102:306-12.
23. Wang Y, Spencer P, Hager C, Bohaty B. Comparison of interfacial characteristics of adhesive bonding to superficial versus deep dentine using SEM and staining techniques. J Dent. 2006;34:26-34.
24. Yip HK, Tay FR, Ngo HC, Smalles RJ, Pashley DH. Bonding of contemporary glass ionomer cements to dentin. Dent Mater. 2001;17:456-70.
25. Yuan Y, Shimada Y, Ichinose S, Tagami J. Effect of dentin depth on hybridization quality using different bonding tactics in vivo. J Dent. 2007;35:664-72.
 Correspondence:
Correspondence:
Rubens Nazareno Garcia
Universidade da Região de Joinville – Univille – Departamento de Odontologia
Rua Paulo Malschitzki, n.° 10 – Zona Industrial – Bom Retiro
CEP 89219-710 – Joinville – SC – Brasil
E-mail: rubens.garcia@univille.net
Received for publication: March 12, 2011
Accepted for publication: April 27, 2011













