Serviços Personalizados
Artigo
Links relacionados
Compartilhar
RSBO (Online)
versão On-line ISSN 1984-5685
RSBO (Online) vol.8 no.4 Joinville Out./Dez. 2011
LITERATURE REVIEW ARTICLE
Root resorption after dental traumas: classification and clinical, radiographic and histologic aspects
Bruno Oliveira de Aguiar SantosI; Diego Santiago de MendonçaI; Denise Lins de SousaI; José Jeová Siebra Moreira NetoI; Rebeca Bastos Rocha de AraújoI
I Federal University of Ceara – Fortaleza – CE – Brazil
ABSTRACT
Introduction: One of the most common sequelae observed after dental trauma is root resorption. Objective: The aim of this study was to classify and discuss the external root resorption after a dental trauma, based on a literature review. Literature review: A bibliographic search was performed in the following databases: Medline, PubMed, and Lilacs, from 1997 to 2010. The following descriptors were used: Root resorption, Dental trauma and Classification. From a total of 152 articles found, 25 were selected: 24 in English and 1 in Spanish. Classic articles were also used in our study. External root resorption after dental traumas can be divided into superficial, inflammatory and replacement. It can also be verified in primary dentition as physiological and atypical resorptions. Conclusion: Each type of resorption presents clinical features as well as radiographic and histological aspects. Therefore, the dentist should know these characteristics to perform an early diagnosis and appropriate treatment, minimizing the sequelae related to this problem. Moreover, in primary dentition, the differential diagnosis between physiological and pathological resorption is important to avoid over-treatment.
Keywords: dental trauma; root resorption; classification.
Introduction
According to the International Association of Dental Traumatology, oral trauma comprises 5% of all traumatic injuries 11. The prevalence of trauma in this area is higher between 18 and 30 months of age due to lack of development of motor coordination and protective reflex, and, between 6-12 years of age, period in which children initiate sports activities 22.
After dental traumas, sequelae (root resorption, root canal obliteration, interruption in root formation, periapical lesion, and damages to permanent tooth buds) may be frequently observed in patient's follow-up appointments 6,7,18. Tooth mobility, crown discoloration, and sensitivity to percussion may also be reported as clinical sequelae of traumatized teeth. Therefore, follow-up radiographic examination of traumatized teeth plays an important role in the early diagnosis of these alterations 6.
Longitudinal studies show that root resorption prevalence is very high (8-50%) after tooth trauma 4,5,10,13,20, so that a standard classification is mandatory for their diagnosis and treatment.
The aim of this study was to classify and discuss external root resorptions after dental traumas, based on a literature review, emphasizing the importance of an early diagnosis and adequate treatment.
Literature review
Root resorption is defined as either a physiologic or pathological event mainly occurring due to the action of activated clasts; it is characterized by the progressive or transitory loss of cementum or cementum/dentin 19. It is a strictly local process and its onset is associated with a significant necrosis of cementoblasts and/or injury to periodontal ligament 8,10.
Root resorptions occurrence may be induced by traumatic and/or infectious factors. Dental trauma is an important etiological factor of resorptions, although these may also occur due to a chronic inflammatory process of pulp and/or periodontal tissue; also, root resorptions may be induced by tooth eruption, impacted teeth, occlusal trauma, pathological tissues (cysts or neoplasias), and by the pressure exert by extreme orthodontic tooth movement 2,12,14. Root resorptions may also be of idiopathic origin, although less frequent 9,15.
Dental trauma can promote cementoblasts necrosis either directly (when the traumatic impact causes direct cellular crushing) or indirectly (when trauma compromises the neurovascular bundle which nurture periodontal tissues and tooth pulp). As far as pulp is concerned, the lack of blood supply results in pulp necrosis due to coagulation. Following, the tooth defense mechanisms are also affected and the tooth can be easily infected by microorganisms, inducing and propagating root resorption of inflammatory nature. Infection may occur through dentinal tubules that are exposed to oral cavity, through gingival sulcus and micro- and macro-fissures of enamel appearing from trauma or pulp contamination through anchoritic via 2,10.
Dentin, cementum, and bone are mineralized hard tissues. However, while bone is continuously remodeling by resorption/neoformation during life, tooth's hard tissues are not. Therefore, periodontal ligament interposition between bone and root is an important factor for root protection against resorption 19.
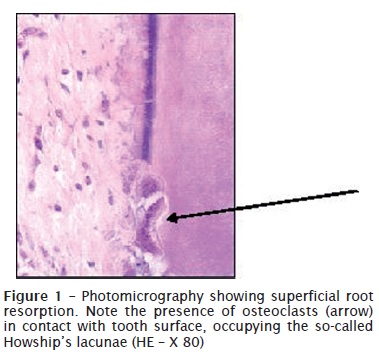
External root surface hard tissues are protected by pre-cementum, cementoblasts, and epithelial rests of Malassez. If these tissues are mechanically damaged or fragmented, a chemotactic process will attract the activated clasts which will colonized the affected or exposed surface, initiating the resorption process. Cementoclasts or osteoclasts are present in the interface between soft (periodontal ligament) and hard tissue (cementum), at depressions in the calcified matrix. Such depressions are areas occurring from the reabsorption process itself, so-called Howship's lacunae (figure 1) 10.
Due to the complexity of root resorptions' etiological factors, it is difficult to establish a standard classification in literature. Several studies were conducted to standardize the different types of resorption 1,2,7,12,15,19,28.
Andreasen 1 has greatly contributed to the understanding of root resorptions during 40 years. This author creates a classification, largely used until today, which divided resorptions into internal (replacement and inflammatory) and external (superficial, replacement, and inflammatory).
Gunraj 14 classifies root resorption in: internal; external (superficial, inflammatory, and replacement) associated with traumatic injuries; external due to pulp necrosis and periradicular lesion; external due to pressure on periodontal ligament (tumors, cysts, orthodontic treatment, impacted teeth); and cervical.
Benítez et al. 3 classified root resorptions according to their localization, into internal dentinal resorptions and external cementum/dentin resorptions; according to etiology into physical factors (traumas and tooth pressure), infectious agents (from pulp cavity or periodontium), systemic or from idiopathic cause infections.
Fuss et al. 12 proposed the diagnosis, classification, and the treatment of choice of root resorptions based on stimulation factors. These can be: pulp infection, periodontal infection, orthodontic pressure, ankylosis, and tumoral or impacted tooth pressure. These authors affirmed that the most common stimulation factor of root resorption is pulp infection.
Heithersey 15 classifies dental resorptions into three groups: induced by trauma, induced by infection and hyperplasic invasive.
Patel et al. 24 divided root resorptions regarding their localization of root surface into internal and external (superficial, inflammatory, replacement, cervical and apical transitory).
Yilmaz et al. 29 characterized cervical resorption as a clinical term used for describing an insidious, relatively uncommon, frequently aggressive external root resorption. Internal bleaching, orthodontic movement, traumatic injuries, orthognathic surgery and periodontal treatment account for this resorption type predisposing factors. Different techniques have been described for this resorption type, among them, guided tissue regeneration (GTR).
It is a literature consensus that root resorptions after traumatic injuries are classified as external and they may be divided into: superficial, inflammatory and replacement 2,7,12,14,15,19. Lopes and Siqueira Jr. 19 still classified inflammatory root resorption, according to the area affected, into: apical, lateral, and cervical. Kramer and Feldens 17 reported the atypical resorption in primary dentition. Hereafter, we will show the clinical, radiographic, and histological aspects as well as the diagnosis and treatment of these types of external resorptions.
Superficial root resorption
When small inflammatory changes occur, new periodontal ligament and cementum are formed only after one week post-trauma, characterizing a superficial resorption 14. Consequently, this represents a transitory, self-limiting inflammatory process, in which the body is capable of stopping the resorption and inactivating the activated clasts, i.e., the repair is spontaneous. Superficial resorption can be classified as a transitory inflammatory root resorption because due to lack of stimulus to maintain their action, clastic cells stop their resorptive activity and periodontal ligament cells promote the area repair. Concerning to its characteristics, it can be affirmed:
• The etiology is traumatic lesions of low intensity in tooth's support tissues, e.g. subluxation and concussion;
• During tooth's clinical examination, there is no indicative sign of this resorption;
• Radiographically a normal lamina dura is observed, as well as small excavations on tooth surface;
• Histologically, resorption cavities are seen reaching cementum and dentin, as well as the presence of multinucleated giant cells so-called osteoclasts (figure 1);
• Since the repair is spontaneous, no treatment is necessary 8,14,15.
Replacement root resorption
Replacement or substitutive root resorption is characterized by direct connection between alveolar bone and tooth, a phenomenon so-called dental ankylosis. The resorption occurs due to the lack of vital periodontal ligament and bone remodeling, during which osteoclastic activity causes tooth resorption while osteoblastic activity creates a new bone in the resorbed area. Since bone remodeling is a physiologic phenomenon, the maintenance factors represented by the calcitonin and parathyroid hormones cannot be removed 19. Concerning to its features, it can be affirmed:
• Its etiology is any dental trauma capable of provoke an irreversible damage to periodontal ligament, resulting in dental ankylosis, e.g., avulsion followed by delayed replantation of avulsed teeth;
• Radiographically, the tooth presents no symptoms, without physiologic or pathologic mobility; and metallic sound in response to vertical percussion, which can be diagnosed even before radiographic evidences. Commonly, the tooth is in infraocclusion 15,26.
• Replacement resorption is greatly related to age; the younger the patient, the greater the resorption rate. There is a high risk of infraocclusion when ankylosis is diagnosed either before 10 years of age or prior to the individual's peak of growth. However, patients aging 20 years or more, root resorption rate is slower, and the tooth can survive 20 years or more. In patients aging from 7 to 16 years, tooth loss occurs from 3 to 7 years after the resorption onset; consequently, a long-term treatment planning is important for the replacement of teeth presenting this type of pathology to avoid greater damages 15,26;
• Histologically, bone trabeculae are in direct contact with tooth root (figure 3);
• Replacement resorption is an irreversible process; there is no treatment for its interruption 10,12,15,17,26.
Because there is no etiological factor to be removed, no treatment can be performed 12,15. The prevention to minimize the damage to the periodontal ligament after trauma is the only treatment 12. When only the epithelial insertion holds the tooth, or there is alteration of the rizolysis process and permanent tooth delay or ectopic eruption, primary tooth extraction is indicated 17.
Rarely, a cementum layer may act as a biological barrier and ankylosis is not followed by replacement resorption 15.
Hidalgo et al. 16 reported the relationship of replacement resorption due to trauma with patient's humoral immunological profile, concluding that dentin exhibits a immunogenic potential and that these patient's serum presents a higher amount of IgG and smaller amount of IgM, both specific for human dentin, when compared to control patients 22.

Inflammatory root resorption
External inflammatory resorption is a progressive inflammatory process and the main factor accounting for its maintenance is pulp necrosis. The presence of either pulp necrotic rests or bacteria within dentinal tubules attracts a large number of osteoclasts for the area. Consequently, resorption advances continuously up to root canal be exposed. It is necessary the clinician intervention to stop the process through elimination or reduction of the maintenance factor 12. Concerning its characteristics, it can be affirmed:
• Its etiology is traumatic lesions of great intensity localized in tooth's support tissues, e.g., lateral luxation, intrusion and avulsion;
• Clinically, the tooth does not respond to vitality tests. Tooth crown color can be altered to grey. Tooth can present pain to vertical or horizontal percussion, depending on the area in which resorptive process is installed (apical or lateral, respectively);
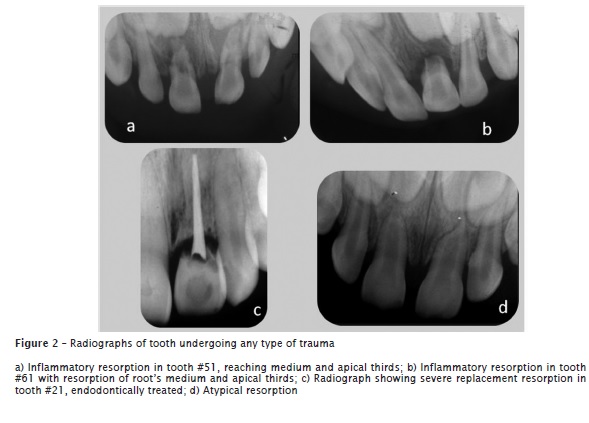
• Radiographically, it is seen a radiolucency at periapical area associated with root resorption (figures 2a and 2b). Concerning to its localization, it can be classified as apical, lateral, or cervical;
• Histologically, saucer-shape resorption areas are observed, involving both cementum and dentin; also inflammation of adjacent periodontal ligament and bone resorption occurs (figure 4). It may quickly occur in young teeth because dentinal tubules are larger and allow that irritants move freely through root's external surface 28.
Chronic inflammation represents an indicative of the necessity of endodontic treatment whose goal is to promote bacterial disinfection of the affected area 10,12,15.
When inflammatory resorption is detected, calcium hydroxide is considered the intracanal medication of choice. The mechanism by which calcium hydroxide promotes tissue repair is not known, but success rates of 97% have been reported when this method is used 2.

Atypical resorption
In primary dentition, atypical external root resorption can be diagnosed during follow-up appointments of patients undergoing dental trauma. This is not associated with pulp necrosis and is characterized by tissue loss surrounding all root circumference, normally involving root's apical and medium thirds. However, there is the maintenance of periodontal ligament space and lack of both dental ankylosis and periapical radiolucency. The tooth is normally asymptomatic up to its rizolysis 17.
Atypical resorption is also known as dome-shape or cone-shape resorption due to its radiographic aspect, in which there is loss of root tissue and bone tissue growth compensating the resorbed area and sound periodontal ligament (figure 2d). It seems to be associated with thumb sucking and upper incisors overjet, which resulting in constant traumas of low intensity. It is self-limiting because there is spontaneous repair of cementum and periodontal ligament; consequently it does not demand any treatment and its prognosis is favorable 26.
Discussion
Depending on the trauma type, there is a greater or smaller risk of root resorption development; tooth traumas mostly associated with resorption are intrusive luxation, lateral luxation, and avulsion followed by replantation 2,10,26.
Finucane and Kinirons 10 affirmed that root resorption following extrusive luxation is rare: the prevalence of inflammatory resorption is approximately 5%, particularly when the tooth is repositioned within 90 minutes after the avulsion. In teeth replanted after avulsion, however, root resorption is common, with prevalence of 50-80%.
The maintenance of avulsed teeth in proper storage media is primordial for periodontal ligament repair and root resorption prevention after replantation. Milk is the storage media mostly indicated when immediate replantation is not possible, making viable periodontal ligament's cells for up to 6 hours. Studies have been performed to find a storage media which increases the chances of periodontal repair and inhibits the occurrence of root resorption 21,23,27.
Pissiotis et al. 25 affirmed that multiple dental traumatic episodes (MDTE) in permanent dentition increase the risk of certain complications, such as replacement and inflammatory resorption.
The trauma recurrence on the same tooth is a factor associated with pathological root resorption development. The identification of two (age above 18 months and complicated trauma or age above 18 months and recurrent trauma) or three factors (age above 18 months, complicated trauma, and recurrent trauma) at the same tooth increases the chance of pathological resorption in primary dentition 6.
Finally, as far as primary dentition is concerned, differential diagnosis between physiologic (or rizolysis) and pathological resorption is important. Among permanent tooth components, tooth bud and stellate reticulum plays an important role in primary tooth's root resorption. The pressure of permanent tooth eruption plays a contributory role in rizolysis, but the presence of the permanent successor tooth is not a pre-requisite for the process occurrence 8. Therefore, the radiographic difference between physiologic and pathologic resorptions is that in the first, it is normally observed a continuity between primary and permanent tooth while in the second there is no indicative of permanent tooth causing resorption in primary tooth's root. Additionally, rizolysis progression is symmetrical and uniform while pathological resorption exhibits an irregular aspect.
The cells responsible for rizolysis are multinucleated giant cells with characteristics similar to osteoclasts, so-called odontoclasts. Odontoclasts are aided by mononuclear phagocytic cells, such as fibroblasts, cementoclasts, and macrophages. These cells are actively involved in the removal of tooth's hard and soft tissues during primary tooth exfoliation. Cementoblasts, not odontoclasts, account for the phagocytosis of tooth surface's collagen fibrils; odontoclasts would be responsible for dentinal demineralization and degradation of the non-collagen matrix 8,9.
Conclusion
External root resorptions are very prevalent sequelae after tooth traumas. The knowledge of the resorptions' classification, clinical, radiographic, and histologic aspects is important for the early diagnosis, treatment planning elaboration and prognosis.
References
1. Andreasen JO. Luxation of permanent teeth due to trauma. A clinical and radiographic follow-up study of 189 injured teeth. Scand J Dental Res. 1970;78(3):273-86. [ Links ]
2. Andreasen JO, Andreasen FM. Traumatismo dentário: soluções clínicas. São Paulo: Panamericana; 1991.
3. Benítez MB, Chiera CM, Jacobo MI. Reabsorciones dentarias: un problema para el diagnóstico, el tratamiento y el pronóstico. Claves Odontol. 2002;8(50):10-3.
4. Borum MK, Andreasen JO. Sequelae of trauma to primary maxillary incisors. I. Complications in the primary dentition. Endod Dent Traumatol. 1998 Feb;14(1):31-44.
5. Cardoso M, Rocha MJC. Federal University of Santa Catarina follow-up management routine for traumatized primary teeth – part 1. Dent Traumatol. 2004 Dec;20(6):307-13.
6. Cardoso M, Rocha MJC. Identification of factors associated with pathological root resorption in traumatized primary teeth. Dental Traumatol. 2008 Jun;24(3):343-9.
7. Cohenca N, Simon JH, Mathur A, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 2: root resorption. Dental Traumatol. 2007 Apr;23(1):105-13.
8. Consolaro A. Reabsorções dentárias nas especialidades clínicas. 2. ed. Maringá: Dental Press; 2005.
9. Evlambia HH. Physiologic root resorption in primary teeth: molecular and histological events. J Oral Sci. 2007 Mar;49(1):1-12.
10. Finucane D, Kinirons MJ. External inflammatory and replacement resorption of luxated, and avulsed replanted permanent incisors: a review and case presentation. Dent Traumatol. 2003 Jun;19(3):170-4.
11. Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F et al. Guidelines for the management of traumatic dental injuries. II. Avulsion of permanent teeth. Guidelines for the management of traumatic injuries in the primary dentition. Dent Traumatol. 2007 Jun;23(3):130-6.
12. Fuss Z, Tsesis I, Lin S. Root resorption – diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003 Aug;19(4):175-82.
13. Gondim JO, Moreira Neto JJS. Evaluation of intruded primary incisors. Dent Traumatol. 2005 Jun;21(3):131-3.
14. Gunraj MN. Dental root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 Dec;88(6):647-53.
15. Heithersay GS. Management of tooth resorption. Aust Dent J. 2007 Mar;52(1 Suppl):S105-21.
16. Hidalgo MM, Itano EN, Consolaro A. Humoral immune response of patients with dental trauma and consequent replacement resorption. Dent Traumatol. 2005 Aug;21(4):218-21.
17. Kramer PF, Feldens CA. Traumatismos na dentição decídua. Prevenção, diagnóstico e tratamento. 1. ed. São Paulo: Santos; 2005.
18. Lenzi AR, Medeiros PJ. Severe sequelae of acute dental trauma in the primary dentition – a case report. Dent Traumatol. 2006 Dec;22(6):334-6.
19. Lopes HP, Siqueira Jr JF. Endodontia. Biologia e técnica. 2. ed. Rio de Janeiro: Guanabara Koogan/Medsi; 2004.
20. Majorana A, Bardellini E, Conti G, Keller E, Pasini S. Root resorption in dental trauma: 45 cases followed for 5 years. Dent Traumatol. 2003 Oct;19(5):262-5.
21. Martin MP, Pileggi R. A quantitative analysis of Propolis: a promising new storage media following avulsion. Dent Traumatol. 2004 Apr;20(2):85-9.
22. Moreira Neto JJS, Gondim JO. Traumatismo dentário – protocolo de atendimento. 1. ed. Fortaleza: Pouchin Ramos; 2007.
23. Mori GG, Nunes DC, Castilho LR, Moraes IG, Poi WR. Propolis as storage media for avulsed teeth: microscopic and morphometric analysis in rats. Dent Traumatol. 2010 Feb;26(1):80-5.
24. Patel S, Kanagasingam S, Pitt Ford T. External cervical resorption: a review. J Endod. 2009 May;35(5):616-25.
25. Pissiotis A, Vanderas AP, Papagiannoulis L. Longitudinal study on types of injury, complications and treatment in permanent traumatized teeth with single and multiple dental trauma episodes. Dent Traumatol. 2007 Aug;23(4):222-5.
26. Sapir S, Shapira J. Decoronation for the management of an ankylosed young permanent tooth. Dent Traumatol. 2008 Feb;24(1):131-5.
27. Sigalas E, Regan JD, Kramer PR, Whiterspoon DE, Opperman LA. Survival of human periodontal ligament cells in media proposed for transport of avulsed teeth. Dent Traumatol. 2004 Feb;20(1):21-8.
28. Trope M. Clinical management of the avulsed tooth: present strategies and future directions. Dental Traumatol. 2002 Feb;18(1):1-11.
29. Yilmaz HG, Kalender A, Cengiz E. Use of mineral trioxide aggregate in the treatment of invasive cervical resorption: a case report. J Endod. 2010 Jan;36(1):160-3.
 Correspondence:
Correspondence:
Diego Santiago de Mendonça
Rua Marechal Deodoro, n.º 1.395 – ap. 218
CEP 60020-060 – Fortaleza – CE – Brasil
E-mail: santiagoufc@gmail.com
Received for publication: February 25, 2010
Accepted for publication: May 17, 2010













